Endometrial cancer pathophysiology: Difference between revisions
No edit summary |
|||
| Line 3: | Line 3: | ||
{{CMG}} | {{CMG}} | ||
==Overview== | ==Overview== | ||
== | ==Pathophysiology== | ||
[[Image:Endometrial adenocarcinoma (1).jpg|thumb|left|Endometrial adenocarcinoma]] | [[Image:Endometrial adenocarcinoma (1).jpg|thumb|left|Endometrial adenocarcinoma]] | ||
====Microscopic pathology==== | ====Microscopic pathology==== | ||
Revision as of 02:46, 23 September 2012
|
Endometrial cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Endometrial cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Endometrial cancer pathophysiology |
|
Risk calculators and risk factors for Endometrial cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathophysiology
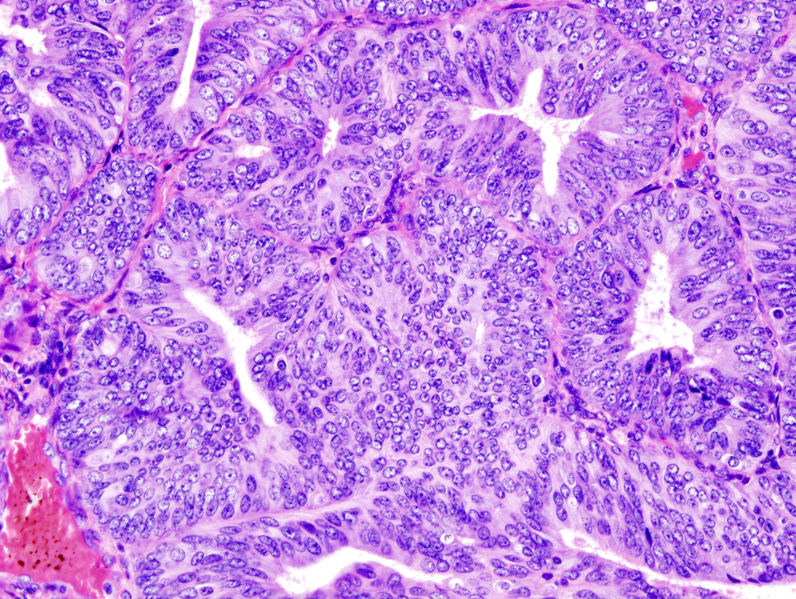
Microscopic pathology
The histopathology of endometrial cancers is highly diverse. The most common finding is a well-differentiated endometrioid adenocarcinoma, which is composed of numerous, small, crowded glands with varying degrees of nuclear atypia, mitotic activity, and stratification. This often appears on a background of endometrial hyperplasia. Frank adenocarcinoma may be distinguished from atypical hyperplasia by the finding of clear stromal invasion, or "back-to-back" glands which represent nondestructive replacement of the endometrial stroma by the cancer. With progression of the disease, the myometrium is infiltrated.[1]
References
- ↑ Richard Cote, Saul Suster, Lawrence Weiss, Noel Weidner (Editor). Modern Surgical Pathology (2 Volume Set). London: W B Saunders. ISBN 0-7216-7253-1.