Endometrial cancer natural history, complications and prognosis
|
Endometrial cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Endometrial cancer natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Endometrial cancer natural history, complications and prognosis |
|
FDA on Endometrial cancer natural history, complications and prognosis |
|
CDC on Endometrial cancer natural history, complications and prognosis |
|
Endometrial cancer natural history, complications and prognosis in the news |
|
Blogs on Endometrial cancer natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Monalisa Dmello, M.B,B.S., M.D. [2]
Overview
If left untreated, 8–30% of patients with atypical endometrial hyperplasia may progress to develop endometrial cancer. Common complications of endometrial cancer include menorrhagia and metastasis. Depending on the extent of the tumor at the time of diagnosis, the prognosis may vary. However, the prognosis is generally regarded as good.
Natural history
- If untreated, within ten years, 8–30% of atypical endometrial hyperplasia develop into cancer, whereas 1–3% of non-atypical hyperplasias do so.
- Patient has early symptoms like,abnormal vaginal bleeding, abnormal menstrual periods, metrorrhagia in premenopausal women, postmenopausal vaginal bleeding.
- As the tumor grows larger, patient may notice symptoms like, polyuria, dysuria, pelvic pain and dyspareunia, fatigue and unexplained weight loss.
- Once the diseases advances and spreads to other organs, the patient may present with dyspnea, cough with blood-stained sputum, persistent pain or discomfort in the chest, bilateral edema feet, itchiness, jaundice.
Complications
Complications of endometrial cancer include:
- Menorrhagia
- Metastasis - usually in the liver and lungs but may occur in other sites
Prognosis
Another factor found to correlate with extrauterine and nodal spread of tumor is involvement of the capillary-lymphatic space on histopathologic examination.
Three prognostic groupings of clinical stage I disease become possible by careful operative staging.
1. Patients with grade 1 tumors involving only endometrium and no evidence of intraperitoneal disease (i.e; adnexal spread) have a low risk (<5%) of nodal involvement.
2. Patients with grade 2 or 3 tumors and invasion of less than 50% of the myometrium and no intraperitoneal disease have a 5% to 9% incidence of pelvic node involvement and a 4% incidence of positive para-aortic nodes.
3. Patients with deep muscle invasion and high-grade tumors and/or intraperitoneal disease have a significant risk of nodal spread, 20% to 60% to pelvic nodes and 10% to 30% to para-aortic nodes.
The following four are statistically significant adverse prognostic factors:
- Myometrial invasion
- Vascular invasion
- Eight or more mitoses per ten high-power fields
- An absence of progesterone receptors
- Based on Gynecologic Oncology Group (GOG) study following are the other prognostic indicators of clinical outcome
- Oncogene expression
- DNA ploidy
- The fraction of cells in S-phase
- The following subtypes of endometrial cancer are associated with the poor prognosis:
- Clear cell endometrial carcinoma
- Serous endometrial carcinoma
- Squamous cell endometrial carcinoma
- Undifferentiated endometrial carcinomas
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with endometrial cancer was 83.2%.[1]
- When stratified by age, the 5-year relative survival of patients with endometrial cancer was 86.6% and 73.1% for patients <65 and ≥ 65 years of age respectively.[1]
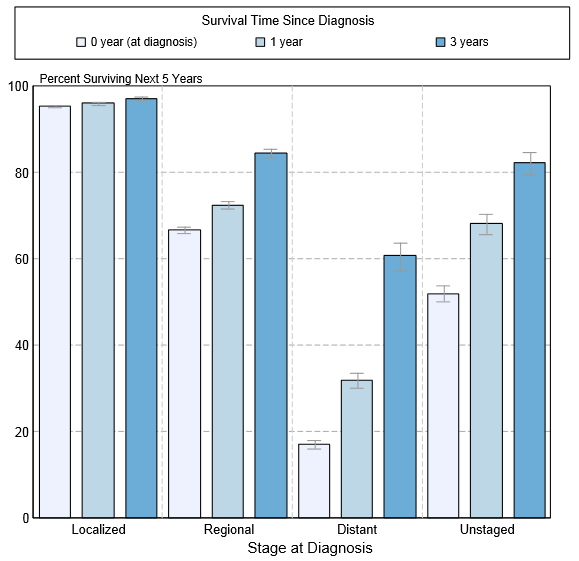
- The survival of patients with endometrial cancer varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of uterine cancer:[1]
| Stage | 5-year relative survival (%), (2004-2010) |
| All stages | 81.5% |
| Localized | 95.1% |
| Regional | 67.7% |
| Distant | 17,5% |
| Unstaged | 47.9% |
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of endometrial cancerby stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[1]
References
- ↑ 1.0 1.1 1.2 1.3 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.