Pharyngitis overview: Difference between revisions
| Line 102: | Line 102: | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
There is broad overlap between the signs and symptoms of streptococcal and non-streptococcal (usually viral) pharyngitis, and the ability to identify streptococcal pharyngitis accurately on the basis of clinical grounds alone is generally poor.<ref name="pmid5056872">Wannamaker LW (1972) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=5056872 Perplexity and precision in the diagnosis of streptococcal pharyngitis.] ''Am J Dis Child'' 124 (3):352-8. PMID: [https://pubmed.gov/5056872 5056872]</ref><ref name="pmid855837">Breese BB (1977) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=855837 A simple scorecard for the tentative diagnosis of streptococcal pharyngitis.] ''Am J Dis Child'' 131 (5):514-7. PMID: [https://pubmed.gov/855837 855837]</ref><ref name="pmid15069046">McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE (2004) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=15069046 Empirical validation of guidelines for the management of pharyngitis in children and adults.] ''JAMA'' 291 (13):1587-95. [http://dx.doi.org/10.1001/jama.291.13.1587 DOI:10.1001/jama.291.13.1587] PMID: [https://pubmed.gov/15069046 15069046]</ref> Therefore, except when obvious viral clinical and epidemiological features are present, a laboratory test should be performed to determine whether GAS is present in the pharynx.<ref name="pmid8637780">Bisno AL (1996) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=8637780 Acute pharyngitis: etiology and diagnosis.] ''Pediatrics'' 97 (6 Pt 2):949-54. PMID: [https://pubmed.gov/8637780 8637780]</ref><ref name="pmid15069046">McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE (2004) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=15069046 Empirical validation of guidelines for the management of pharyngitis in children and adults.] ''JAMA'' 291 (13):1587-95. [http://dx.doi.org/10.1001/jama.291.13.1587 DOI:10.1001/jama.291.13.1587] PMID: [https://pubmed.gov/15069046 15069046]</ref> Even subjects with all clinical features in a particular scoring system can be confirmed to have streptococcal pharyngitis only about 35%–50% of the time, and this is particularly the case in children.<ref name="pmid855837">Breese BB (1977) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=855837 A simple scorecard for the tentative diagnosis of streptococcal pharyngitis.] ''Am J Dis Child'' 131 (5):514-7. PMID: [https://pubmed.gov/855837 855837]</ref> Swabbing the throat and testing for GAS pharyngitis with RADT&/ culture should be performed because the clinical features alone do not reliably discriminate between GAS and viral pharyngitis except when overt viral features like rhinorrhea, cough, oral ulcers, and/or hoarseness are present. | There is broad overlap between the signs and symptoms of streptococcal and non-streptococcal (usually viral) pharyngitis, and the ability to identify streptococcal pharyngitis accurately on the basis of clinical grounds alone is generally poor.<ref name="pmid5056872">Wannamaker LW (1972) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=5056872 Perplexity and precision in the diagnosis of streptococcal pharyngitis.] ''Am J Dis Child'' 124 (3):352-8. PMID: [https://pubmed.gov/5056872 5056872]</ref><ref name="pmid855837">Breese BB (1977) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=855837 A simple scorecard for the tentative diagnosis of streptococcal pharyngitis.] ''Am J Dis Child'' 131 (5):514-7. PMID: [https://pubmed.gov/855837 855837]</ref><ref name="pmid15069046">McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE (2004) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=15069046 Empirical validation of guidelines for the management of pharyngitis in children and adults.] ''JAMA'' 291 (13):1587-95. [http://dx.doi.org/10.1001/jama.291.13.1587 DOI:10.1001/jama.291.13.1587] PMID: [https://pubmed.gov/15069046 15069046]</ref> Therefore, except when obvious viral clinical and epidemiological features are present, a laboratory test should be performed to determine whether GAS is present in the pharynx.