|
|
| Line 12: |
Line 12: |
| MeshID = D009101 | | | MeshID = D009101 | |
| }} | | }} |
| {{SI}} | | {{Multiple myeloma}} |
| {{CMG}} | | {{CMG}} |
|
| |
|
| {{Editor Help}}
| | ==[[Multiple myeloma overview|Overview]]== |
|
| |
|
| ==Overview== | | ==[[Multiple myeloma historical perspective|Historical Perspective]]== |
|
| |
|
| '''Multiple myeloma''' (also known as '''MM''', '''myeloma''', '''plasma cell myeloma''', or as '''Kahler's disease''' after [[Otto Kahler]]) is a type of [[cancer]] of [[plasma cell]]s which are [[immune system]] cells in bone marrow that produce [[antibody|antibodies]]. Its [[prognosis]], despite therapy, is generally poor, and treatment may involve [[chemotherapy]] and [[stem cell transplant]]. It is part of the broad group of diseases called [[Hematological malignancy|hematological malignancies]].
| | ==[[Multiple myeloma pathophysiology|Pathophysiology]]== |
|
| |
|
| ==Clinical features== | | ==[[Multiple myeloma epidemiology and demographics|Epidemiology & Demographics]]== |
| Because many organs can be affected by myeloma, the symptoms and signs vary greatly. A [[mnemonic]] sometimes used to remember the common tetrad of multiple myeloma is ''CRAB'' - C = Calcium (elevated), R =Renal failure, A = Anemia, B = Bone lesions.<ref name="IMWG">International Myeloma Working Group. ''Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group.'' Br J Haematol 2003;121:749-57. PMID 12780789.</ref> Myeloma has many possible symptoms, and all symptoms may be due to other causes. They are presented here in decreasing order of incidence.
| |
|
| |
|
| ;Bone pain
| | ==[[Multiple myeloma risk factors|Risk Factors]]== |
| Myeloma bone pain usually involves the spine and ribs, and worsens with activity. Persistent localized pain may indicate a pathological [[bone fracture]]. Involvement of the vertebrae may lead to [[spinal cord compression]]. Myeloma bone disease is due to proliferation of tumor cells and release of [[Interleukin 6|IL-6]], also known as osteoclast activating factor (OAF), which stimulates [[osteoclast]]s to break down bone. These bone lesions are lytic in nature and are best seen in plain radiographs, which may show a "punched-out" resorptive lesions. The breakdown of bone also leads to release of [[calcium]] into the blood, leading to [[hypercalcemia]] and its associated symptoms.
| |
|
| |
|
| ;Infection
| | ==[[Multiple myeloma screening|Screening]]== |
| The most common infections are [[pneumonia]]s and [[pyelonephritis]]. Common pneumonia pathogens include ''[[streptococcus pneumoniae|S pneumoniae]]'', ''[[staphylococcus aureus|S aureus]]'', and ''[[klebsiella pneumoniae|K pneumoniae]]'', while common pathogens causing pyelonephritis include ''[[escherichia coli|E coli]]'' and other [[gram-negative]] organisms. The increased risk of infection is due to immune deficiency resulting from diffuse [[hypogammaglobulinemia]], which is due to decreased production and increased destruction of normal [[antibody|antibodies]].
| |
|
| |
|
| ;Renal failure
| | ==[[Multiple myeloma causes|Causes of Multiple myeloma]]== |
| [[Renal failure]] may develop both [[acute renal failure|acutely]] and [[chronic renal failure|chronically]]. It is commonly due to [[hypercalcemia]] (see above). It may also be due to tubular damage from excretion of [[light chain]]s, also called [[Bence Jones protein]]s, which can manifest as the [[Fanconi syndrome]] (type II [[renal tubular acidosis]]). Other causes include glomerular deposition of [[amyloid]], [[hyperuricemia]], recurrent infections ([[pyelonephritis]]), and local infiltration of tumor cells. | |
|
| |
|
| ;Anemia
| | ==[[Multiple myeloma differential diagnosis|Differentiating Multiple myeloma from other Diseases]]== |
| The [[anemia]] found in myeloma is usually normocytic and normochromic. It results from the replacement of normal bone marrow by infiltrating tumor cells and inhibition of normal red blood cell production ([[hematopoiesis]]) by [[cytokines]].
