Syncope resident survival guide: Difference between revisions
| Line 73: | Line 73: | ||
</table> | </table> | ||
----- | ----- | ||
''' | '''Obtain a detailed past medical history:'''<br> | ||
❑ Previously healthy <br> | ❑ Previously healthy <br> | ||
❑ Previous syncope episodes <br> | ❑ Previous syncope episodes <br> | ||
Revision as of 15:43, 19 March 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Karol Gema Hernandez, M.D. [2]; Alejandro Lemor, M.D. [3]
| Syncope Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Click here to go back to the resident survival guide home page.
Overview
Syncope is the transient loss of consciousness (LOC) due to cerebral hypoperfusion and it is characterized by a rapid onset, a short duration and a spontaneous complete recovery. It is extremely important to identify the cause of the syncope and recognize high risk patients (order a EKG to look for heart disease as a possible cause). The initial management would depend on the etiology of the syncope(reflex, orthostatic hypotension or cardiovascular).
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Arrhythmia
- Medication (vasodilators, diuretics, antiarrhythmics, antipsychotics)
- Orthostatic hypotension
- Vagal stimulation
- Vertebrobasilar insufficiency[2]
Diagnosis
Shown below is an algorithm summarizing the diagnostic approach to syncope based on the 2009 ESC Guidelines for the Diagnosis and Management of Syncope. [3]
Abbreviations: TIA:Transient ischemic attack; EEG:Electroencephalography; HF: Heart failure; AF: Atrial fibrillation: SVT: Supraventricular tachycardia ; VT:Ventricular tachycardia: MI: Myocardial infarction; BBB: Bundle branch block
Characterize symptoms ❑ Loss of consciousness (LOC)
❑ Prodrome (diaphoresis, nausea, blurry vision)
Inquire about medications intake:
Obtain a detailed past medical history: | ||||||||||||||||||||||||||||||||||||||||||
Identify possible triggers:
| ||||||||||||||||||||||||||||||||||||||||||
❑ Examine the patient
| ||||||||||||||||||||||||||||||||||||||||||
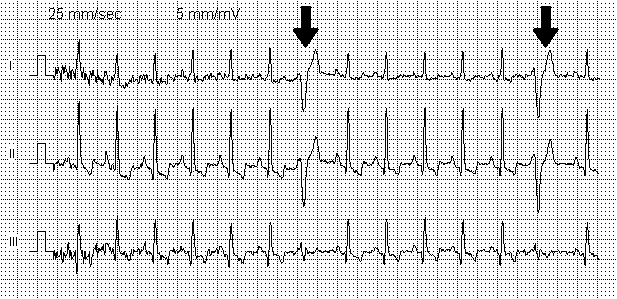
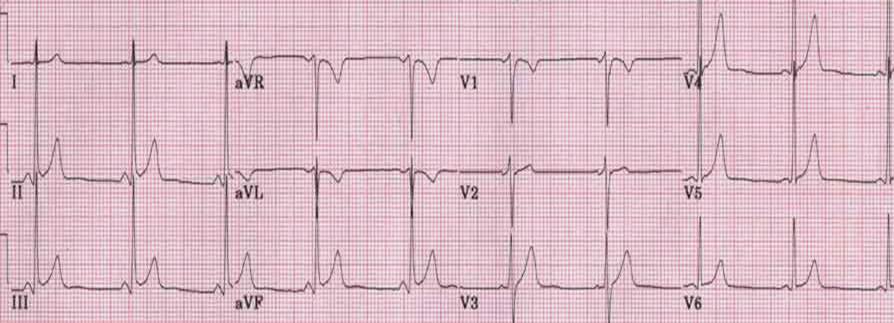
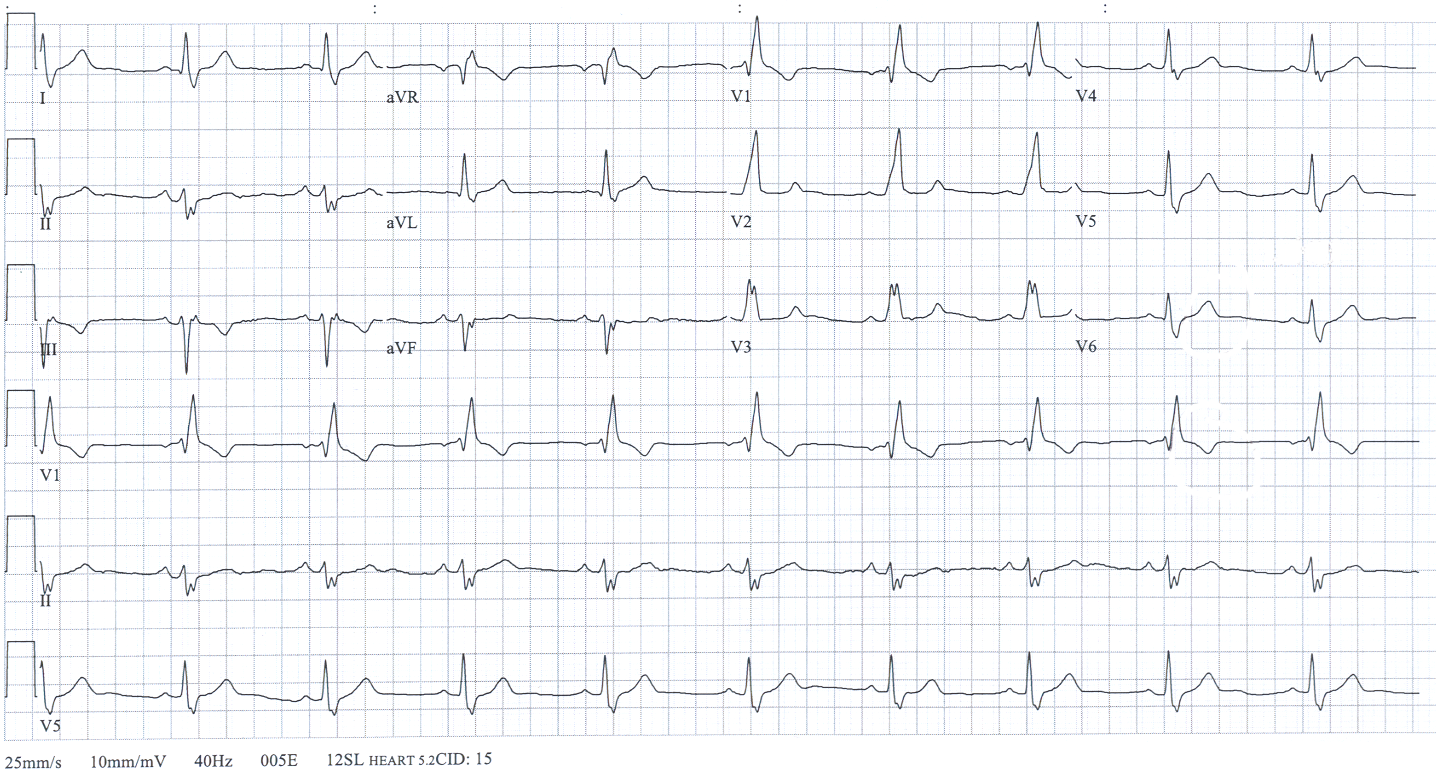
❑ Order an EKG ❑ Order a stool guaiac test (to look for GI bleeding) ❑ Order electrolytes, glucose, ABG) (search for metabolic disorders: hypoglycemia, hyponatreamia, hypernatremia, hypokalemia, hypoxia) ❑ Order blood and urine toxicology tests (if intoxication is suspected) | ||||||||||||||||||||||||||||||||||||||||||
Rule out other possible diagnoses:
With loss of consciousness:
❑ Metabolic disorders (order electrolytes, glucose, ABG):
❑ Intoxication Without loss of consciousness: ❑ Cataplexy ❑ Drop attacks ❑ Functional /psychogenic pseudosyncope (patients with conversion disorder) ❑ TIA | ||||||||||||||||||||||||||||||||||||||||||
❑ Determine the etiology of the syncope | ||||||||||||||||||||||||||||||||||||||||||
Reflex | Orthostatic hypotension | Cardiovascular | ||||||||||||||||||||||||||||||||||||||||
Findings: ❑ Heart rate: tachycardia, normal or bradycardia ❑ Absence of heart disease ❑ History of recurrent syncope ❑ After unpleasant sight or odor ❑ Associated to nausea ❑ Head rotation or pressure to carotid sinus ❑ Neurological system: look for focal neurologic signs ❑ EKG: tachycardia, normal or bradycardia | Findings: ❑ Blood pressure (BP):
❑ Cardiac evaluation: palpitations ❑ After standing up or prolonged standing ❑ Start of new antihypertensive drug ❑ Presence of autonomic neuropathy ❑ EKG: tachycardia or normal | Findings: ❑ Heart rate:
❑ Cardiac evaluation: palpitations, carotid bruits, murmurs (search for aortic stenosis or pulmonary stenosis)
| ||||||||||||||||||||||||||||||||||||||||
Management
Shown below is an algorithm summarizing the therapeutic approach to syncope based on the 2009 ESC Guidelines for the Diagnosis and Management of Syncope. [3]
Abbreviations: AF: Atrial fibrillation: SVT: Supraventricular tachycardia ; VT:Ventricular tachycardia: MI: Myocardial infarction; BBB: Bundle branch block
| ❑ Determine the etiology of the syncope | |||||||||||||||||||||||||||
Reflex | Cardiovascular | ||||||||||||||||||||||||||
❑ Explain diagnosis, provide reassurance ❑ Explain risk of recurrence and avoidance of triggers ❑ Isometric physical counterpressure maneuvers (PCM) in patients with prodrome:
| ❑ Adequate hydration and salt intake ❑ Adjunctive therapy if needed: | Depends on the cause of the arrhythmia: ❑ Schedule for cardiac pacing: patients with sinus node disease, Mobitz II AV block, BBB with positive electrophysiological study ❑ Schedule for catheter ablation: patients with SVT and VT in absence of structural hearth disease ❑ Administer antiarrhythmic drug therapy: patients with AF, failed catheter ablation ❑ Schedule for implantable cardioverter defibrillator: patients with VT with heart disease, electrophysiological study induced VT in patients with previous MI, VT and inherited cardiomyopathy | |||||||||||||||||||||||||
Do's