<ref name="pmid8637780">Bisno AL (1996) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=8637780 Acute pharyngitis: etiology and diagnosis.] ''Pediatrics'' 97 (6 Pt 2):949-54. PMID: [https://pubmed.gov/8637780 8637780]</ref><ref name="pmid15069046">McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE (2004) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=15069046 Empirical validation of guidelines for the management of pharyngitis in children and adults.] ''JAMA'' 291 (13):1587-95. [http://dx.doi.org/10.1001/jama.291.13.1587 DOI:10.1001/jama.291.13.1587] PMID: [https://pubmed.gov/15069046 15069046]</ref> Even subjects with all clinical features in a particular scoring system can be confirmed to have streptococcal pharyngitis only about 35%–50% of the time, and this is particularly the case in children.<ref name="pmid855837">Breese BB (1977) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=855837 A simple scorecard for the tentative diagnosis of streptococcal pharyngitis.] ''Am J Dis Child'' 131 (5):514-7. PMID: [https://pubmed.gov/855837 855837]</ref> Swabbing the throat and testing for GAS pharyngitis with RADT&/ culture should be performed because the clinical features alone do not reliably discriminate between GAS and viral pharyngitis except when overt viral features like rhinorrhea, cough, oral ulcers, and/or hoarseness are present. | ||
The rapid streptococcal antigen tests are widely available and have been used and studied extensively as an adjunct to making the diagnosis of GAS pharyngitis. Specificity for the test has been reported to be as high as 95%, with a sensitivity of 80% to 90%.38 Throat cultures are much more sensitive, between 90% and 95%; however, they require up to 48 hours for results. | |||
A test negative for GAS provides reassurance that the patient likely has a viral cause of pharyngitis. A negative test result also allows the clinician to safely avoid the use of antibiotics. Because of the general increase in rates of resistance to antibiotics, antimicrobial therapy should be prescribed only for proven episodes of GAS pharyngitis.<ref name="pmid12087516">Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH, Infectious Diseases Society of America (2002) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=12087516 Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America.] ''Clin Infect Dis'' 35 (2):113-25. [http://dx.doi.org/10.1086/340949 DOI:10.1086/340949] PMID: [https://pubmed.gov/12087516 12087516]</ref><ref name="pmid11255529">Snow V, Mottur-Pilson C, Cooper RJ, Hoffman JR, American Academy of Family Physicians. American College of Physicians-American Society of Internal Medicine et al. (2001) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=11255529 Principles of appropriate antibiotic use for acute pharyngitis in adults.] ''Ann Intern Med'' 134 (6):506-8. PMID: [https://pubmed.gov/11255529 11255529]</ref> | A test negative for GAS provides reassurance that the patient likely has a viral cause of pharyngitis. A negative test result also allows the clinician to safely avoid the use of antibiotics. Because of the general increase in rates of resistance to antibiotics, antimicrobial therapy should be prescribed only for proven episodes of GAS pharyngitis.<ref name="pmid12087516">Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH, Infectious Diseases Society of America (2002) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=12087516 Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America.] ''Clin Infect Dis'' 35 (2):113-25. [http://dx.doi.org/10.1086/340949 DOI:10.1086/340949] PMID: [https://pubmed.gov/12087516 12087516]</ref><ref name="pmid11255529">Snow V, Mottur-Pilson C, Cooper RJ, Hoffman JR, American Academy of Family Physicians. American College of Physicians-American Society of Internal Medicine et al. (2001) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=11255529 Principles of appropriate antibiotic use for acute pharyngitis in adults.] ''Ann Intern Med'' 134 (6):506-8. PMID: [https://pubmed.gov/11255529 11255529]</ref> | ||
Revision as of 21:02, 3 January 2017
|
Pharyngitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pharyngitis overview On the Web |
|
American Roentgen Ray Society Images of Pharyngitis overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Venkata Sivakrishna Kumar Pulivarthi M.B.B.S [2]
Synonyms and keywords: Sore throat; Group A streptococcal pharyngitis; Bacterial pharyngitis; Viral pharyngitis.