| |
|
| |
|
| ;Neurological symptoms
| | ==[[Multiple myeloma natural history|Natural History, Complications & Prognosis]]== |
| Common problems are weakness, confusion and fatigue due to [[hypercalcemia]]. [[Headache]], visual changes and [[retinopathy]] may be the result of hyperviscosity of the blood depending on the properties of the [[paraprotein]]. Finally, there may be [[radicular pain]], loss of bowel or bladder control (due to involvement of [[spinal cord]] leading to cord compression) or [[carpal tunnel syndrome]] and other [[neuropathies]] (due to infiltration of [[peripheral nerves]] by [[amyloid]]). It may give rise to [[paraplegia]] in late presenting cases.
| | |
| | ==[[Multiple myeloma staging|Staging]]== |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| ===Investigations===
| | [[Multiple myeloma history and symptoms|History & Symptoms]] | [[Multiple myeloma physical examination|Physical Examination]] | [[Multiple myeloma laboratory tests|Lab Tests]] | [[Multiple myeloma electrocardiogram|Electrocardiogram]] | [[Multiple myeloma chest x ray|Chest X Ray]] | [[Multiple myeloma CT|CT]] | [[Multiple myeloma MRI|MRI]] | [[Multiple myeloma echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Multiple myeloma other imaging findings|Other Imaging Findings]] | [[Multiple myeloma other diagnostic studies|Other Diagnostic Studies]] |
| | |
| The presence of unexplained [[anemia]], [[kidney]] dysfunction, a high [[erythrocyte sedimentation rate]] (ESR) and a high serum [[protein]] (especially raised [[immunoglobulin]]) may prompt further testing. A [[medical doctor|doctor]] will request [[protein electrophoresis]] of the blood and urine, which might show the presence of a [[paraprotein]] (monoclonal protein, or M protein) band, with or without reduction of the other (normal) immunoglobulins (known as immune paresis). One type of paraprotein is the [[Bence Jones protein]] which is a urinary paraprotein composed of free light chains (see below). Quantitative measurements of the paraprotein are necessary to establish a diagnosis and to monitor the disease. The paraprotein is an abnormal [[immunoglobulin]] produced by the tumor clone. Very rarely, the myeloma is ''nonsecretory'' (not producing immunoglobulins).
| |
| | |
| In theory, multiple myeloma can produce all classes of immunoglobulin, but IgG paraproteins are most common, followed by IgA and IgM. IgD and IgE myeloma are very rare. In addition, light and or heavy chains (the building blocks of antibodies) may be secreted in isolation: κ- or λ-light chains or any of the five types of heavy chains (α-, γ-, δ-, ε- or μ-heavy chains).
| |
| | |
| Additional findings include: a raised [[calcium]] (when [[osteoclasts]] are breaking down bone, releasing calcium into the bloodstream), raised serum creatinine due to reduced [[renal function]], which may be due to paraprotein deposition in the [[kidney]].
| |
| | |
| ==Diagnostic Findings==
| |
| | |
| ===MRI===
| |
| | |
| ([http://www.radswiki.net Images courtesy of RadsWiki])
| |
| | |
| <gallery>
| |
| Image:Multiple_myeloma_MRI101.jpg|Multiple myeloma
| |
| Image:Multiple_myeloma_MRI102.jpg|Multiple myeloma
| |
| Image:Multiple_myeloma_MRI103.jpg|Multiple myeloma
| |
| </gallery>
| |
| | |
| ===Pathology===
| |
| | |
| | |
| <gallery>
| |
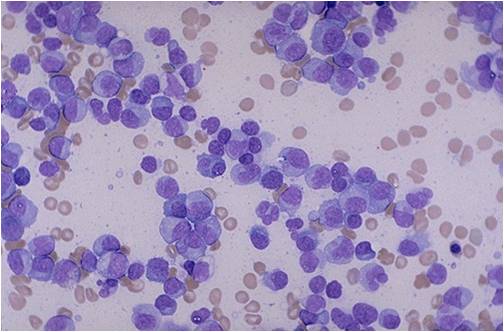
| Image:Multiple Myeloma.jpg|thumb|left|Multiple Myeloma <ref>http://picasaweb.google.com/mcmumbi/USMLEIIImages</ref>
| |
| Image:Vertebras in multiple myeloma 0001.jpg|thumb|left|Vertebras in multiple myeloma <br> (Image courtesy of Melih Aktan M.D.)
