Brugada syndrome overview: Difference between revisions
| Line 83: | Line 83: | ||
The EKG changes of Brugada syndrome can vary over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the [[ST segment]] elevation, while [[vagal stimulation]] worsens it. During sleep, there is [[heightened vagal tone]], and the pattern may be exacerbated at that time (as is the risk of [[sudden cardiac death]] at that time). The administration of class Ia, Ic and III drugs increases the [[ST segment]] elevation, as does [[fever]]. The impact of exercise depends upon when the EKG is obtained: during exercise the [[ST segment]] elevation may decrease but may increase later after exercise when the body temperature has risen. Similar to [[early repolarization variant]], when the heart rate decreases, the [[ST segment]] elevation increases and when the heart rate increases the [[ST segment]] elevation decreases. While Brugada syndrome is often associated with polymorphic VT which may be self terminating, in the presence of autonomic imbalance, hypokalemia, fever or exacerbating drugs sustained ventricular fibrillation and sudden cardiac death may result.<ref name="pmid15898165">{{cite journal |author=Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A |title=Brugada syndrome: report of the second consensus conference |journal=[[Heart Rhythm : the Official Journal of the Heart Rhythm Society]] |volume=2 |issue=4 |pages=429–40 |year=2005 |month=April |pmid=15898165 |doi= |url= |issn= |accessdate=2012-10-14}}</ref> | The EKG changes of Brugada syndrome can vary over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the [[ST segment]] elevation, while [[vagal stimulation]] worsens it. During sleep, there is [[heightened vagal tone]], and the pattern may be exacerbated at that time (as is the risk of [[sudden cardiac death]] at that time). The administration of class Ia, Ic and III drugs increases the [[ST segment]] elevation, as does [[fever]]. The impact of exercise depends upon when the EKG is obtained: during exercise the [[ST segment]] elevation may decrease but may increase later after exercise when the body temperature has risen. Similar to [[early repolarization variant]], when the heart rate decreases, the [[ST segment]] elevation increases and when the heart rate increases the [[ST segment]] elevation decreases. While Brugada syndrome is often associated with polymorphic VT which may be self terminating, in the presence of autonomic imbalance, hypokalemia, fever or exacerbating drugs sustained ventricular fibrillation and sudden cardiac death may result.<ref name="pmid15898165">{{cite journal |author=Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A |title=Brugada syndrome: report of the second consensus conference |journal=[[Heart Rhythm : the Official Journal of the Heart Rhythm Society]] |volume=2 |issue=4 |pages=429–40 |year=2005 |month=April |pmid=15898165 |doi= |url= |issn= |accessdate=2012-10-14}}</ref> | ||
The electrocardiographic findings of Brugada syndrome are often concealed, but can be unmasked or modulated by a number of drugs and pathophysiological states including (in alphabetical order)<ref name="pmid15898165">{{cite journal |author=Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A |title=Brugada syndrome: report of the second consensus conference |journal=[[Heart Rhythm : the Official Journal of the Heart Rhythm Society]] |volume=2 |issue=4 |pages=429–40 |year=2005 |month=April |pmid=15898165 |doi= |url= |issn= |accessdate=2012-10-13}}</ref>: | The electrocardiographic findings of Brugada syndrome are often concealed, but can be unmasked or modulated by a number of drugs and pathophysiological states including (in alphabetical order)<ref name="pmid15898165">{{cite journal |author=Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A |title=Brugada syndrome: report of the second consensus conference |journal=[[Heart Rhythm : the Official Journal of the Heart Rhythm Society]] |volume=2 |issue=4 |pages=429–40 |year=2005 |month=April |pmid=15898165 |doi= |url= |issn= |accessdate=2012-10-13}}</ref>: | ||
*A combination of [[glucose]] and [[insulin]]<ref name="pmid12687840">{{cite journal| author=Nogami A, Nakao M, Kubota S, Sugiyasu A, Doi H, Yokoyama K et al.| title=Enhancement of J-ST-segment elevation by the glucose and insulin test in Brugada syndrome. | journal=Pacing Clin Electrophysiol | year= 2003 | volume= 26 | issue= 1 Pt 2 | pages= 332-7 | pmid=12687840 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12687840 }} </ref>. In Thailand large meals of glutinous sticky carbohydrate rich rice have been associated with sudden cardiac death.<ref name="pmid1681278">{{cite journal |author=Nimmannit S, Malasit P, Chaovakul V, Susaengrat W, Vasuvattakul S, Nilwarangkur S |title=Pathogenesis of sudden unexplained nocturnal death (lai tai) and endemic distal renal tubular acidosis |journal=[[Lancet]] |volume=338 |issue=8772 |pages=930–2 |year=1991 |month=October |pmid=1681278 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/0140-6736(91)91786-T |issn= |accessdate=2012-10-14}}</ref> | *A combination of [[glucose]] and [[insulin]]<ref name="pmid12687840">{{cite journal| author=Nogami A, Nakao M, Kubota S, Sugiyasu A, Doi H, Yokoyama K et al.