Pharyngitis overview: Difference between revisions
No edit summary |
|||
| Line 96: | Line 96: | ||
=== Surgery === | === Surgery === | ||
=== Prevention === | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Revision as of 18:07, 29 December 2016
|
Pharyngitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pharyngitis overview On the Web |
|
American Roentgen Ray Society Images of Pharyngitis overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Overview
Pharyngitis is the inflammation of the pharynx, manifested by sore throat. It is a painful inflammation of the pharynx, and is colloquially referred to as a sore throat. [1] Pharyngitis is a common medical problem in the outpatient medical setting, resulting in more than seven million pediatric visits each year. Most types of pharyngitis are caused by infectious etiologies. The most common cause of pharyngitis is viral infection. However, some of the more serious types of pharyngitis are attributed to bacterial etiologies, such as group A-hemolytic Streptococcus pyogenes (GAS). Complications from GAS pharyngitis include rheumatic fever, deep space abscesses, and toxic shock. Although most episodes of pharyngitis are acute in nature, a small percentage becomes recurrent or chronic. With regards to chronic pharyngitis, non-infectious etiologies, such as laryngopharyngeal reflux and periodic fever, aphthous ulcers, pharyngitis, and adenitis syndrome also need to be considered. Both medical and surgical therapies are effective in managing pharyngitis. First-line medical therapy includes antibiotic therapy. For certain indications, surgical management via adenotonsillectomy is recommended. Adenotonsillectomy has been shown to be effective in reducing disease burden and improving disease-specific and global quality of life. Several techniques for adenotonsillectomy exist, including traditional and intracapsular tonsillectomies.[2]
Historical Prospective
Pathophysiology
Causes
Classification
Differential Diagnosis
Epidemiology and Demographics
Risk Factors
Natural History, Complications & Prognosis
Diagnosis
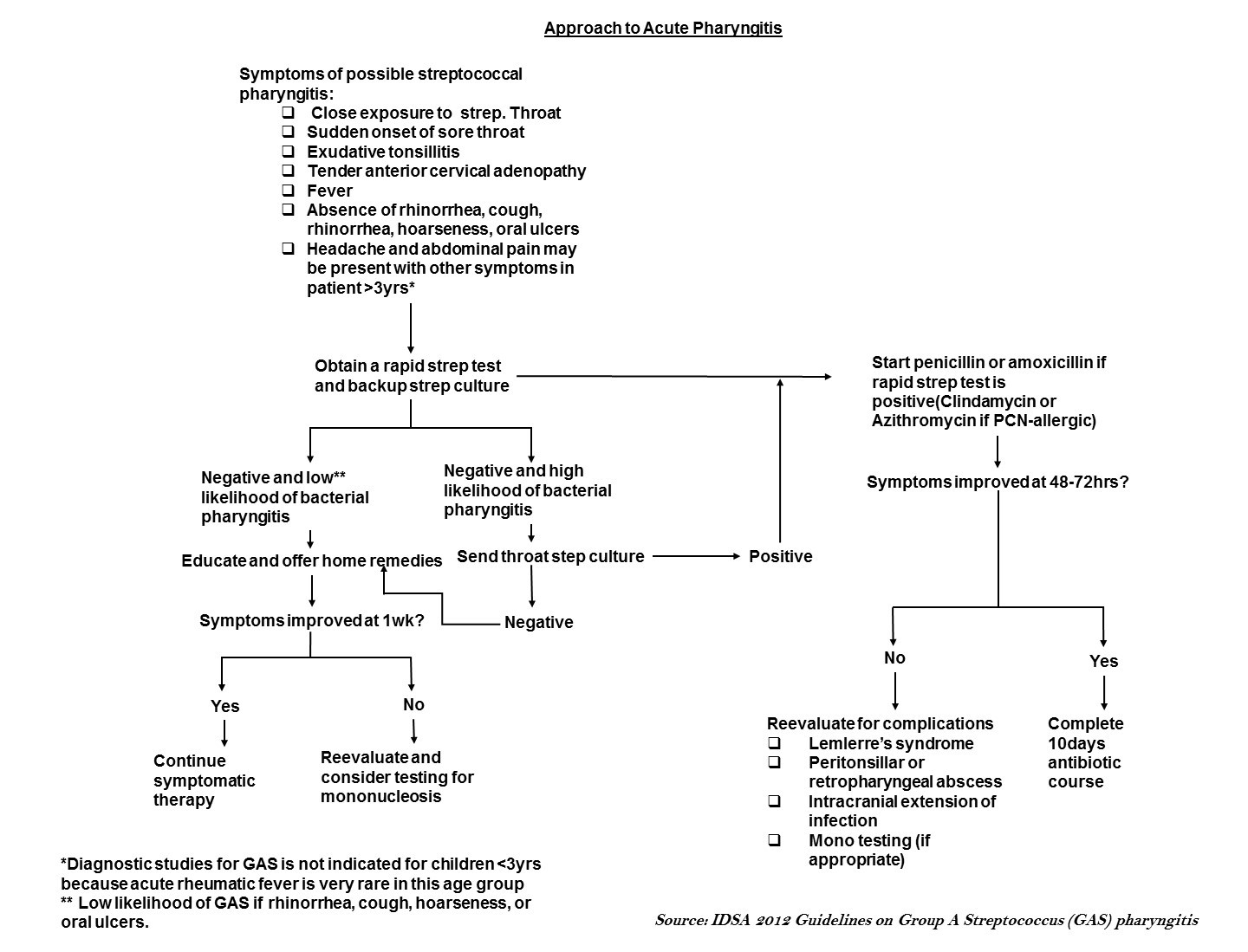
The major goal of the evaluation of patients with sore throat or acute pharyngitis is to exclude potentially dangerous causes (e.g. Group A streptococcus), to identify any treatable causes, and to improve symptoms. Identifying group A streptococcus (GAS) is important because timely treatment with antibiotics helps prevent poststreptococcal complications such as acute rheumatic fever.[3] The evaluation includes a thorough history, focused physical examination, and diagnostic testing in selected patients.
Key points in the evaluation of acute pharyngitis