| |
| Image:Calvarium in multiple myeloma.jpg|thumb|left|Calvarium in multiple myeloma. <br> (Image courtesy of Melih Aktan M.D.)
| |
| Image:Bone marrow aspiration in multiple myeloma 0001.jpg|thumb|left|Bone marrow aspiration in multiple myeloma. <br> (Image courtesy of Melih Aktan M.D.)
| |
| Image:Bone marrow biopsy in multiple myeloma 0001.jpg|thumb|left|Bone marrow biopsy in multiple myeloma. <br> (Image courtesy of Melih Aktan M.D.)
| |
| Image:Bone marrow in multiple myeloma 0001.jpg|thumb|left|Bone marrow in multiple myeloma. <br> (Image courtesy of Melih Aktan M.D.)
| |
| Image:Bone marrow in multiple myeloma 0002.jpg|thumb|left|Bone marrow in multiple myeloma. <br> (Image courtesy of Melih Aktan M.D.)
| |
| </gallery>
| |
| | |
| ===Workup===
| |
| The workup of suspected multiple myeloma includes a [[skeletal survey]]. This is a series of [[X-ray]]s of the skull, axial skeleton and proximal long bones. Myeloma activity sometimes appear as "lytic lesions" (with local disappearance of normal bone due to resorption), and on the skull X-ray as "punched-out lesions" (pepper pot skull). [[Magnetic resonance imaging]] (MRI) is more sensitive than simple X-ray in the detection of lytic lesions, and may supersede skeletal survey, especially when vertebral disease is suspected. Occasionally a [[CT scan]] is performed to measure the size of soft tissue plasmacytomas.
| |
| | |
| A [[bone marrow biopsy]] is usually performed to estimate the percentage of bone marrow occupied by plasma cells. This percentage is used in the diagnostic criteria for myeloma. [[Immunohistochemistry]] (staining particular cell types using antibodies against surface proteins) can detect plasma cells which express immunoglobulin in the cytoplasm but usually not on the surface; myeloma cells are typically [[CD56]], [[CD38]], [[CD138]] positive and [[CD19]] and [[CD45]] negative.<ref name=IMWG /> [[Cytogenetics]] may also be performed in myeloma for prognostic purposes.
| |
| | |
| Other useful laboratory tests include quantitative measurement of [[IgA]], [[IgG]], [[IgM]] ([[immunoglobulin]]s) to look for immune paresis, and β2-microglobulin which provides prognostic information. On peripheral blood smear the rouleaux formation of red blood cells is commonly seen.
| |
| | |
| The recent introduction of a commercial immunoassay for measurement of free light chains potentially offers an improvement in monitoring disease progression and response to treatment, particularly where the paraprotein is difficult to measure accurately by electrophoresis (for example in light chain myeloma, or where the paraprotein level is very low). Initial research also suggests that measurement of free light chains may also be used, in conjunction with other markers, for assessment of the risk of progression from [[monoclonal gammopathy of undetermined significance]] (MGUS) to multiple myeloma.