Overview
Pharyngitis is the inflammation of the pharynx, manifested by sore throat. It is a painful inflammation of the pharynx, and is colloquially referred to as a sore throat. [1] Pharyngitis is a common medical problem in the outpatient medical setting, resulting in more than seven million pediatric visits each year. Most types of pharyngitis are caused by infectious etiologies. The most common cause of pharyngitis is viral infection. However, some of the more serious types of pharyngitis are attributed to bacterial etiologies, such as group A-hemolytic Streptococcus pyogenes (GAS). Complications from GAS pharyngitis include rheumatic fever, deep space abscesses, and toxic shock. Although most episodes of pharyngitis are acute in nature, a small percentage becomes recurrent or chronic. With regards to chronic pharyngitis, non-infectious etiologies, such as laryngopharyngeal reflux and periodic fever, aphthous ulcers, pharyngitis, and adenitis syndrome also need to be considered. Both medical and surgical therapies are effective in managing pharyngitis. First-line medical therapy includes antibiotic therapy. For certain indications, surgical management via adenotonsillectomy is recommended. Adenotonsillectomy has been shown to be effective in reducing disease burden and improving disease-specific and global quality of life. Several techniques for adenotonsillectomy exist, including traditional and intracapsular tonsillectomies.[2]
Historical Prospective
Pathophysiology
Causes
Classification
Differential Diagnosis
Epidemiology and Demographics
Pharyngitis is one of the most common disorders in adults and children, with more than 10 million ambulatory visits per year.[3] Viruses are the single most common cause of pharyngitis and account for 25% to 45% of all cases.[4] Group A streptococcus presents in up to 37% of all children presenting with a sore throat to an outpatient clinic or ED and 24% of those presenting at younger than 5 years.[5] Group A streptococcus is by far the most common bacterial cause of acute pharyngitis, accounting for approximately 15 to 30 percent of cases in children and 5 to 10 percent of cases in adults.[6] Peak seasons for sore throat include late winter and early spring.
Risk Factors
Pharyngitis is contagious, so anyone in close proximity to someone with the illness, is at risk. Social situations with prolonged close interpersonal contact are associated with a higher incidence of the disease, such as in schools, dormitories, or military barracks. Other common risk factors include History of ill contact, Over crowding, Frequent sinus infections, Smoking, Attending day care, Immunocompromised etc.
Natural History, Complications & Prognosis
Acute pharyngitis is typically described as the triad of sore throat, fever, and pharyngeal inflammation characterized by erythema and edema, although exudates, vesicles, or ulcerations may also be present. Although pharyngitis may be a primary disorder, sore throat and pharyngeal erythema may also be prominent in systemic disorders, such as the acute retroviral syndrome, or part of a more generalized upper respiratory tract infection. Most cases of acute pharyngitis are due to common viral infections and are benign, self-limited processes. The appropriate recognition of patients with more complicated infections that require diagnostic evaluations and treatment is one of the challenges of primary care medicine.[7] An estimated 1-2% of acute pharyngitis progresses to recurrent or chronic disease.[8]
Diagnosis
Key points in the evaluation of acute pharyngitis
- Essential to diagnosis is the identification of treatable causes (e.g. Group A streptococcus) to prevent complications.s[9]
- Signs and symptoms of GAS pharyngitis include acute onset of sore throat with tonsillar or pharyngeal exudates, tender anterior cervical lymphadenopathy and fever.
- Signs and symptoms consistent with viral etiologies include conjunctivitis, coryza, oral ulcers, cough, and diarrhea.
- Testing for GAS pharyngitis should not be pursued in those with signs and symptoms indicative of a viral etiology.
- Rapid antigen detection tests (RADTs) alone are sufficient for the diagnosis of GAS in adults, but negative results should be backed up by throat culture in children.
- Specific techniques should be used to identify other causes where appropriate.