- Essential to diagnosis is the identification of treatable causes (e.g. Group A streptococcus) to prevent complications.s[4]
- Signs and symptoms of GAS pharyngitis include acute onset of sore throat with tonsillar or pharyngeal exudates, tender anterior cervical lymphadenopathy, and fever.
- Signs and symptoms consistent with viral etiologies include conjunctivitis, coryza, oral ulcers, cough, and diarrhea.
- Testing for GAS pharyngitis should not be pursued in those with signs and symptoms indicative of a viral etiology.
- Rapid antigen detection tests (RADTs) alone are sufficient for the diagnosis of GAS in adults, but negative results should be backed up by throat culture in children.
- Specific techniques should be used to identify other causes where appropriate.
Centor criteria: It is important to evaluate for definitive diagnosis to exclude GAS and to avoid unnecessary lab tests and antibiotic use. Centor criteria are a widely used and accepted clinical decision tool in identifying patients for whom neither microbiologic tests nor antimicrobial therapy are necessary.The Centor score to use for children and adults with a sore throat to estimate probability of Streptococcus pyogenes infection.[5]
| Modified Centor criteria | Appropriate management according to the total score | ||||
| Criteria | Points | Total score | Chance of streptococcal infection in community
with usual levels of infection, % |
Suggested management | |
| Fever (temperature > 38°C) | +1 | 0 | 2-3 | No culture or antibiotic is required | |
| Absence of cough | +1 | 1 | 4-6 | ||
| Swollen and tender anterior cervical nodes | +1 | 2 | 10-12 | Culture all; treat only if
culture result is positive | |
| Tonsillar swelling or exudates | +1 | 3 | 27-28 | ||
| Age 3–14 yr | +1 | 4 | 38–63 | Culture all; treat with penicillin
on clinical grounds | |
| Age 15–44 yr | 0 | ||||
| Age ≥ 45 yr | -1 | ||||
Prevention
Treatment
Medical Therapy
Surgery
Prevention
References
- ↑ Acute Pharyngitis - Get Smart: Know When Antibiotics Work. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/getsmart/community/materials-references/print-materials/hcp/adult-acute-pharyngitis.html July 28, 2016
- ↑ Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G et al. (2012) Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 55 (10):1279-82. DOI:10.1093/cid/cis847 PMID: 23091044
- ↑ Del Mar CB, Glasziou PP, Spinks AB (2006) Antibiotics for sore throat. Cochrane Database Syst Rev (4):CD000023. DOI:10.1002/14651858.CD000023.pub3 PMID: 17054126
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ Anjos LM, Marcondes MB, Lima MF, Mondelli AL, Okoshi MP (2014) Streptococcal acute pharyngitis. Rev Soc Bras Med Trop 47 (4):409-13. PMID: 25229278