| |
| | |
| ===Diagnostic criteria===
| |
| In 2003, the International Myeloma Working Group<ref name=IMWG /> agreed on diagnostic criteria for symptomatic myeloma, asymptomatic myeloma and [[monoclonal gammopathy of undetermined significance|MGUS]] (monoclonal gammopathy of undetermined significance):
| |
| | |
| * Symptomatic myeloma:
| |
| *# Clonal plasma cells >10% on [[bone marrow]] [[biopsy]] or (in any quantity) in a biopsy from other tissues ([[plasmacytoma]])
| |
| *# A [[monoclonal]] protein ([[paraprotein]]) in either [[blood plasma|serum]] or [[urine]]
| |
| *# Evidence of end-organ damage (''related organ or tissue impairment'', ROTI):
| |
| *#* [[Hypercalcemia]] (corrected calcium >2.75 mmol/L)
| |
| *#* [[Renal insufficiency]] attributable to myeloma
| |
| *#* [[Anemia]] (hemoglobin <10 g/dL)
| |
| *#* Bone [[lesions]] (lytic lesions or [[osteoporosis]] with compression fractures)
| |
| *#* Frequent severe [[infections]] (>2 a year)
| |
| *#* [[Amyloidosis]] of other organs
| |
| *#* [[Hyperviscosity syndrome]]
| |
| * Asymptomatic myeloma:
| |
| *# Serum paraprotein >30 g/L AND/OR
| |
| *# Clonal plasma cells >10% on bone marrow biopsy AND
| |
| *# NO myeloma-related organ or tissue impairment
| |
| * Monoclonal gammopathy of undetermined significance (MGUS):
| |
| *# Serum paraprotein <30 g/L AND/OR
| |
| *# Clonal plasma cells <10% on bone marrow biopsy AND
| |
| *# NO myeloma-related organ or tissue impairment
| |
| | |
| Related conditions include ''solitary [[plasmacytoma]]'' (a single tumor of plasma cells, typically treated with irradiation), ''plasma cell [[dyscrasia]]'' (where only the antibodies produce symptoms, e.g. AL [[amyloid|amyloidosis]]), and [[POEMS syndrome]] (peripheral neuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, skin changes).
| |
| | |
| ===Staging===
| |
| ;International Staging System
| |
| The International Staging System (ISS) for myeloma was published by the International Myeloma Working Group in 2003 <ref name="ISS">Greipp PR, San Miguel J, Fonseca R, Avet-Loiseau H, Jacobson JL, Rasmussen E, Crowley J, Durie BMG. Development of an international prognostic index (IPI) for myeloma: report of the international myeloma working group. ''Hematology Journal'' 2003;4:S42. NLM ID 100965523.</ref>:
| |
| * Stage I: [[beta-2-microglobulin|β<sub>2</sub>-microglobulin]] (β2M) < 3.5 mg/L, [[serum albumin|albumin]] >= 3.5 g/dL
| |
| * Stage II: β2M < 3.5 and albumin < 3.5; or β2M between 3.5 and 5.5
| |
| * Stage III: β2M > 5.5
| |
| | |
| ;Durie-Salmon staging system
| |
| First published in 1975, the Durie-Salmon staging system <ref name="Salmon">Durie BG, Salmon SE. A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment and survival. ''Cancer'' 1975;36:842–854. PMID 1182674.</ref> is still in use, but has largely been superseded by the simpler ISS:
| |
| * stage 1: all of
| |
| ** Hb > 10g/dL
| |
| ** normal calcium
| |
| ** Skeletal survey: normal or single plasmacytoma or osteoporosis
| |
| ** Serum paraprotein level < 5 g/dL if IgG, < 3 g/dL if IgA
| |
| ** Urinary light chain excretion < 4 g/24h
| |
| * stage 2: fulfilling the criteria of neither 1 nor 3
| |
| * stage 3: one or more of
| |
| ** Hb < 8.5g/dL
| |
| ** high calcium > 12mg/dL
| |
| ** Skeletal survey: 3 or more lytic bone lesions
| |
| ** Serum paraprotein >7g/dL if IgG, > 5 g/dL if IgA
| |
| ** Urinary light chain excretion > 12g/24h
| |
| | |
| Stages 1, 2 and 3 of the Durie-Salmon staging system can be divided into A or B depending on serum creatinine:
| |
| * A: serum creatinine < 2mg/dL (< 177 umol/L)
| |
| * B: serum creatinine > 2mg/dL (> 177 umol/L)
| |
| | |
| ==Pathophysiology==
| |
| Multiple myeloma develops in post-germinal center [[B lymphocytes]].
| |
| | |
| A [[chromosomal translocation]] between the immunoglobulin heavy chain gene (on the fourteenth [[chromosome]], locus 14q32) and an [[oncogene]] (often 11q13, 4p16.3, 6p21, 16q23 and 20q11<ref name="Kyle">Kyle RA, Rajkumar SV. ''Multiple myeloma.'' [[N Engl J Med]] 2004;351:1860-73. PMID 15509819.</ref>) is frequently observed in patients with multiple myeloma. This mutation results in dysregulation of the oncogene which is thought to be an important initiating event in the pathogenesis of myeloma. The result is proliferation of a plasma cell clone and genomic instability that leads to further mutations and translocations. The chromosome 14 abnormality is observed in about 50% of all cases of myeloma. Deletion of (parts of) the thirteenth chromosome is also observed in about 50% of cases.