Guidelines Comparison for the Management of Acute Pharyngitis
| Recommendation | American College of Physicians | Infectious Diseases Society of America |
|---|---|---|
| Screening for acute pharyngitis | Use Centor criteria | Use clinical and epidemiologic findings to assess patient’s risk of GABHS (e.g., sudden onset of sore throat, fever, odynophagia, tonsillar erythema, exudates, cervical lymphadenitis, or history of streptococcal exposure) |
| Diagnostic testing | RADT with Centor score of 2 or 3 only | RADT or throat culture in all patients at risk |
| Back-up culture needed if RADT result negative? | Adults: No
Children: Yes |
Adults: No
Children: Yes |
| Who requires antibiotic treatment? | Empiric antibiotics for Centor score of 3 or 4; treat patients with positive RADT result | Positive RADT result or throat culture |
| Antibiotic of choice | Oral penicillin V (Veetids; brand no longer available in the United States); intramuscular penicillin G benzathine (Bicillin L-A); oral amoxicillin with equal effectiveness and better palatability in children | |
| Penicillin allergy | Oral erythromycin; cephalosporin (first generation) | |
History and Symptoms
Pharyngitis is a very common inflammatory condition of the pharynx accompanied by a sore throat and occasionally difficulty in swallowing.[10] Other symptoms depends on the etiology such as bacterial or viral.[2]
| Clinical features of acute pharyngitis | |
|---|---|
| Group A streptococcal pharyngitis | Viral pharyngitis |
|
|
Physical Examination
Laboratory Findings
There is broad overlap between the signs and symptoms of streptococcal and non-streptococcal (usually viral) pharyngitis, and the ability to identify streptococcal pharyngitis accurately on the basis of clinical grounds alone is generally poor.[11][12][13] Therefore, except when obvious viral clinical and epidemiological features are present, a laboratory test should be performed to determine whether GAS is present in the pharynx.[14][13] Even subjects with all clinical features in a particular scoring system can be confirmed to have streptococcal pharyngitis only about 35%–50% of the time, and this is particularly the case in children.[12] Swabbing the throat and testing for GAS pharyngitis with RADT&/ culture should be performed because the clinical features alone do not reliably discriminate between GAS and viral pharyngitis except when overt viral features like rhinorrhea, cough, oral ulcers, and/or hoarseness are present.
The rapid streptococcal antigen tests are widely available and have been used and studied extensively as an adjunct to making the diagnosis of GAS pharyngitis. Specificity for the test has been reported to be as high as 95%, with a sensitivity of 80% to 90%.38 Throat cultures are much more sensitive, between 90% and 95%; however, they require up to 48 hours for results.
