Brugada syndrome electrocardiogram: Difference between revisions
| Line 32: | Line 32: | ||
[[File:Brugada ecg characteristics.png|center|500px]] | [[File:Brugada ecg characteristics.png|center|500px]] | ||
Typically these changes are in the right precordial leads but these EKG changes can occur | Typically these changes are in the right precordial leads but these EKG changes can occur in the inferior <ref name="pmid10695469">{{cite journal |author=Kalla H, Yan GX, Marinchak R |title=Ventricular fibrillation in a patient with prominent J (Osborn) waves and ST segment elevation in the inferior electrocardiographic leads: a Brugada syndrome variant? |journal=[[Journal of Cardiovascular Electrophysiology]] |volume=11 |issue=1 |pages=95–8 |year=2000 |month=January |pmid=10695469 |doi= |url= |issn= |accessdate=2012-10-14}}</ref> or left precordial leads<ref name="pmid14661171">{{cite journal |author=Horigome H, Shigeta O, Kuga K, Isobe T, Sakakibara Y, Yamaguchi I, Matsui A |title=Ventricular fibrillation during anesthesia in association with J waves in the left precordial leads in a child with coarctation of the aorta |journal=[[Journal of Electrocardiology]] |volume=36 |issue=4 |pages=339–43 |year=2003 |month=October |pmid=14661171 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0022073603000797 |issn= |accessdate=2012-10-14}}</ref>. The fact that these cases may represent atypical variants of Brugada syndrome is supported by the observation that these cases were associated with [[SCN5A]] genetic abnormalities. | ||
==Provocation of EKG Changes== | ==Provocation of EKG Changes== | ||
Revision as of 15:17, 14 October 2012
|
Brugada syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Brugada syndrome electrocardiogram On the Web |
|
American Roentgen Ray Society Images of Brugada syndrome electrocardiogram |
|
Risk calculators and risk factors for Brugada syndrome electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
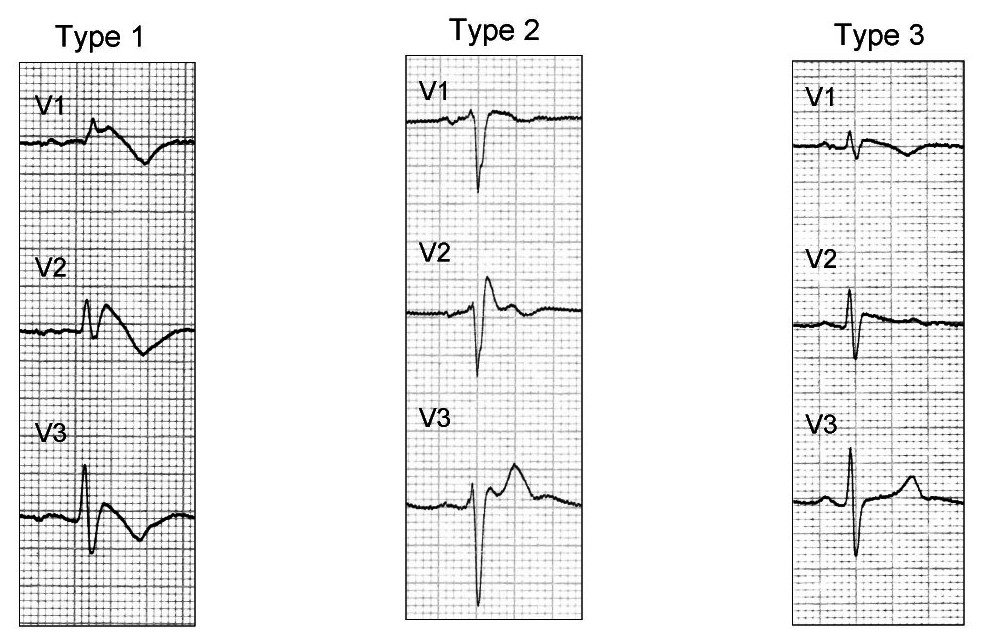
There are three electrocardiographic patterns associated with Brugada syndrome: Type I, Type II and Type III. The diagnosis of Brugada syndrome is based upon the presence of Type I EKG changes. Patients with Type II or Type III Brugada patterns can convert to a Type I Brugada pattern following the administration of sodium channel blockers such as ajmaline and flecainide. Type 1 Brugada syndrome may always be present on the EKG, or it may be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels such as ajmaline, flecainide) or it may be unmasked by various triggers or risk factors.
Type 1 Brugada pattern is characterized by ST elevations in leadsV1-V3 with a right bundle branch block (RBBB). A prolongation of the PR interval is also frequently seen. The EKG changes of Brugada syndrome can vary over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the ST segment elevation, while vagal stimulation worsens it. The administration of class Ia, Ic and III drugs increases the ST segment elevation, as does fever. Exercise decreases ST segment elevation in some patients but increases it in others (after exercise when the body temperature has risen). The changes in heart rate induced by atrial pacing are accompanied by changes in the degree of ST segment elevation. When the heart rate decreases, the ST segment elevation increases and when the heart rate increases the ST segment elevation decreases.