| |
| | |
| Production of [[cytokine]]s (especially [[Interleukin 6|IL-6]]) by the plasma cells causes much of their localised damage, such as [[osteoporosis]], and creates a microenvironment in which the malignant cells thrive. [[Angiogenesis]] (the attraction of new blood vessels) is increased.
| |
| | |
| The produced antibodies are deposited in various organs, leading to renal failure, polyneuropathy and various other myeloma-associated symptoms.
| |
| | |
| ==Epidemiology==
| |
| There are approximately 45,000 people in the United States living with multiple myeloma, and the [[American Cancer Society]] estimates that approximately 14,600 new cases of myeloma are diagnosed each year in the United States. It follows from here that the average survival at diagnosis is about three years.
| |
| | |
| Multiple myeloma is the second most prevalent blood cancer (10%) after [[non-Hodgkin's lymphoma]]. It represents approximately 1% of all cancers and 2% of all cancer deaths. Although the peak age of onset of multiple myeloma is 65 to 70 years of age, recent statistics indicate both increasing incidence and earlier age of onset. | |
| | |
| Multiple myeloma affects slightly more men than women. African Americans and Native Pacific Islanders have the highest reported incidence of this disease in the United States and Asians the lowest. Results of a recent study found the incidence of myeloma to be 9.5 cases per 100,000 African Americans and 4.1 cases per 100,000 Caucasian Americans. Among African Americans, myeloma is one of the top 10 leading causes of cancer death.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| Treatment for multiple myeloma is focused on disease containment and suppression. If the disease is completely asymptomatic (i.e. there is a paraprotein and an abnormal bone marrow population but no end-organ damage), treatment may be deferred.
| | [[Multiple myeloma medical therapy|Medical Therapy]] | [[Multiple myeloma surgery|Surgery]] | [[Multiple myeloma primary prevention|Primary Prevention]] | [[Multiple myeloma secondary prevention|Secondary Prevention]] | [[Multiple myeloma cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Multiple myeloma future or investigational therapies|Future or Investigational Therapies]] |
| | |
| Although [[bone marrow transplant|allogeneic stem cell transplant]] might cure the cancer, it is considered investigational given the high treatment-related mortality of 5-10% associated with the procedure. In addition to direct treatment of the plasma cell proliferation, [[bisphosphonate]]s (e.g. [[pamidronate]] or [[zoledronic acid]]) are routinely administered to prevent fractures and [[erythropoietin]] to treat anemia.
| |
| | |
| ===Initial therapy===
| |
| Initial treatment is aimed at treating symptoms and reducing disease burden. Commonly used induction regimens include [[dexamethasone]] with or without [[thalidomide]] and [[cyclophosphamide]], and ''VAD'' ([[vincristine]], [[doxorubicin|adriamycin]], and dexamethasone). Low-dose therapy with [[melphalan]] combined with prednisone can be used to palliate symptoms in patients who cannot tolerate aggressive therapy. [[Plasmapheresis]] can be used to treat symptomatic protein proliferation ([[hyperviscosity syndrome]]).
| |
| | |
| In younger patients, therapy may include high-dose [[chemotherapy]], [[melphalan]], and ''[[bone marrow transplant|autologous stem cell transplantation]]''. This can be given in ''tandem'' fashion, i.e. an autologous transplant followed by a second transplant.