- Tilt testing is indicated when it is of clinical value to demonstrate susceptibility to reflex syncope to the patient.
- Tilt testing should be considered to discriminate between reflex and OH syncope.
- Perform tilt testing if psychiatric disease.
- Tilt testing may be considered for differentiating syncope with jerking movements from epilepsy.
- If syncope happened after standing up position, there should be documentation with active standing or tilt testing in order to diagnose orthostatic hypotension.
- Perform carotid sinus massage if patient >40 years with syncope of unknown etiology after initial evaluation.
- If multiple unexplained falls; perform tilt testing.
- Consider implantable loop recorder before embarking on cardiac pacing in patients with suspected or certain reflex syncope presenting with frequent or traumatic syncopal episodes.
- Evaluate neurologically if syncope is due to autonomic failure, to evaluate underlying disease.
Don'ts
- Don't perform carotid sinus massage in patients with previous TIA or stroke within the past 3 months and in patients with carotid sinus bruits (except if carotid sinus Doppler studies excluded significant stenosis.
- Don't use tilt testing for assessment of treatment.
- Don't perform isoproterenol tilt testing in patients with ischemic heart disease.
- Don't use adenosine stress test as a diagnostic test to select patients for cardiac pacing, owing to lack of correlation with spontaneous syncope.
- Don't perform electrophysiologic study if there is already indication for ICD in patients with ischemic heart with suspected arrhythmic cause.
- Don't perform electrophysiologic study in patients with normal EKG, no heart disease, and no palpitations.
References
- ↑ Khoo, C.; Chakrabarti, S.; Arbour, L.; Krahn, AD. (2013). "Recognizing life-threatening causes of syncope". Cardiol Clin. 31 (1): 51–66. doi:10.1016/j.ccl.2012.10.005. PMID 23217687. Unknown parameter
|month=ignored (help) - ↑ Kapoor, WN. (2000). "Syncope". N Engl J Med. 343 (25): 1856–62. doi:10.1056/NEJM200012213432507. PMID 11117979. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 Task Force for the Diagnosis and Management of Syncope. European Society of Cardiology (ESC). European Heart Rhythm Association (EHRA). Heart Failure Association (HFA). Heart Rhythm Society (HRS). Moya A; et al. (2009). "Guidelines for the diagnosis and management of syncope (version 2009)". Eur Heart J. 30 (21): 2631–71. doi:10.1093/eurheartj/ehp298. PMC 3295536. PMID 19713422 Check
|pmid=value (help).