Congestive heart failure chronic pharmacotherapy: Difference between revisions
| Line 24: | Line 24: | ||
==A General Strategy in the Chronic Treatment of Heart Fialure== | ==A General Strategy in the Chronic Treatment of Heart Fialure== | ||
* '''First''', begin by rapidly improving the symptoms of heart failure (within hours to days) by the use of [[diuretics]]. [[Diuretics]] reduce excess volume that accumulates with [[heart failure]] and decrease [[pulmonary edema]] that causes symptoms of [[dyspnea]] and [[orthopnea]]<ref name="pmid20653715">{{cite journal| author=Michael Felker G| title=Diuretic management in heart failure. | journal=Congest Heart Fail | year= 2010 | volume= 16 Suppl 1 | issue= | pages= S68-72 | pmid=20653715 | doi=10.1111/j.1751-7133.2010.00172.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20653715 }} </ref>. [[Lasix]] 20 to 40 mg PO daily is a conventional starting dose, but in some patients, [[torsemide]] may have better and more predictable absorption. | * '''First''', begin by rapidly improving the symptoms of heart failure (within hours to days) by the use of [[diuretics]]. [[Diuretics]] reduce excess volume that accumulates with [[heart failure]] and decrease [[pulmonary edema]] that causes symptoms of [[dyspnea]] and [[orthopnea]]<ref name="pmid20653715">{{cite journal| author=Michael Felker G| title=Diuretic management in heart failure. | journal=Congest Heart Fail | year= 2010 | volume= 16 Suppl 1 | issue= | pages= S68-72 | pmid=20653715 | doi=10.1111/j.1751-7133.2010.00172.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20653715 }} </ref>. [[Lasix]] 20 to 40 mg PO daily is a conventional starting dose, but in some patients, [[torsemide]] may have better and more predictable absorption. Once a day dosing of a givne diuretic is preferred to twice a day dosing at a lower dose. | ||
:*'''Simultaneous with number 1''' | :*'''Simultaneous with number 1''' | ||
::*[[Congestive heart failure treatment of underlying causes|Treat the underlying cause of heart failure]] such as [[ischemic heart disease]], [[hypertension]], and [[valvular heart disease]]. | ::*[[Congestive heart failure treatment of underlying causes|Treat the underlying cause of heart failure]] such as [[ischemic heart disease]], [[hypertension]], and [[valvular heart disease]]. | ||
Revision as of 17:59, 27 April 2013
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Assistant editor-in-chief Rim Halaby
Overview
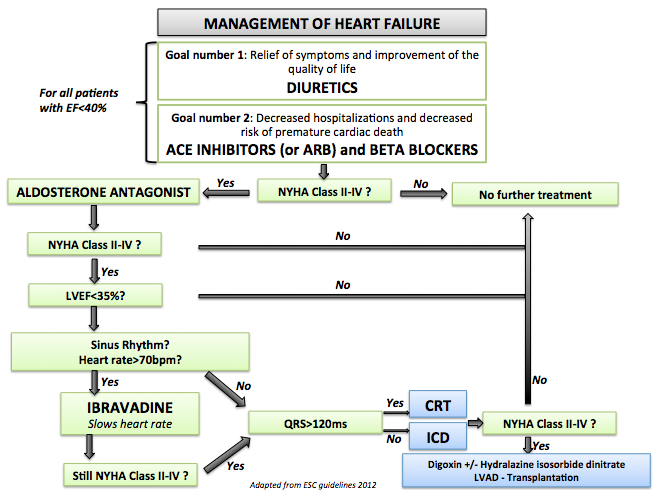
There are several goals in the chronic management of systolic heart failure. The management of diastolic heart failure is discussed elsewhere. The first goal is to treat the patient's symptoms of heart failure and to improve the patient's exercise tolerance and quality of life. The use of diuretics and regular assessment of the patient's weight helps in avoiding excess body fluids that are associated with dyspnea and orthopnea. Another goal of the chronic treatment of heart failure is to decrease the rate of hospitalization and mortality. To cheat the second goal, patients with chronic heart failure should be administered an ACE inhibitor (or ARB if they are ACE intolerant) and a beta blocker. If the patient remains symptomatic, additional therapy may be advised.