A test negative for GAS provides reassurance that the patient likely has a viral cause of pharyngitis. A negative test result also allows the clinician to safely avoid the use of antibiotics. Because of the general increase in rates of resistance to antibiotics, antimicrobial therapy should be prescribed only for proven episodes of GAS pharyngitis.[15][16]
Rapid Antigen Detection Test (RADT)
RADT is useful for the identification of GAS pharyngitis directly from throat swabs. RADTs currently available are highly specific (approximately 95%) when compared with blood agar plate cultures.[17]
Centor criteria
The original Centor score uses four signs and symptoms to estimate the probability of acute streptococcal pharyngitis in adults with a sore throat.[18] The score was later modified by adding age.[19] It is important to evaluate for definitive diagnosis to exclude GAS and to avoid unnecessary lab tests and antibiotic use. Centor criteria are a widely used and accepted clinical decision tool in identifying patients for whom neither microbiologic tests nor antimicrobial therapy are necessary.The Centor score to use for children and adults with a sore throat to estimate probability of Streptococcus pyogenes infection.[20][21]
| Modified Centor criteria | Appropriate management according to the total score | ||||
| Criteria | Points | Total score | Chance of streptococcal infection in community
with usual levels of infection, % |
Suggested management | |
| Fever (temperature > 38°C) | +1 | 0 | 2-3% | No culture or antibiotic is required | |
| Absence of cough | +1 | 1 | 4-6% | ||
| Swollen and tender anterior cervical nodes | +1 | 2 | 10-12% | RADT or Culture and treat only if culture result is positive | |
| Tonsillar swelling or exudates | +1 | 3 | 27-28% | ||
| Age 3–14 yr | +1 | 4 | 38–63% | Culture all and treat emperically with penicillin on clinical grounds | |
| Age 15–44 yr | 0 | ||||
| Age ≥ 45 yr | -1 | ||||
Special Considerations in the Diagnosis of Acute Pharyngitis in Adults
GAS causes only 5%–15% of cases of acute pharyngitis in adults.[14] The risk of acute pharyngitis due to GAS among adults is higher for parents of school-age children and for those whose occupation brings them into close association with children. However, the risk of a first attack of ARF is extremely low in adults, even with an undiagnosed and untreated episode of streptococcal pharyngitis. Because of these epidemiological distinctions, the use of a clinical algorithm without microbiological confirmation has been suggested as an acceptable alternative basis for diagnosis of infection in adults.[16][22] However, use of this diagnostic strategy would result in treatment of an unacceptably large number of adults with non-streptococcal pharyngitis, that is an undesirable result in this age group, which has a low prevalence of GAS pharyngitis and a very low risk of rheumatic fever or rheumatic carditis. However, routine use of back-up throat cultures for those with a negative RADT is not necessary for adults in usual circumstances, because of the low incidence of GAS pharyngitis in adults and because the risk of subsequent acute rheumatic fever is generally exceptionally low in adults with acute pharyngitis.[16]