| title=Enhancement of J-ST-segment elevation by the glucose and insulin test in Brugada syndrome. | journal=Pacing Clin Electrophysiol | year= 2003 | volume= 26 | issue= 1 Pt 2 | pages= 332-7 | pmid=12687840 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12687840 }} </ref>. In Thailand large meals of glutinous sticky carbohydrate rich rice have been associated with sudden cardiac death.<ref name="pmid1681278">{{cite journal |author=Nimmannit S, Malasit P, Chaovakul V, Susaengrat W, Vasuvattakul S, Nilwarangkur S |title=Pathogenesis of sudden unexplained nocturnal death (lai tai) and endemic distal renal tubular acidosis |journal=[[Lancet]] |volume=338 |issue=8772 |pages=930–2 |year=1991 |month=October |pmid=1681278 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/0140-6736(91)91786-T |issn= |accessdate=2012-10-14}}</ref> | ||
Revision as of 23:41, 14 October 2012
|
Brugada syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Brugada syndrome overview On the Web |
|
American Roentgen Ray Society Images of Brugada syndrome overview |
|
Risk calculators and risk factors for Brugada syndrome overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The Brugada syndrome is a genetic disease that is characterized by abnormal electrocardiogram (ECG) findings and an increased risk of sudden cardiac death in young adults, and occasionally in children and infants.
Historical Perspective
The Brugada brothers were the first to describe the characteristic ECG findings and link them to sudden death.
Before that the characteristic ECG findings were often mistaken for a right ventricular myocardial infarction. In 1953 a publication by Oscher mentioned that despite being mistaken for right ventricular myocardial infarction, the ECG findings were not associated with myocardial ischemia.[1]
Although the ECG findings of Brugada syndrome were first reported[2] among survivors of cardiac arrest in 1989, it was only in 1992 that the Brugada brothers[3] recognized it as a distinct clinical entity, causing sudden death by causing ventricular fibrillation.
Pathophysiology
Approximately 20% of the cases of Brugada syndrome have been shown to be associated with mutation(s) in the gene that encodes for the sodium ion channel in the cell membranes of the muscle cells of the heart (the myocytes). The gene, named SCN5A, is located on the short arm of the third chromosome (3p21). Loss-of-function mutations in this gene lead to a loss of the action potential dome of some epicardial areas of the right ventricle. This results in transmural and epicardial dispersion of repolarization. Over 160 mutations in the SCN5A gene have been discovered to date, each having varying mechanisms and effects on function, thereby explaining the varying degrees of penetration and expression of this disorder. [4]
Differentiating Brugada Syndrome from other Diseases
Abnormalities that can lead to ST-segment elevation in the right precordial leads include the following:[5]
- Acute myocardial ischemia or infarction
- Acute myocarditis
- Acute pericarditis
- Acute pulmonary thromboemboli
- Arrhythmogenic right ventricular dysplasia / cardiomyopathy (ARVD/C)[6][7]
- Cardioversion. Brugada-like ECG changes can be observed briefly after direct-current cardioversion. It is currently unclear if this is a sign that the patient is a gene carrier for Brugada syndrome.[8][9][10]
- Cocaine intoxication
- Coronary spasm
- Dissecting aortic aneurysm[11]
- Duchenne muscular dystrophy[12]
- Early repolarization
- Friedreich ataxia
- Heterocyclic antidepressant overdose
- Hypercalcemia[13][14]
- Hyperkalemia[15][16][17]
- Hypothermia, can cause an Osborn wave on the ECG which can sometimes resemble Brugada syndrome[18][19]
- Left ventricular hypertrophy
- Pectus excavatum[20]
- Prinzmetal's angina[21]
- Mediastinal tumor compressing the right ventricular outflow tract (RVOT)
- Right or left bundle-branch block (atypical)
- Right ventricular infarction
- Right ventricular ischemia
- Right ventricular outflow tract compression due to a mediastinal tumor[22]or hemopericardium[23]
- Thiamine deficiency[24]
- Various central and autonomic nervous system abnormalities
- Other conditions that can lead to ST-segment elevation in the right precordial leads
- Early repolarization syndrome
- Other normal variants (particularly in males)
Differentiating Brugada Syndrome from Arrhythmogenic Right Ventricular Dysplasia
Although both Brugada syndrome and Arrhythmogenic Right Ventricular Dysplasia are associated with sudden cardiac death in young patients, the two syndromes are fairly easy to distinguish electrocardiographically and clinically.