The three patterns of Brugada syndrome (Type I,II,III) are shown below:
Diagnostic Criteria for Brugada Syndrome[1]
1. The presence of Type 1 ST-segment elevation in more than one right precordial lead (V1-V3). Type I ST elevation must be observed either spontaneously or following the administration of a sodium channel blocking agent.
2. One or more of the following criteria must also be met:
- Family history of sudden cardiac death (SCD) (<45 years old)
- Documented ventricular fibrillation (VF)
- Polymorphic ventricular tachycardia
- Coved-type ECG changes in family members
- Inducibility of ventricular tachycardia (VT) with programmed electrical stimulation (PES)
3. The patient is also diagnosed as having Brugada syndrome when a Type 2 (saddleback pattern) or Type 3 ST-segment elevation is observed in more than one right precordial lead under baseline conditions and that can be converted to the diagnostic Type 1 pattern following administration of a sodium channel blocker.
Type 1 Brugada Syndrome
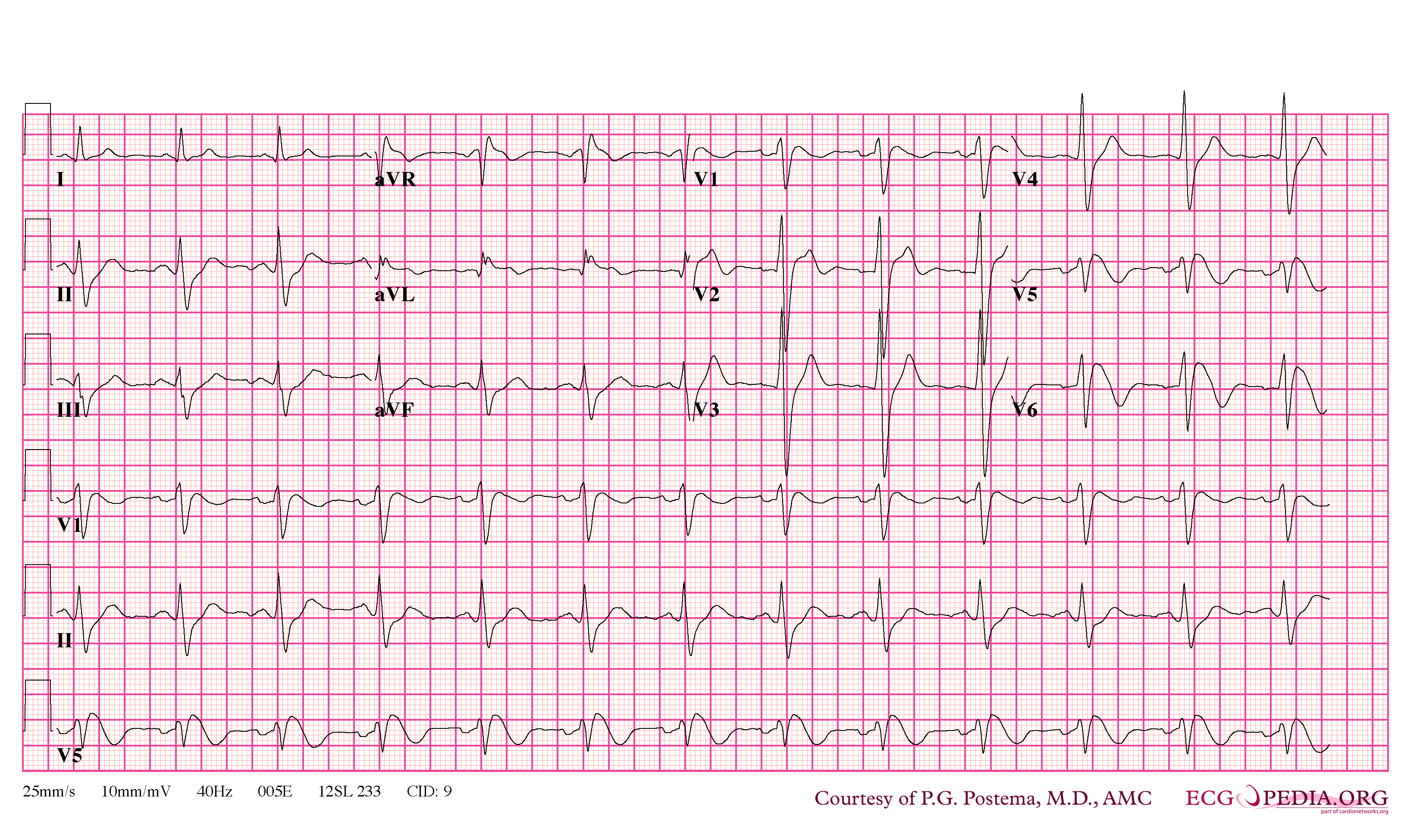
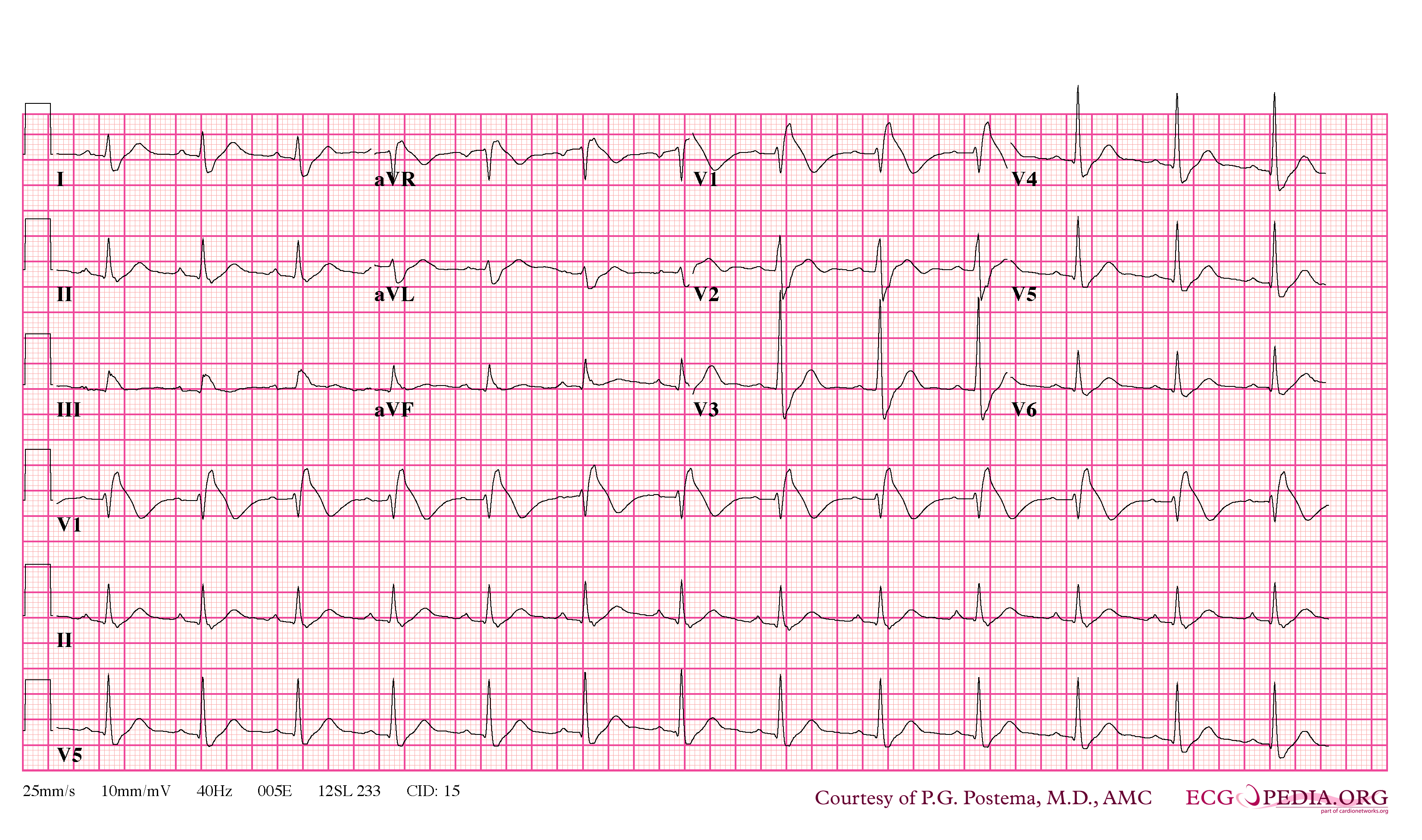
As shown by the tracing below, the EKG characteristics of Type 1 Brugada syndrome include the following EKG findings in the right precordial leads (V1-V3):
- a) A broad P-wave with some PQ prolongation
- b) J point elevation in the right precordial leads (V1-V3)
- c) Coved ST segment elevation
- d) An inverted T wave
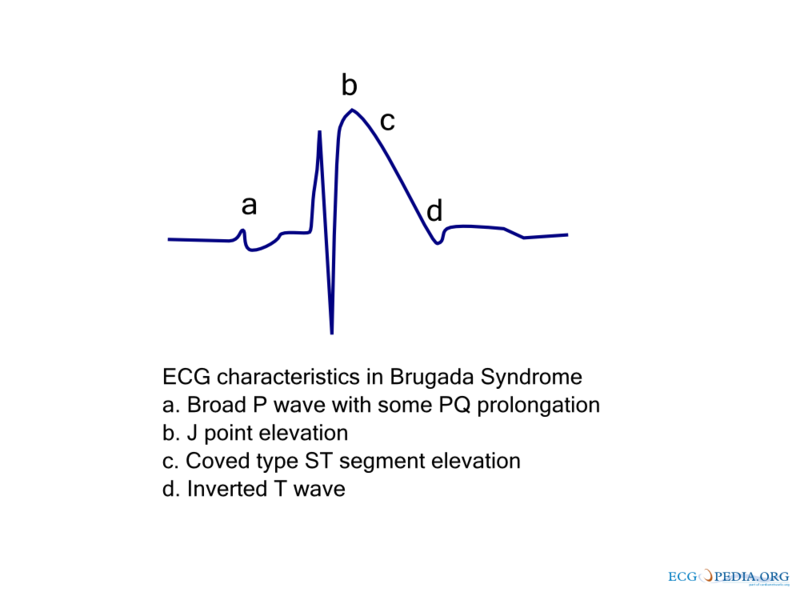
Typically these changes are in the right precordial leads but these EKG changes can occur in the inferior [2] or left precordial leads[3]. The fact that these cases may represent atypical variants of Brugada syndrome is supported by the observation that these cases were associated with SCN5A genetic abnormalities.