Special Considerations in the Diagnosis of Acute Pharyngitis in Children <3 Years
The prevalence of GAS pharyngitis is significantly lower for children <3 years of age, ranging from 10% to 14%, and if a corresponding rise in ASO is required, the prevalence can be as low as 0%– 6%.[23][24] Thus, diagnostic testing for GAS pharyngitis is not routinely indicated in children <3 years of age. However, if a child is <3 years of age and there is household contact with a school-aged sibling with documented streptococcal pharyngitis, then it is reasonable to consider testing the child if the child is symptomatic. Therefore, if a child is in day care or another setting with a high rate of cases of GAS infections, then it is reasonable to test symptomatic children and treat them if they are found to be positive for GAS.
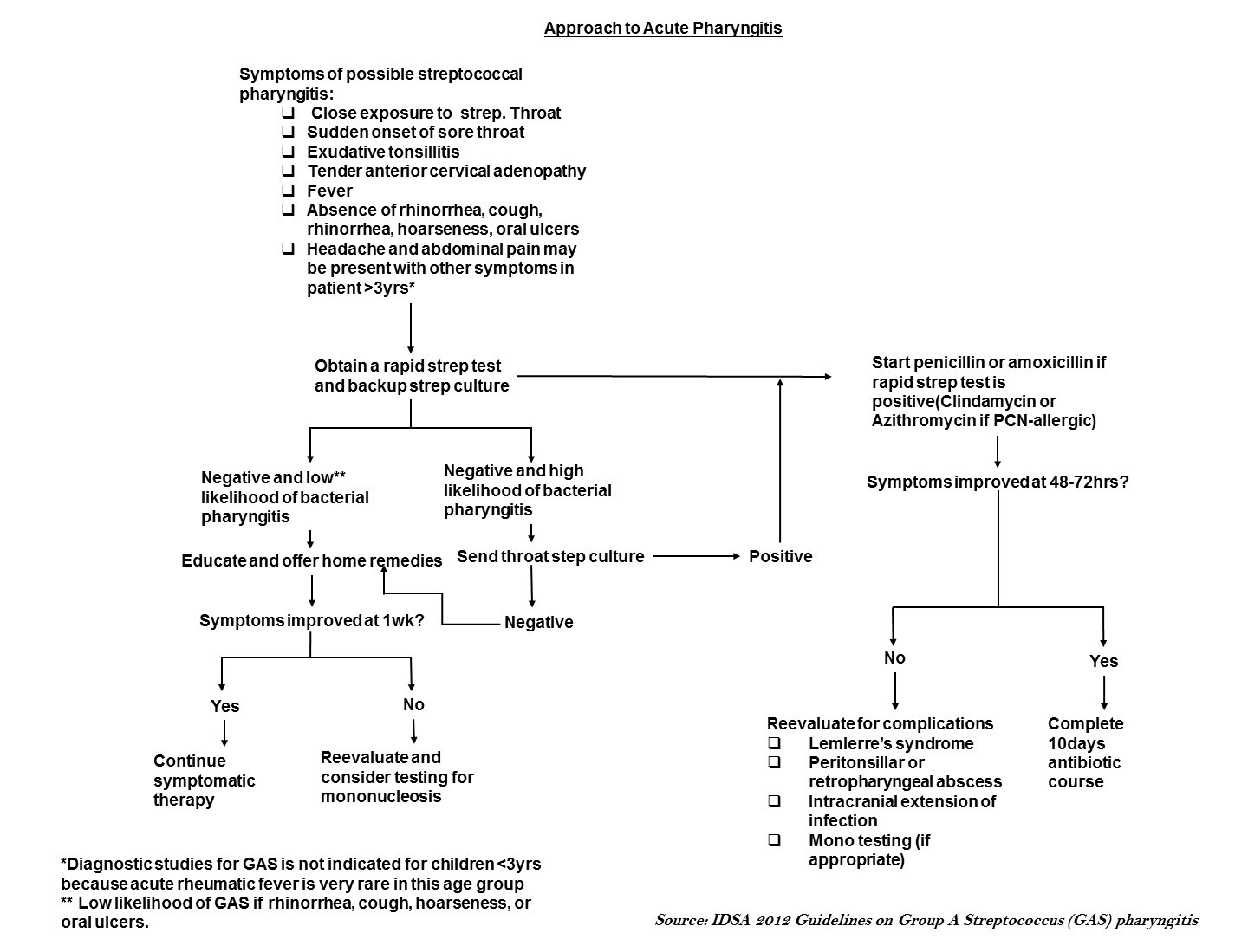
Evaluation of acute pharyngitis
The major goal of the evaluation of patients with sore throat or acute pharyngitis is to exclude potentially dangerous causes (e.g. Group A streptococcus), to identify any treatable causes, and to improve symptoms. Identifying group A streptococcus (GAS) is important because timely treatment with antibiotics helps prevent poststreptococcal complications such as acute rheumatic fever.[25] The evaluation includes a thorough history, focused physical examination, and diagnostic testing in selected patients.
Treatment
As is evident from potential etiologic agents of pharyngitis, group A streptococcus is the only commonly occurring form of acute pharyngitis for which antibiotic therapy is definitely indicated. Therefore, for a patient with acute pharyngitis, the clinical decision that usually needs to be made is whether or not the pharyngitis is attributable to GAS.[2]
Medical Therapy
Patients with acute GAS pharyngitis should be treated with an appropriate antibiotic at an appropriate dose for a duration likely to eradicate the organism from the pharynx (usually 10 days). Based on their narrow spectrum of activity, infrequency of adverse reactions, and modest cost, penicillin or amoxicillin is the recommended drug of choice for those non-allergic to these agents.[2] Treatment of GAS pharyngitis in penicillin-allergic individuals should include a first generation cephalosporin (for those not anaphylactically sensitive) for 10 days, clindamycin or clarithromycin for 10 days, or azithromycin for 5 days. Adjunctive therapy with Nonsteroidal Anti-inflammatory Drugs (NSAIDs), Acetaminophen, Aspirin, or Corticosteroids may be useful in the management of GAS pharyngitis.