Genetics
There is only one gene associated with Brugada syndrome, namely the SCN5A gene, and there is no overlap of the genetic abnormalities associated with Arrhythmogenic Right Ventricular Dysplasia.
Structural Abnormalities of the right Ventricle
While Brugada syndrome is not associated with structural abnormalities in the right ventricle, arrhythmogenic right ventricular dysplasia is associated with fibrofatty infiltration.
Precipitant of Ventricular Arrhythmias
Arrhythmogenic right ventricular dysplasia is associated with monomorphic ventricular tachycardia with a left bundle branch morphology and is precipitated by catecholamines or exercise. In contrast, Brugada syndrome is associated with polymorphic ventricular tachycardia and occurs predominantly during sleep or rest.
Response to Pharmacologic Agents
The EKG abnormalities of Brugada syndrome are enhanced by vagotonic agents, beta-adrenergic blockers, and sodium channel blockers whereas the EKG changes of arrhythmogenic right ventricular dysplasia are constant and do not very with vagotonic agents, beta-adrenergic blockers, or sodium channel blockers.
Epidemiology and Demographics
Insofar as Brugada syndrome is a relatively newly recognized syndrome, its incidence and prevalence continues to increase. Brugada syndrome is quite common in Southeast Asia where it is endemic, and affects 50 out of every 10,000 individuals. It is the second leading cause of death after car accidents among young people in these countries. It has been estimated that Brugada syndrome accounts for 4% of all sudden cardiac deaths and 20% of sudden cardiac deaths among patients with structurally normal hearts. It is 8-10 times more common in men.
Prevalence
The prevalence of the Brugada syndrome is estimated at 5-50:10,000, largely depending on geographic location.
Age
The average age at the time of initial diagnosis or sudden death is 40 ± 22 years, with the youngest patient diagnosed at 2 days of age and the oldest at 84 years. Brugada syndrome usually becomes apparent in adulthood, although signs and symptoms, including sudden death, can occur any time from early infancy to old age. The mean age of sudden death is approximately 40 years. This condition may explain some cases of sudden infant death syndrome (SIDS), which is a major cause of death in babies younger than one year. It is characterized by sudden and unexplained death, usually during sleep. Sudden unexplained nocturnal death syndrome (SUNDS) is a condition characterized by unexpected cardiac arrest in young adults, usually at night during sleep. This condition was originally described in Southeast Asian populations, where it is a major cause of death. Researchers have determined that SUNDS and Brugada syndrome are the same disorder.
Race
This condition occurs much more frequently in people of Asian ancestry, particularly in Japanese and Southeast Asian populations. It is the most common cause of sudden death in young men without known underlying cardiac disease in Thailand and Laos[25]. In some southeast Asian countries the disease is considered endemic and believed to be the second cause of death among young men (after car accidents). In these countries Brugada syndrome is believed to underly (in part) the 'Sudden Unexpected Death Syndrome' (SUDS). This relation has, however, not been thoroughly investigated and there are almost no epidemiological studies into Brugada syndrome ECGs (apart from Japan). In different Asian countries, different names have been given to SUDS: in the Phillipines it is called bangungut (to rise and moan in sleep) and in Thailand lai tai (death during sleep).
Gender
Although Brugada syndrome affects both men and women, the condition appears to be 8 to 10 times more common in men. Researchers suspect that testosterone, a sex hormone present at much higher levels in men, may be responsible for this difference.
Risk Factors: Agents and Scenarios that Provoke the Brugada Syndrome Pattern
The EKG changes of Brugada syndrome can vary over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the ST segment elevation, while vagal stimulation worsens it. During sleep, there is heightened vagal tone, and the pattern may be exacerbated at that time (as is the risk of sudden cardiac death at that time). The administration of class Ia, Ic and III drugs increases the ST segment elevation, as does fever. The impact of exercise depends upon when the EKG is obtained: during exercise the ST segment elevation may decrease but may increase later after exercise when the body temperature has risen. Similar to early repolarization variant, when the heart rate decreases, the ST segment elevation increases and when the heart rate increases the ST segment elevation decreases. While Brugada syndrome is often associated with polymorphic VT which may be self terminating, in the presence of autonomic imbalance, hypokalemia, fever or exacerbating drugs sustained ventricular fibrillation and sudden cardiac death may result.[26]
The electrocardiographic findings of Brugada syndrome are often concealed, but can be unmasked or modulated by a number of drugs and pathophysiological states including (in alphabetical order)[26]:
- A combination of glucose and insulin[27]. In Thailand large meals of glutinous sticky carbohydrate rich rice have been associated with sudden cardiac death.[28]
- Ajmaline[29] (a diagnostic test agent)
- α-adrenergic agonists[30]
- β-adrenergic blockers[31][30] such as propranolol.