Provocation of EKG Changes
The findings of Brugada syndrome are often concealed, but can be unmasked or modulated by a number of drugs and pathophysiological states including sodium channel blockers, a febrile state, vagotonic agents that mimic sleep, tricyclic antidepressants, as well as cocaine and Propranolol intoxication.
EKG Images
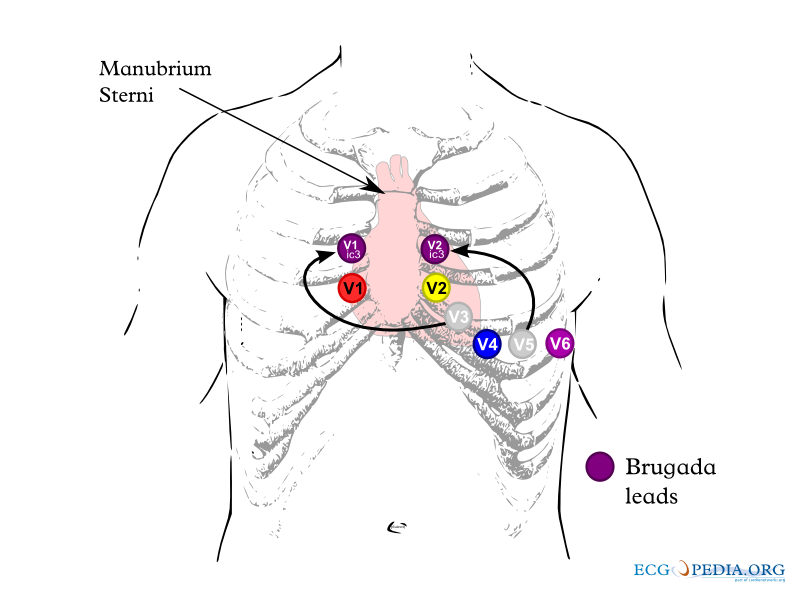
Shown below is an example of lead placements in Brugada syndrome.
Shown below is an example of general EKG characteristics in Brugada syndrome - right bundle branch block in leads V1-2 and ST segment elevation in leads V1-3
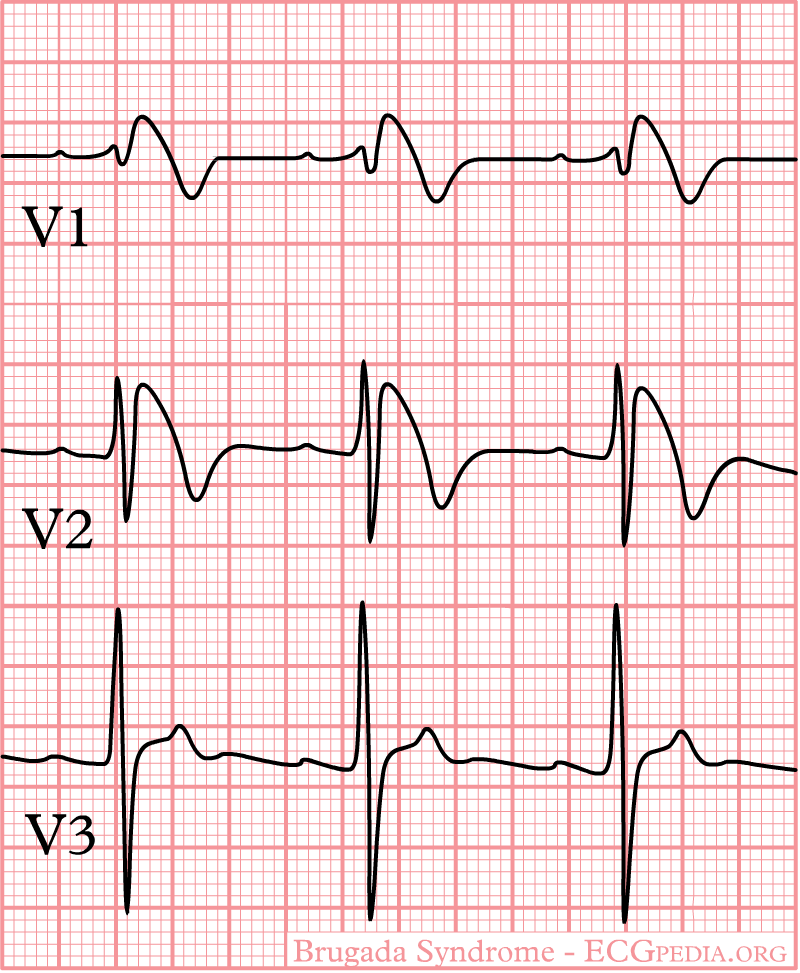
Shown below is an example of Brugada syndrome with ST segment elevation.