Surgery
Prevention
Accurate diagnosis of streptococcal pharyngitis followed by appropriate antimicrobial therapy is important for the prevention of acute rheumatic fever and for the prevention of suppurative complications such as Peritonsillar abscess, cervical lymphadenitis, mastoiditis.[2]
References
- ↑ Acute Pharyngitis - Get Smart: Know When Antibiotics Work. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/getsmart/community/materials-references/print-materials/hcp/adult-acute-pharyngitis.html July 28, 2016
- ↑ 2.0 2.1 2.2 2.3 2.4 Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G et al. (2012) Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 55 (10):1279-82. DOI:10.1093/cid/cis847 PMID: 23091044
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ Cirilli AR (2013) Emergency evaluation and management of the sore throat. Emerg Med Clin North Am 31 (2):501-15. DOI:10.1016/j.emc.2013.01.002 PMID: 23601485
- ↑ Bisno AL (2001) Acute pharyngitis. N Engl J Med 344 (3):205-11. DOI:10.1056/NEJM200101183440308 PMID: 11172144
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ St Sauver JL, Weaver AL, Orvidas LJ, Jacobson RM, Jacobsen SJ (2006) Population-based prevalence of repeated group A beta-hemolytic streptococcal pharyngitis episodes. Mayo Clin Proc 81 (9):1172-6. PMID: 16970213
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ Cohen, J (2010). Infectious diseases. Edinburgh: Mosby/Elsevier. ISBN 978-0323045797.
- ↑ Wannamaker LW (1972) Perplexity and precision in the diagnosis of streptococcal pharyngitis. Am J Dis Child 124 (3):352-8. PMID: 5056872
- ↑ 12.0 12.1 Breese BB (1977) A simple scorecard for the tentative diagnosis of streptococcal pharyngitis. Am J Dis Child 131 (5):514-7. PMID: 855837
- ↑ 13.0 13.1 McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE (2004) Empirical validation of guidelines for the management of pharyngitis in children and adults. JAMA 291 (13):1587-95. DOI:10.1001/jama.291.13.1587 PMID: 15069046
- ↑ 14.0 14.1 Bisno AL (1996) Acute pharyngitis: etiology and diagnosis. Pediatrics 97 (6 Pt 2):949-54. PMID: 8637780
- ↑ Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH, Infectious Diseases Society of America (2002) Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America. Clin Infect Dis 35 (2):113-25. DOI:10.1086/340949 PMID: 12087516
- ↑ 16.0 16.1 16.2 Snow V, Mottur-Pilson C, Cooper RJ, Hoffman JR, American Academy of Family Physicians. American College of Physicians-American Society of Internal Medicine et al. (2001) Principles of appropriate antibiotic use for acute pharyngitis in adults. Ann Intern Med 134 (6):506-8. PMID: 11255529
- ↑ Gerber MA (1989) Comparison of throat cultures and rapid strep tests for diagnosis of streptococcal pharyngitis. Pediatr Infect Dis J 8 (11):820-4. PMID: 2687791
- ↑ Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K (1981) The diagnosis of strep throat in adults in the emergency room. Med Decis Making 1 (3):239-46. PMID: 6763125
- ↑ McIsaac WJ, Goel V, To T, Low DE (2000) The validity of a sore throat score in family practice. CMAJ 163 (7):811-5. PMID: 11033707
- ↑ Anjos LM, Marcondes MB, Lima MF, Mondelli AL, Okoshi MP (2014) Streptococcal acute pharyngitis. Rev Soc Bras Med Trop 47 (4):409-13. PMID: 25229278
- ↑ Choby BA (2009) Diagnosis and treatment of streptococcal pharyngitis. Am Fam Physician 79 (5):383-90. PMID: 19275067
- ↑ Humair JP, Revaz SA, Bovier P, Stalder H (2006) Management of acute pharyngitis in adults: reliability of rapid streptococcal tests and clinical findings. Arch Intern Med 166 (6):640-4. DOI:10.1001/archinte.166.6.640 PMID: 16567603
- ↑ Nussinovitch M, Finkelstein Y, Amir J, Varsano I (1999) Group A beta-hemolytic streptococcal pharyngitis in preschool children aged 3 months to 5 years. Clin Pediatr (Phila) 38 (6):357-60. PMID: 10378093
- ↑ Amir J, Shechter Y, Eilam N, Varsano I (1994) Group A beta-hemolytic streptococcal pharyngitis in children younger than 5 years. Isr J Med Sci 30 (8):619-22. PMID: 8045744
- ↑ Del Mar CB, Glasziou PP, Spinks AB (2006) Antibiotics for sore throat. Cochrane Database Syst Rev (4):CD000023. DOI:10.1002/14651858.CD000023.pub3 PMID: 17054126