- Calcium channel blockers
- Carotid sinus massage
- Cocaine[32][33][34]
- Dimenhydrinate
- Family History: In large studies, a family history of sudden cardiac death among patients with Brugada syndrome does not appear to be a risk factor for sudden cardiac death in siblings.
- Fever[35].[36][37][38][39] Hot baths and warm climates (such as that in Northeastern Thailand) may be precipitating factors for sudden cardiac death. It is for this reason that antipyretic agents are recommended to aggressively treat a fever in the patient with Brugada syndrome.
- Flecainide[31][40][41][42] (a diagnostic test agent)
- Hypercalcemia[13][14]
- Hyperkalemia[43][44][17]
- Hypokalemia.[45] Hypokalemia in a patient with Brugada syndrome may trigger sustained ventricular fibrillation and sudden cardiac death. In northeastern Thailand where potassium deficiency is widespread, there is a higher incidence of sudden cardiac death than is observed in Bangkok where potassium levels in food are much higher.[28]
- Lithium. Administration of Lithium can result in EKG manifestations of the Brugada syndrome. [46][47]. Syncope and sudden cardiac death have been observed in these patients.[48] The putative role of lithium has been suggested in so far as withdrawal of lithium results in either 1) normalization of the ECG or 2) conversion of the Brugada pattern to type 2 or 3. The appearance of Brugada type EKG patterns does not require toxic lithium levels.
- Phenothiazines
- Potassium channel openers such as nicorandil.
- Procainamide[31] [30](a diagnostic test agent)
- Propranolol intoxication[49]
- Selective serotonin reuptake inhibitors
- Shaving due to vagal stimulation[50][51][52]
- Sleep may exacerbate the electrocardiographic and clinical findings of brugada syndrome due to variations in the balance of sympathetic versus vagal tone, hormonal changes and other metabolic factors.[26][53][54][51]
- Sodium channel blockers[55][31][56][41] (a diagnostic test agent)
- Tetracyclic antidepressants[57]
Risk Stratification
In a study of 547 individuals who had confirmed Brugada syndrome who had no prior history of cardiac arrest, Brugada and associates identified the following correlates of future events:[61]
Inducibility on Electrophysiologic Testing
Patients who are inducible at the time electrophysiologic study have an eightfold increased risk of aborted sudden cardiac death compared with those patients who are not inducible.[62] Some groups have advocated that programmed electrical stimulation (PES) be performed to induce ventricular fibrillation for risk assessment in Brugada patients [63][64] Other groups have not reproduced the predictive value of these tests,[65][66] so the value of programmed electrical stimulation (PES) and inducibility remains controversial.
Spontaneous Type I Brugada Pattern
The presence of a spontaneous abnormal Type I pattern of ST segment elevation is associated with a 7.7 fold increased risk of in arrhythmic event during a patient's lifetime compared with those patients who only develop a Type I pattern following sodium blocker infusion.[67]
Male Gender
Male gender is associate with the 5.5 fold increased risk of sudden cardiac death.[68]
Family History
A family history of the disease is not associated with a higher risk of sudden death compared with sporadic occurrence of the disease.[69]
Symptoms
In another study, Brugada has reported that the symptoms of the patient may aid in risk stratification:[70]
- Brugada syndrome patients who present with aborted sudden cardiac death are at particularly high risk of recurrence with an incidence of 69% at 54 months of follow-up in the Brugada series.
- Brugada syndrome patients with syncope and Type 1 ST elevation pattern have a 19% risk of recurrence at 26 months.
- Brugada syndrome patients who are asymptomatic have an 8% risk of cardiac events over the same time period.