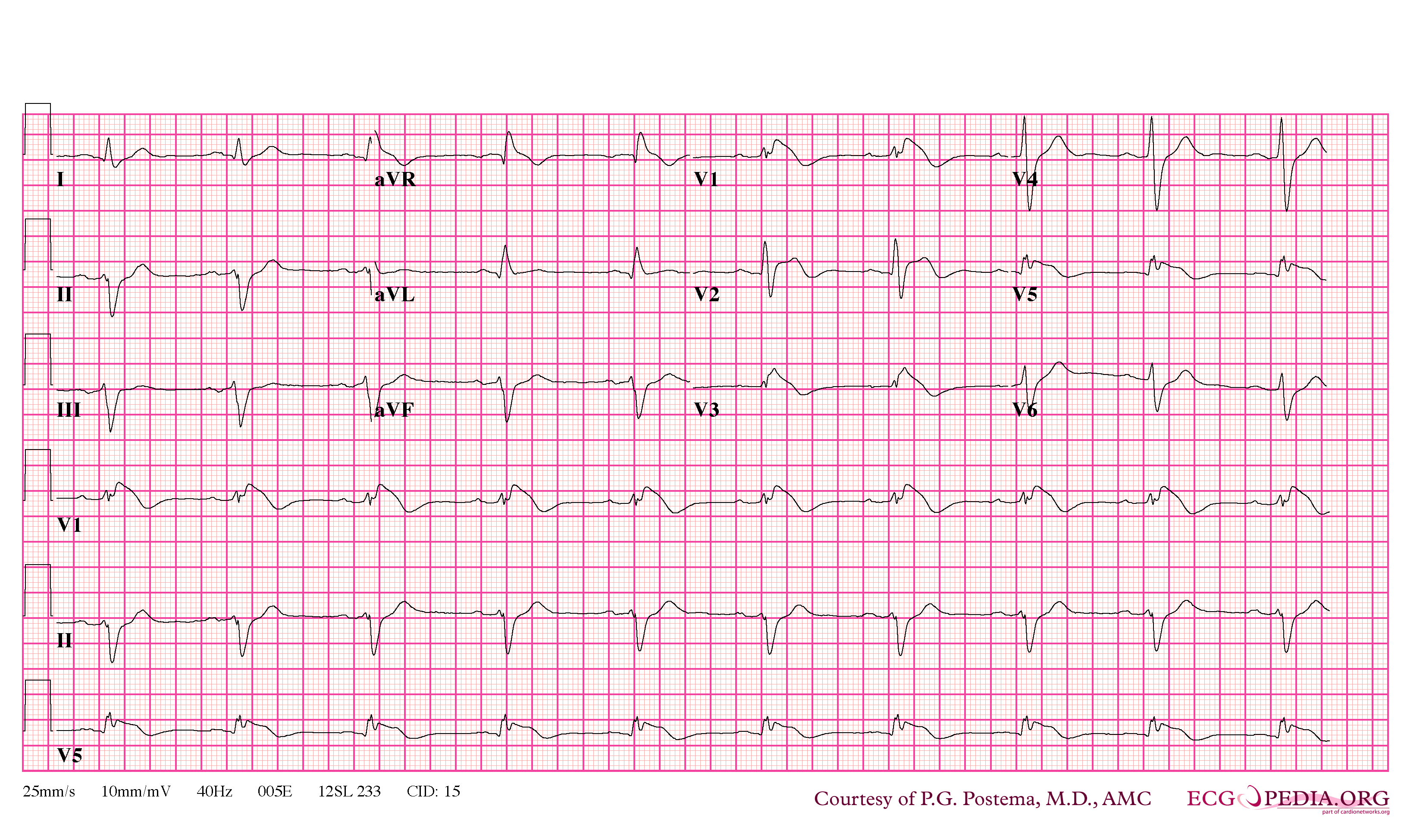
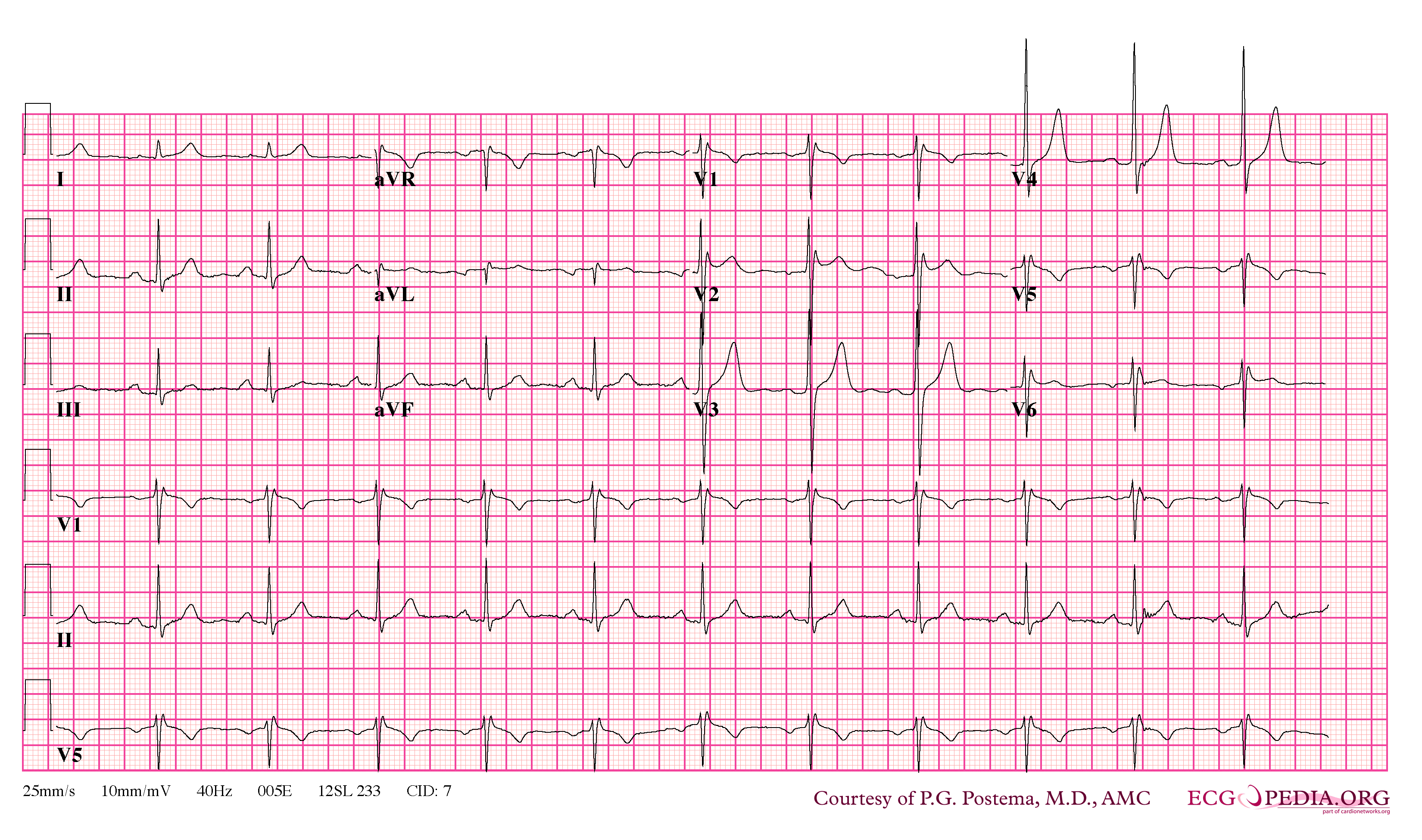
Shown below are examples of Brugada syndrome type 1 showing J point elevation, right bundle branch block and T wave inversion.
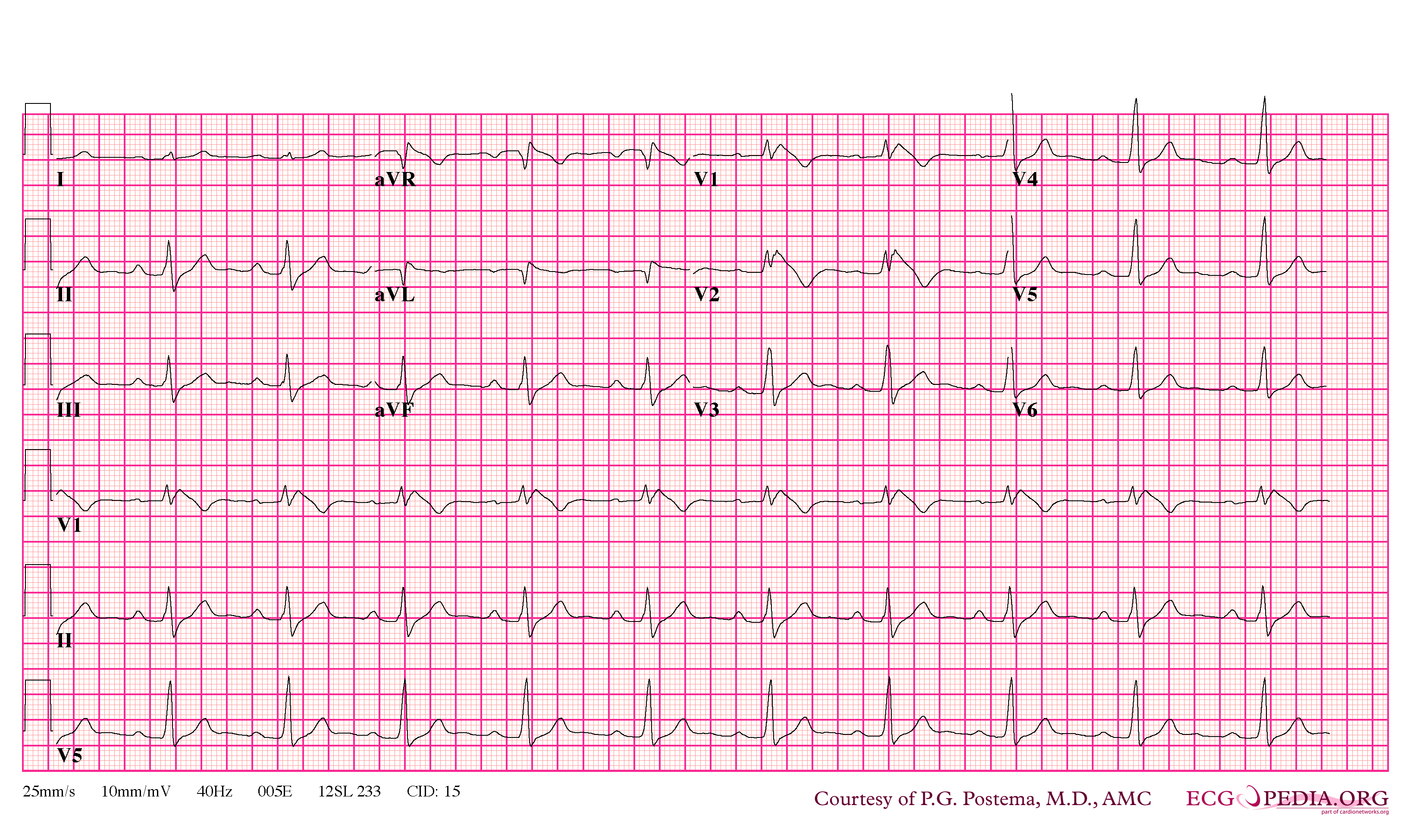

Shown below are examples of Brugada sydrome type 2 showing J point elevation, saddle shaped ST segment.
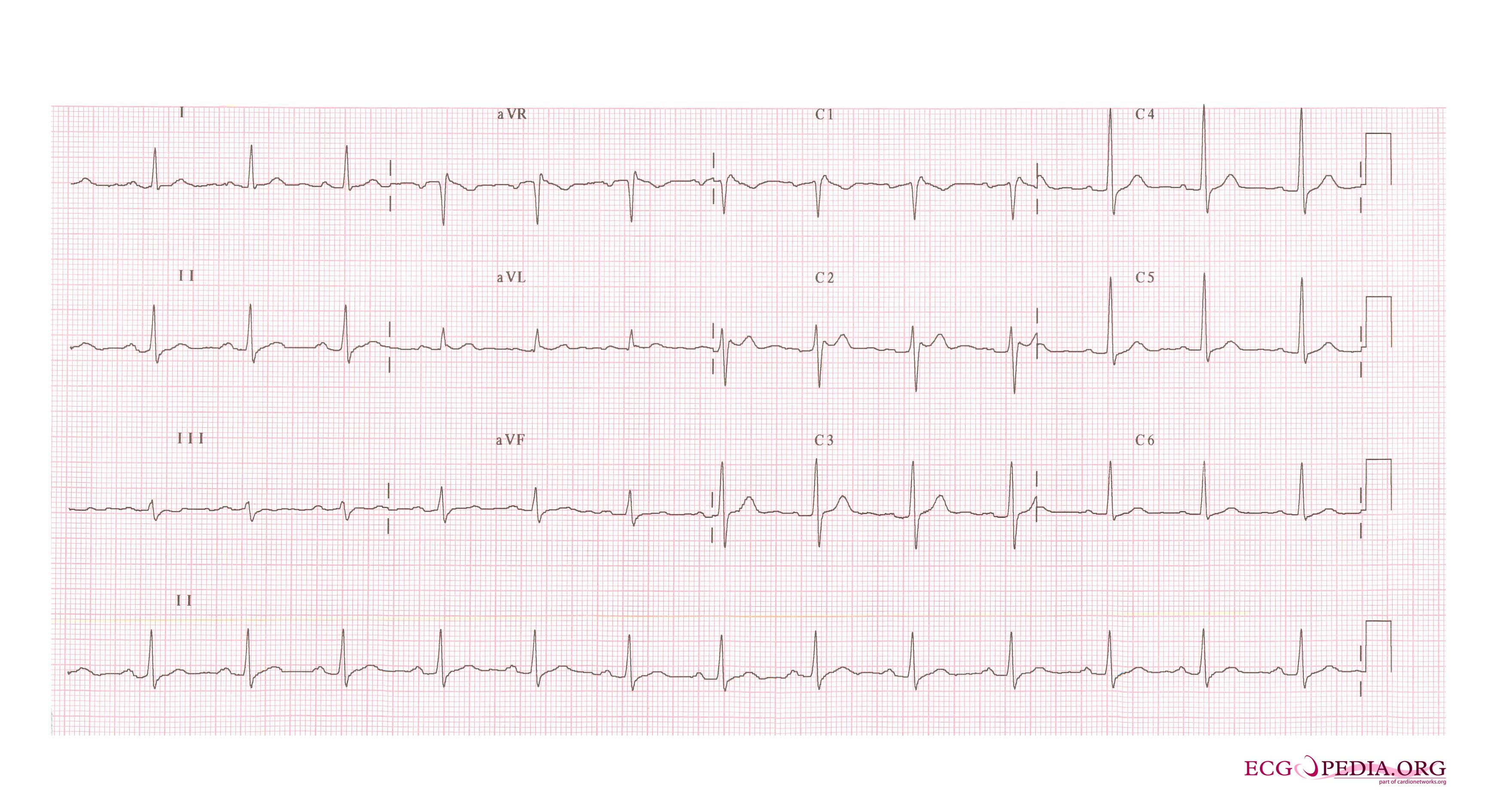