| |
| [[Bone marrow transplant#Conditioning Regimens|Nonmyeloablative (or "mini") allogeneic stem cell transplantation]] is being investigated as an alternative to autologous stem cell transplant, or as part of a tandem transplant following an autologous transplant (also known as an "auto-mini" tandem transplant). | |
| | |
| A 2007 trial indicated that the addition of thalidomide to reduced-intensity chemotherapy (melphalan and prednisone, MP) in patients between 65-75 led to a marked prolongation (median 51 versus 33 months) in survival. Reduced intensity melphalan followed by a stem cell transplant was inferior to the MP-thalidomide regimen (median survival 38 months).<ref>{{cite journal |author=Facon T, Mary JY, Hulin C ''et al'' |year=2007 |month= |title=Melphalan and prednisone plus thalidomide versus melphalan and prednisone alone or reduced-intensity autologous stem cell transplantation in elderly patients with multiple myeloma (IFM 99–06): a randomised trial |journal= Lancet|volume=370 |issue= |pages=1209-1218 |id=| url=http://www.thelancet.com/journals/lancet/article/PIIS0140673607615372/abstract | DOI=10.1016/S0140-6736(07)61537-2}}</ref>
| |
| | |
| ===Relapse===
| |
| The natural history of myeloma is of relapse following treatment. Depending on the patient's condition, the prior treatment modalities used and the duration of remission, options for relapsed disease include re-treatment with the original agent, use of other agents (such as melphalan, cyclophosphamide, thalidomide or dexamethasone, alone or in combination), and a second autologous stem cell transplant.
| |
| | |
| Later in the course of the disease, "treatment resistance" occurs. This may be a reversible effect,<ref name=Kyle /> and some new treatment modalities may re-sensitize the tumor to standard therapy. For patients with ''relapsed disease'', [[bortezomib]] (or Velcade®) is a recent addition to the therapeutic arsenal, especially as second line therapy. Bortezomib is a [[proteasome]] inhibitor. Finally, [[lenalidomide]] (or Revlimid®), a less toxic thalidomide analog, is showing promise for treating myeloma.
| |
| | |
| Renal failure in multiple myeloma can be [[acute renal failure|acute]] (reversible) or [[chronic renal failure|chronic]] (irreversible). Acute renal failure typically resolves when the calcium and paraprotein levels are brought under control. Treatment of chronic renal failure is dependent on the type of renal failure and may involve [[dialysis]].
| |
| | |
| ==Prognosis==
| |
| The [[#Staging|International Staging System]] can help to predict survival, with a median survival of 62 months for stage 1 disease, 45 months for stage 2 disease, and 29 months for stage 3 disease.<ref name=ISS />
| |
| | |
| [[Cytogenetic]] analysis of myeloma cells may be of [[prognosis|prognostic value]], with deletion of chromosome 13, non-hyperdiploidy and the balanced translocations t(4;14) and t(14;16) conferring a poorer prognosis. The 11q13 and 6p21 cytogenetic abnormalities are associated with a better prognosis. | |
| | |
| Prognostic markers such as these are always generated by retrospective analyses, and it is likely that new treatment developments will improve the outlook for those with traditionally 'poor-risk' disease.
| |
|
| |
|
| ==See also== | | ==See also== |
| Line 185: |
Line 49: |
| ==References== | | ==References== |
| {{Reflist|2}} | | {{Reflist|2}} |
|
| |
| ==External links==
| |
| * [http://www.myeloma.org.uk Myeloma UK]
| |
| * [http://www.myeloma.org International Myeloma Foundation]
| |
| * [http://www.multiplemyeloma.org Multiple Myeloma Research Foundation]
| |
| * [http://www.mmsupport.net/ MM Support Network]
| |
| * [http://www.myeloma-euronet.org Myeloma Euronet] - European Network of Myeloma Patient Groups
| |
| * [http://www.leukemia-lymphoma.org/all_page?item_id=7032 The Leukemia & Lymphoma Society's Myeloma Page]
| |
|
| |
|
| |
|
| {{Hematological malignancy histology}} | | {{Hematological malignancy histology}} |
| {{SIB}}
| |
| [[ar:ورم نقوي متعدد]]
| |
| [[de:Multiples Myelom]]
| |
| [[es:Mieloma múltiple]]
| |
| [[fr:Myélome multiple]]
| |
| [[he:מיאלומה נפוצה]]
| |
| [[nl:Ziekte van Kahler]]
| |
| [[ja:多発性骨髄腫]]
| |
| [[pt:Mieloma múltiplo]]
| |
| [[sv:Myelom]]
| |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| Line 214: |
Line 59: |
| [[Category:Types of cancer]] | | [[Category:Types of cancer]] |
| [[Category:Oncology]] | | [[Category:Oncology]] |
| [[Category:Mature chapter]]
| |