Genetic Testing
Genetic testing does not identify patients at high risk of sudden cardiac death and does not aid in risk stratification.[26]
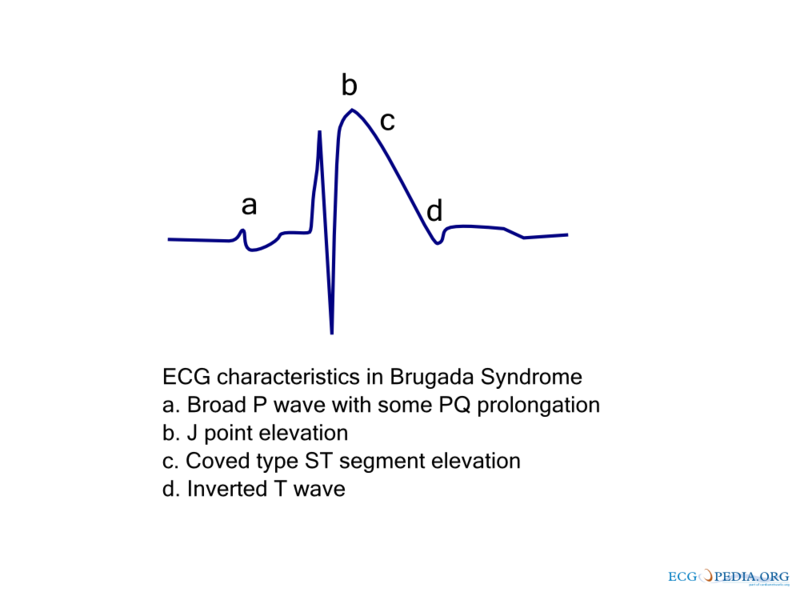
EKG Characteristics
As shown by the racing below, The EKG characteristics of Bugada syndrome include:
- a) A broad P-wave with some PQ prolongation
- b) J point elevation in the right precordial leads (V1-V3)
- c) Coved ST segment elevation
- d) An inverted T wave
References
- ↑ OSHER HL, WOLFF L (1953). "Electrocardiographic pattern simulating acute myocardial injury". The American Journal of the Medical Sciences. 226 (5): 541–5. PMID 13104407. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Martini B, Nava A, Thiene G, Buja GF, Canciani B, Scognamiglio R, Daliento L, Dalla Volta S. Ventricular fibrillation without apparent heart disease: description of six cases. Am Heart J 1989 Dec;118(6):1203-9 PMID 2589161
- ↑ Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992 Nov 15;20(6):1391-6. PMID 1309182
- ↑ Napolitano C, Priori SG (2006). "Brugada syndrome". Orphanet journal of rare diseases. 1: 35. doi:10.1186/1750-1172-1-35. PMID 16972995.
- ↑ Takehara N, Makita N, Kawabe J, Sato N, Kawamura Y, Kitabatake A, Kikuchi K (2004). "A cardiac sodium channel mutation identified in Brugada syndrome associated with atrial standstill". Journal of Internal Medicine. 255 (1): 137–42. PMID 14687250. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help) - ↑ Corrado D, Nava A, Buja G, Martini B, Fasoli G, Oselladore L, Turrini P, Thiene G. Familial cardiomyopathy underlies syndrome of right bundle branch block, ST segment elevation and sudden death. J Am Coll Cardiol. 1996; 27: 443–448.
- ↑ Corrado D, Basso C, Buja G, Nava A, Rossi L, Thiene G. Right bundle branch block, right precordial ST-segment elevation, and sudden death in young people. Circulation. 2001; 103: 710–717.
- ↑ Kok LC, Mitchell MA, Haines DE, Mounsey JP, DiMarco JP (2000). "Transient ST elevation after transthoracic cardioversion in patients with hemodynamically unstable ventricular tachyarrhythmia". The American Journal of Cardiology. 85 (7): 878–81, A9. PMID 10758932. Retrieved 2012-10-14. Unknown parameter
|month=ignored (help) - ↑ Gurevitz O, Glikson M (2003). "Cardiac resynchronization therapy: a new frontier in the management of heart failure". The Israel Medical Association Journal : IMAJ. 5 (8): 571–5. PMID 12929296. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Gurevitz O, Lipchenca I, Yaacoby E, Segal E, Perel A, Eldar M, Glikson M (2002). "ST-segment deviation following implantable cardioverter defibrillator shocks: incidence, timing, and clinical significance". Pacing and Clinical Electrophysiology : PACE. 25 (10): 1429–32. PMID 12418739. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Myers GB. Other QRS-T patterns that may be mistaken for myocardial infarction; IV. Alterations in blood potassium; myocardial ischemia; subepicardial myocarditis; distortion associated with arrhythmias. Circulation. 1950; 2: 75–93.
- ↑ Perloff JK, Henze E, Schelbert HR. Alterations in regional myocardial metabolism, perfusion, and wall motion in Duchenne muscular dystrophy studied by radionuclide imaging. Circulation. 1984; 69: 33–42.
- ↑ 13.0 13.1 Douglas PS, Carmichael KA, Palevsky PM (1984). "Extreme hypercalcemia and electrocardiographic changes". The American Journal of Cardiology. 54 (6): 674–5. PMID 6475795. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ 14.0 14.1 Sridharan MR, Horan LG (1984). "Electrocardiographic J wave of hypercalcemia". The American Journal of Cardiology. 54 (6): 672–3. PMID 6475794. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Myers GB. Other QRS-T patterns that may be mistaken for myocardial infarction; IV. Alterations in blood potassium; myocardial ischemia; subepicardial myocarditis; distortion associated with arrhythmias. Circulation. 1950; 2: 75–93.