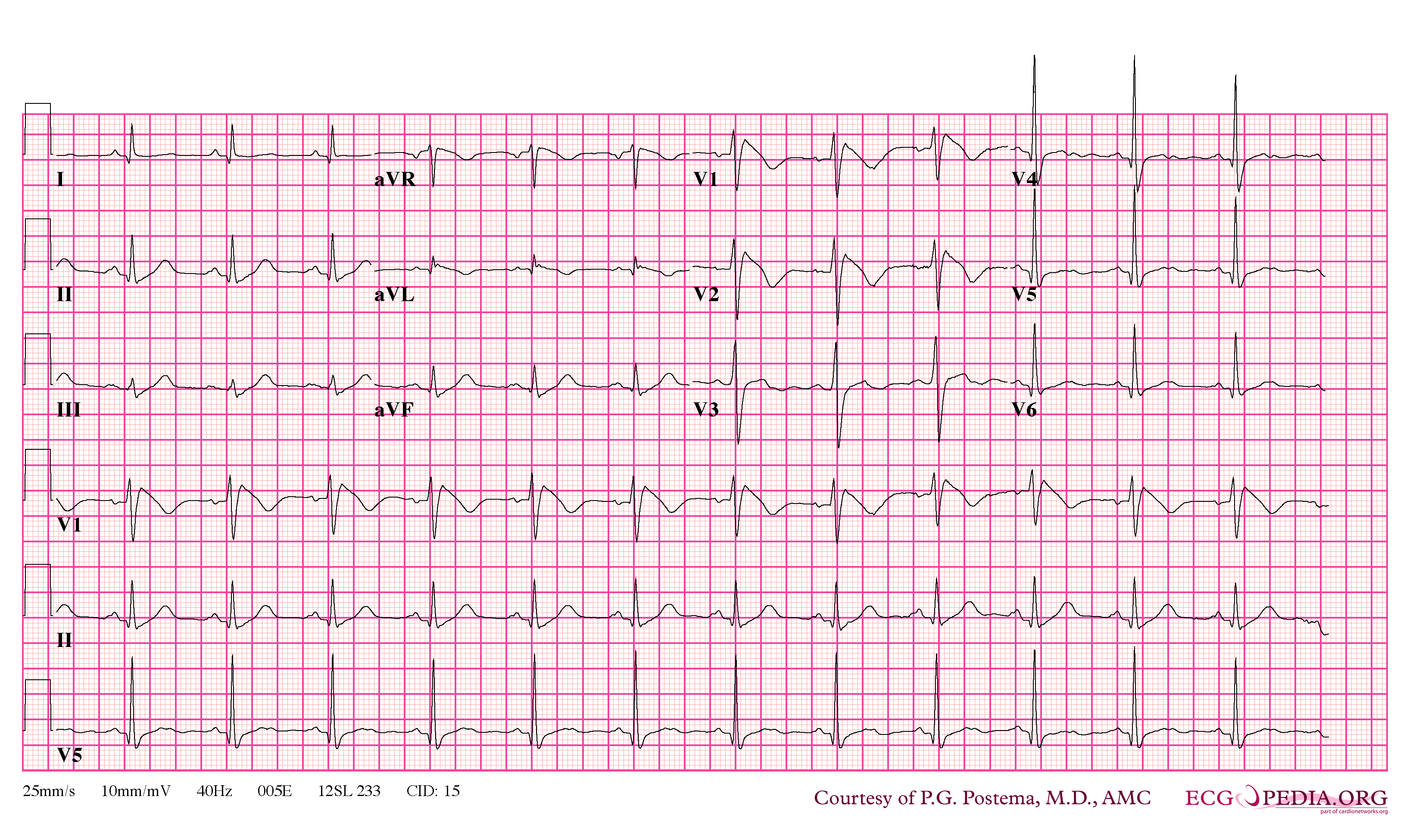
Shown below is an example of Brugada syndrome with right bundle branch block in V1 and St segment elevation in V1-3

References
- ↑ Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A (2005). "Brugada syndrome: report of the second consensus conference". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 2 (4): 429–40. PMID 15898165. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Kalla H, Yan GX, Marinchak R (2000). "Ventricular fibrillation in a patient with prominent J (Osborn) waves and ST segment elevation in the inferior electrocardiographic leads: a Brugada syndrome variant?". Journal of Cardiovascular Electrophysiology. 11 (1): 95–8. PMID 10695469. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Horigome H, Shigeta O, Kuga K, Isobe T, Sakakibara Y, Yamaguchi I, Matsui A (2003). "Ventricular fibrillation during anesthesia in association with J waves in the left precordial leads in a child with coarctation of the aorta". Journal of Electrocardiology. 36 (4): 339–43. PMID 14661171. Retrieved 2012-10-14. Unknown parameter
|month=ignored (help)