Chronic Pharmacotherapy
Treatment Goals
Improvement of symptoms:
Decreased Mortality:
- ACE inhibitors
- ARBs
- Beta blockers
- Diuretics (in meta-analyses) [1]
- Nitrates and hydralazine
- Spironolactone[2]
A General Strategy in the Chronic Treatment of Heart Fialure
- First, begin by rapidly improving the symptoms of heart failure (within hours to days) by the use of diuretics. Diuretics reduce excess volume that accumulates with heart failure and decrease pulmonary edema that causes symptoms of dyspnea and orthopnea[3]. Lasix 20 to 40 mg PO daily is a conventional starting dose, but in some patients, torsemide may have better and more predictable absorption. Once a day dosing of a givne diuretic is preferred to twice a day dosing at a lower dose.
- Simultaneous with number 1
- Treat the underlying cause of heart failure such as ischemic heart disease, hypertension, and valvular heart disease.
- Treat other non cardiac diseases that might contribute to the symptoms of heart failure such as diabetes and hyperthyroidism[4].
- Treat with a low salt diet[5]
- Follow the patient's weight to check for fluid overload
- Treat with vaccines for influenza and pneumococcus [6].
- Second, after diuretics are started or at the same time you can begin the use of an ACE inhibitors [7]. An example would be to start lisinopril 5 mg Q day. Every one to two weeks, the dose would be escalated to achieve a target dose of 15 to 20 mg Q day. ACE inhibitors are initiated before a beta blocker because they achieved their hemodynamic effects more rapidly, and they are less likely to cause a decline in hemodynamic function. If an ACE inhibitor is not tolerated, then an angiotensin receptor blocker ARB is started.
- Third, once you have achieved a stable dose of a diuretic and an ACE inhibitor, then a beta blocker can be added and the dose titrated based upon the patient's tolerance.
- Fourth, the combination of hydralazine and a nitrate (particularly among black patients) can be added if the patient continues to have symptoms on an ACE inhibitor and a beta blocker.
- Shown below is an image that summarizes the steps in the chronic management of patients with heart failure.
References
- ↑ Faris R, Flather MD, Purcell H, Poole-Wilson PA, Coats AJ (2006). "Diuretics for heart failure". Cochrane Database of Systematic Reviews (Online) (1): CD003838. doi:10.1002/14651858.CD003838.pub2. PMID 16437464. Retrieved 2013-04-27.
- ↑ Davies MK, Gibbs CR, Lip GY (2000). "ABC of heart failure. Management: diuretics, ACE inhibitors, and nitrates". BMJ. 320 (7232): 428–31. PMC 1117548. PMID 10669450.
- ↑ Michael Felker G (2010). "Diuretic management in heart failure". Congest Heart Fail. 16 Suppl 1: S68–72. doi:10.1111/j.1751-7133.2010.00172.x. PMID 20653715.
- ↑ DeGroot WJ, Leonard JJ (1970). "Hyperthyroidism as a high cardiac output state". Am Heart J. 79 (2): 265–75. PMID 4903771.
- ↑ Evangelista LS, Shinnick MA (2008). "What do we know about adherence and self-care?". J Cardiovasc Nurs. 23 (3): 250–7. doi:10.1097/01.JCN.0000317428.98844.4d. PMC 2880251. PMID 18437067.
- ↑ Martins Wde A, Ribeiro MD, Oliveira LB, Barros Lda S, Jorge AC, Santos CM; et al. (2011). "Influenza and pneumococcal vaccination in heart failure: a little applied recommendation". Arq Bras Cardiol. 96 (3): 240–5. PMID 21271169.
- ↑ Shiokawa Y (1975). "Proceedings: Streptococcus surveys in Ryukyu Islands, Japan". Jpn Circ J. 39 (2): 168–71. PMID 1117548.