- ↑ Merrill JP, Levine HD, Somerville W, Smith S. Clinical recognition and treatment of acute potassium intoxication. Ann Intern Med. 1950; 33: 797–830.
- ↑ 17.0 17.1 Ortega-Carnicer J, Benezet J, Ruiz-Lorenzo F, Alcázar R (2002). "Transient Brugada-type electrocardiographic abnormalities in renal failure reversed by dialysis". Resuscitation. 55 (2): 215–9. PMID 12413761. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help) - ↑ Osborn JJ. Experimental hypothermia; respiratory and blood pH changes in relation to cardiac function. Am J Physiol. 1953; 175: 389–398.
- ↑ Noda T, Shimizu W, Tanaka K, Chayama K (2003). "Prominent J wave and ST segment elevation: serial electrocardiographic changes in accidental hypothermia". Journal of Cardiovascular Electrophysiology. 14 (2): 223. PMID 12693512. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help) - ↑ Kataoka H. Electrocardiographic patterns of the Brugada syndrome in right ventricular infarction/ischemia. Am J Cardiol. 2000; 86: 1056.
- ↑ Wang K, Asinger RW, Marriott HJ (2003). "ST-segment elevation in conditions other than acute myocardial infarction". The New England Journal of Medicine. 349 (22): 2128–35. doi:10.1056/NEJMra022580. PMID 14645641. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help) - ↑ Tarín N, Farré J, Rubio JM, Tuñón J, Castro-Dorticós J (1999). "Brugada-like electrocardiographic pattern in a patient with a mediastinal tumor". Pacing and Clinical Electrophysiology : PACE. 22 (8): 1264–6. PMID 10461308. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Tomcsanyi J, Simor T, Papp L. Images in cardiology. Haemopericardium and Brugada-like ECG pattern in rheumatoid arthritis. Heart. 2002; 87: 234.
- ↑ Read DH, Harrington DD (1981). "Experimentally induced thiamine deficiency in beagle dogs: clinical observations". American Journal of Veterinary Research. 42 (6): 984–91. PMID 7197132. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Brugada J, Brugada P, Brugada R. The syndrome of right bundle branch block ST segment elevation in V1 to V3 and sudden death--the Brugada syndrome. Europace. 1999 Jul;1(3):156-66. PMID 11225790
- ↑ 26.0 26.1 26.2 26.3 Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A (2005). "Brugada syndrome: report of the second consensus conference". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 2 (4): 429–40. PMID 15898165. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Nogami A, Nakao M, Kubota S, Sugiyasu A, Doi H, Yokoyama K; et al. (2003). "Enhancement of J-ST-segment elevation by the glucose and insulin test in Brugada syndrome". Pacing Clin Electrophysiol. 26 (1 Pt 2): 332–7. PMID 12687840.
- ↑ 28.0 28.1 Nimmannit S, Malasit P, Chaovakul V, Susaengrat W, Vasuvattakul S, Nilwarangkur S (1991). "Pathogenesis of sudden unexplained nocturnal death (lai tai) and endemic distal renal tubular acidosis". Lancet. 338 (8772): 930–2. PMID 1681278. Retrieved 2012-10-14. Unknown parameter
|month=ignored (help) - ↑ Rolf S, Bruns HJ, Wichter T, Kirchhof P, Ribbing M, Wasmer K; et al. (2003). "The ajmaline challenge in Brugada syndrome: diagnostic impact, safety, and recommended protocol". Eur Heart J. 24 (12): 1104–12. PMID 12804924.
- ↑ 30.0 30.1 30.2 Miyazaki T, Mitamura H, Miyoshi S, Soejima K, Aizawa Y, Ogawa S (1996). "Autonomic and antiarrhythmic drug modulation of ST segment elevation in patients with Brugada syndrome". J Am Coll Cardiol. 27 (5): 1061–70. doi:10.1016/0735-1097(95)00613-3. PMID 8609322.
- ↑ 31.0 31.1 31.2 31.3 Brugada P, Brugada J, Brugada R (2000). "Arrhythmia induction by antiarrhythmic drugs". Pacing Clin Electrophysiol. 23 (3): 291–2. PMID 10750126.
- ↑ Ortega-Carnicer J, Bertos-Polo J, Gutiérrez-Tirado C (2001). "Aborted sudden death, transient Brugada pattern, and wide QRS dysrrhythmias after massive cocaine ingestion". J Electrocardiol. 34 (4): 345–9. PMID 11590577.
- ↑ 33.0 33.1 Rouleau F, Asfar P, Boulet S, Dube L, Dupuis JM, Alquier P; et al. (2001). "Transient ST segment elevation in right precordial leads induced by psychotropic drugs: relationship to the Brugada syndrome". J Cardiovasc Electrophysiol. 12 (1): 61–5. PMID 11204086.
- ↑ Littmann L, Monroe MH, Svenson RH (2000). "Brugada-type electrocardiographic pattern induced by cocaine". Mayo Clin Proc. 75 (8): 845–9. doi:10.4065/75.8.845. PMID 10943241.
- ↑ Antzelevitch C, Brugada R (2002). "Fever and Brugada syndrome". Pacing Clin Electrophysiol. 25 (11): 1537–9. PMID 12494608.
- ↑ González Rebollo JM, Hernández Madrid A, García A, García de Castro A, Mejías A, Moro C (2000). "[Recurrent ventricular fibrillation during a febrile illness in a patient with the Brugada syndrome]". Rev Esp Cardiol. 53 (5): 755–7. PMID 10816181.
- ↑ Saura D, García-Alberola A, Carrillo P, Pascual D, Martínez-Sánchez J, Valdés M (2002). "Brugada-like electrocardiographic pattern induced by fever". Pacing Clin Electrophysiol. 25 (5): 856–9. PMID 12049381.
- ↑ Porres JM, Brugada J, Urbistondo V, García F, Reviejo K, Marco P (2002). "Fever unmasking the Brugada syndrome". Pacing Clin Electrophysiol. 25 (11): 1646–8. PMID 12494626.
- ↑ Kum LC, Fung JW, Sanderson JE (2002). "Brugada syndrome unmasked by febrile illness". Pacing Clin Electrophysiol. 25 (11): 1660–1. PMID 12494630.
- ↑ Fujiki A, Usui M, Nagasawa H, Mizumaki K, Hayashi H, Inoue H (1999). "ST segment elevation in the right precordial leads induced with class IC antiarrhythmic drugs: insight into the mechanism of Brugada syndrome". J Cardiovasc Electrophysiol. 10 (2): 214–8. PMID 10090224.
- ↑ 41.0 41.1 Krishnan SC, Josephson ME (1998). "ST segment elevation induced by class IC antiarrhythmic agents: underlying electrophysiologic mechanisms and insights into drug-induced proarrhythmia". J Cardiovasc Electrophysiol. 9 (11): 1167–72. PMID 9835260.
- ↑ Gasparini M, Priori SG, Mantica M, Napolitano C, Galimberti P, Ceriotti C; et al. (2003). "Flecainide test in Brugada syndrome: a reproducible but risky tool". Pacing Clin Electrophysiol. 26 (1 Pt 2): 338–41. PMID 12687841.
- ↑ MYERS GB (1950). "Other QRS-T patterns that may be mistaken for myocardial infarction; IV. alterations in blood potassium; myocardial ischemia; subepicardial myocarditis; distortion associated with arrhythmias". Circulation. 2 (1): 75–93. PMID 15427197.
- ↑ MERRILL JP, LEVINE HD, SOMERVILLE W, SMITH S (1950). "Clinical recognition and treatment of acute potassium intoxication". Ann Intern Med. 33 (4): 797–830. PMID 14771753.
- ↑ Araki T, Konno T, Itoh H, Ino H, Shimizu M (2003). "Brugada syndrome with ventricular tachycardia and fibrillation related to hypokalemia". Circ J. 67 (1): 93–5. PMID 12520160.
- ↑ Pirotte MJ, Mueller JG, Poprawski T. A case report of Brugada-type electrocardiographic changes in a patient taking lithium. Am J Emerg Med. 2008; 26: 113.
- ↑ Wright D, Salehian O. Brugada-Type Electrocardiographic Changes Induced by Long-Term Lithium Use. Circulation, FRCPC2010;122:e418-e419
- ↑ Laske C, Soekadar SR, Laszlo R, Plewnia C. Brugada syndrome in a patient treated with lithium. Am J Psychiatry. 2007; 164: 1440–1441.
- ↑ Aouate P, Clerc J, Viard P, Seoud J (2005). "Propranolol intoxication revealing a Brugada syndrome". J Cardiovasc Electrophysiol. 16 (3): 348–51. doi:10.1046/j.1540-8167.2005.40564.x. PMID 15817098.
- ↑ 50.0 50.1 Kasanuki H, Ohnishi S, Ohtuka M, Matsuda N, Nirei T, Isogai R; et al. (1997). "Idiopathic ventricular fibrillation induced with vagal activity in patients without obvious heart disease". Circulation. 95 (9): 2277–85. PMID 9142005.
- ↑ 51.0 51.1 51.2 Mizumaki K, Fujiki A, Tsuneda T, Sakabe M, Nishida K, Sugao M; et al. (2004). "Vagal activity modulates spontaneous augmentation of ST elevation in the daily life of patients with Brugada syndrome". J Cardiovasc Electrophysiol. 15 (6): 667–73. doi:10.1046/j.1540-8167.2004.03601.x. PMID 15175062.
- ↑ 52.0 52.1 Litovsky SH, Antzelevitch C (1990). "Differences in the electrophysiological response of canine ventricular subendocardium and subepicardium to acetylcholine and isoproterenol. A direct effect of acetylcholine in ventricular myocardium". Circ Res. 67 (3): 615–27. PMID 2397572.
- ↑ Kasanuki H, Ohnishi S, Ohtuka M, Matsuda N, Nirei T, Isogai R, Shoda M, Toyoshima Y, Hosoda S. Idiopathic ventricular fibrillation induced with vagal activity in patients without obvious heart disease. Circulation. 1997; 95: 2277–2285.
- ↑ Proclemer A, Facchin D, Feruglio GA, Nucifora R (1993). "[Recurrent ventricular fibrillation, right bundle-branch block and persistent ST segment elevation in V1-V3: a new arrhythmia syndrome? A clinical case report]". Giornale Italiano Di Cardiologia (in Italian). 23 (12): 1211–8. PMID 8174872. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Brugada R, Brugada J, Antzelevitch C, Kirsch GE, Potenza D, Towbin JA; et al. (2000). "Sodium channel blockers identify risk for sudden death in patients with ST-segment elevation and right bundle branch block but structurally normal hearts". Circulation. 101 (5): 510–5. PMID 10662748.
- ↑ Shimizu W, Antzelevitch C, Suyama K, Kurita T, Taguchi A, Aihara N; et al. (2000). "Effect of sodium channel blockers on ST segment, QRS duration, and corrected QT interval in patients with Brugada syndrome". J Cardiovasc Electrophysiol. 11 (12): 1320–9. PMID 11196553.
- ↑ 57.0 57.1 Bolognesi R, Tsialtas D, Vasini P, Conti M, Manca C (1997). "Abnormal ventricular repolarization mimicking myocardial infarction after heterocyclic antidepressant overdose". Am J Cardiol. 79 (2): 242–5. PMID 9193039.
- ↑ Goldgran-Toledano D, Sideris G, Kevorkian JP (2002). "Overdose of cyclic antidepressants and the Brugada syndrome". N Engl J Med. 346 (20): 1591–2. doi:10.1056/NEJM200205163462020. PMID 12015405.
- ↑ Tada H, Sticherling C, Oral H, Morady F (2001). "Brugada syndrome mimicked by tricyclic antidepressant overdose". J Cardiovasc Electrophysiol. 12 (2): 275. PMID 11232630.
- ↑ Babaliaros VC, Hurst JW (2002). "Tricyclic antidepressants and the Brugada syndrome: an example of Brugada waves appearing after the administration of desipramine". Clin Cardiol. 25 (8): 395–8. PMID 12173907.
- ↑ Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003; 108: 3092–3096.
- ↑ Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003; 108: 3092–3096.
- ↑ Brugada J, Brugada R, Antzelevitch C, Towbin J, Nademanee K, Brugada P (2002). "Long-term follow-up of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3". Circulation. 105 (1): 73–8. PMID 11772879. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help) - ↑ Brugada P, Brugada R, Mont L, Rivero M, Geelen P, Brugada J (2003). "Natural history of Brugada syndrome: the prognostic value of programmed electrical stimulation of the heart". Journal of Cardiovascular Electrophysiology. 14 (5): 455–7. PMID 12776858. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help) - ↑ Priori SG, Napolitano C, Gasparini M, Pappone C, Della Bella P, Giordano U, Bloise R, Giustetto C, De Nardis R, Grillo M, Ronchetti E, Faggiano G, Nastoli J (2002). "Natural history of Brugada syndrome: insights for risk stratification and management". Circulation. 105 (11): 1342–7. PMID 11901046. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help) - ↑ Eckardt L, Probst V, Smits JP, Bahr ES, Wolpert C, Schimpf R, Wichter T, Boisseau P, Heinecke A, Breithardt G, Borggrefe M, LeMarec H, Böcker D, Wilde AA (2005). "Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome". Circulation. 111 (3): 257–63. doi:10.1161/01.CIR.0000153267.21278.8D. PMID 15642768. Retrieved 2012-10-13. Unknown parameter
|month=ignored (help) - ↑ Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003; 108: 3092–3096.
- ↑ Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003; 108: 3092–3096.
- ↑ Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003; 108: 3092–3096.
- ↑ Brugada J, Brugada R, Antzelevitch C, Towbin J, Nademanee K, Brugada P. Long-term follow-up of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002; 105: 73–78.