Necrotizing fasciitis pathophysiology: Difference between revisions
| Line 9: | Line 9: | ||
The pathophysiology of necrotizing fasciitis is common to all types of NF but the speed of development and associated clinical features differs depending on the causative organisms. | The pathophysiology of necrotizing fasciitis is common to all types of NF but the speed of development and associated clinical features differs depending on the causative organisms. | ||
*The transmission of pathogens occurs through the following routes: | *The transmission of pathogens occurs through the following routes: | ||
:*External trauma (e.g., laceration, abrasion, burn, insect bite) | :*External trauma (e.g., [[laceration]], [[abrasion]], [[burn]], insect bite) | ||
:*Direct spread from a perforated viscus (particularly colon, rectum, or anus) or another surgical procedure (e.g., vasectomy, hemorrhoidectomy) | :*Direct spread from a perforated [[viscus]] (particularly [[colon]], [[rectum]], or [[anus]]) or another surgical procedure (e.g., [[vasectomy]], [[hemorrhoidectomy]]) | ||
:*Urogenital organ | :*[[Urogenital|Urogenital organ]] | ||
:*Perirectal abscess | :*[[Abscess|Perirectal abscess]] | ||
:*Decubitus ulcer | :*[[Decubitus ulcer]] | ||
*Following transmission, the bacteria uses the entry site to invade the fascial planes which causes the wide spread necrosis of superficial fascia, deep fascia, subcutaneous fat, nerves, arteries, and veins. | *Following transmission, the bacteria uses the entry site to invade the [[Fascia|fascial planes]] which causes the wide spread necrosis of [[Fascia|superficial fascia]], [[Fascia|deep fascia]], [[Fat | ||
|subcutaneous fat]], [[nerves]], [[arteries]], and [[veins]]. | |||
*Superficial skin and deeper muscles are typically spared. | *Superficial skin and deeper muscles are typically spared. | ||
*In late stages, lesions develop liquefaction necrosis at all tissue levels. | *In late stages, lesions develop [[Necrosis|liquefaction necrosis]] at all tissue levels. | ||
'''Neonate''' | '''Neonate''' | ||
*Necrotizing fasciitis can be a serious complication of omphalitis in the neonate. | *Necrotizing fasciitis can be a serious complication of [[omphalitis]] in the [[neonate]]. | ||
*The omphalitis may progress resulting in purplish discoloration and periumbilical necrosis. | *The omphalitis may progress resulting in purplish discoloration and [[Necrosis|periumbilical necrosis]]. | ||
*The necrosis may extend to the flanks and even onto the chest wall. | *The necrosis may extend to the flanks and even onto the chest wall. | ||
| Line 28: | Line 29: | ||
'''Type 1 NF''' | '''Type 1 NF''' | ||
*The exact pathogenesis of type 1 necrotizing fasciitis is not fully understood. | *The exact pathogenesis of type 1 necrotizing fasciitis is not fully understood. | ||
*It is thought that type 1 NF is caused by polymicrobial species that work together to enhance the spread of infection (Synergistic). | *It is thought that type 1 NF is caused by polymicrobial species that work together to enhance the spread of infection ([[Synergistic]]). | ||
*Synergistic NF is comparatively slow process evolving over days. | *Synergistic NF is comparatively slow process evolving over days. | ||
*It usually develops in the area where gut flora breaches the mucosa, entering the tissue planes. | *It usually develops in the area where [[gut flora]] breaches the [[mucosa]], entering the tissue planes. | ||
'''Type 2 NF''' | '''Type 2 NF''' | ||
*[[Streptococcus|Group A streptococcus]] is the most common causative agent of type 2 NF.<ref name="pmid10925760">{{cite journal| author=Leitch HA, Palepu A, Fernandes CM| title=Necrotizing fasciitis secondary to group A streptococcus. Morbidity and mortality still high. | journal=Can Fam Physician | year= 2000 | volume= 46 | issue= | pages= 1460-6 | pmid=10925760 | doi= | pmc=2144855 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10925760 }} </ref> | *[[Streptococcus|Group A streptococcus]] is the most common causative agent of type 2 NF.<ref name="pmid10925760">{{cite journal| author=Leitch HA, Palepu A, Fernandes CM| title=Necrotizing fasciitis secondary to group A streptococcus. Morbidity and mortality still high. | journal=Can Fam Physician | year= 2000 | volume= 46 | issue= | pages= 1460-6 | pmid=10925760 | doi= | pmc=2144855 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10925760 }} </ref> | ||
*Type 2 NF is initially insidious in onset but progress more rapidly. | *Type 2 NF is initially insidious in onset but progress more rapidly. | ||
*The disease may appear spontaneously with no obvious focus. Hematogenous infection from many foci such as skin, throat, ascending vaginitis, primary peritonitis reaches the fascial layer or seeds vimentin exposed by muscle damage. | *The disease may appear spontaneously with no obvious focus. Hematogenous infection from many foci such as [[skin]], [[throat]], [[Vaginitis|ascending vaginitis]], [[Peritonitis|primary peritonitis]] reaches the fascial layer or seeds [[vimentin]] exposed by muscle damage. | ||
*Direct inoculation of GAS through wounds or associated surgery is less common. | *Direct inoculation of [[Streptococcus|GAS]] through wounds or associated surgery is less common. | ||
*The pathogenesis of type 2 NF is the result of the following process: | *The pathogenesis of type 2 NF is the result of the following process: | ||
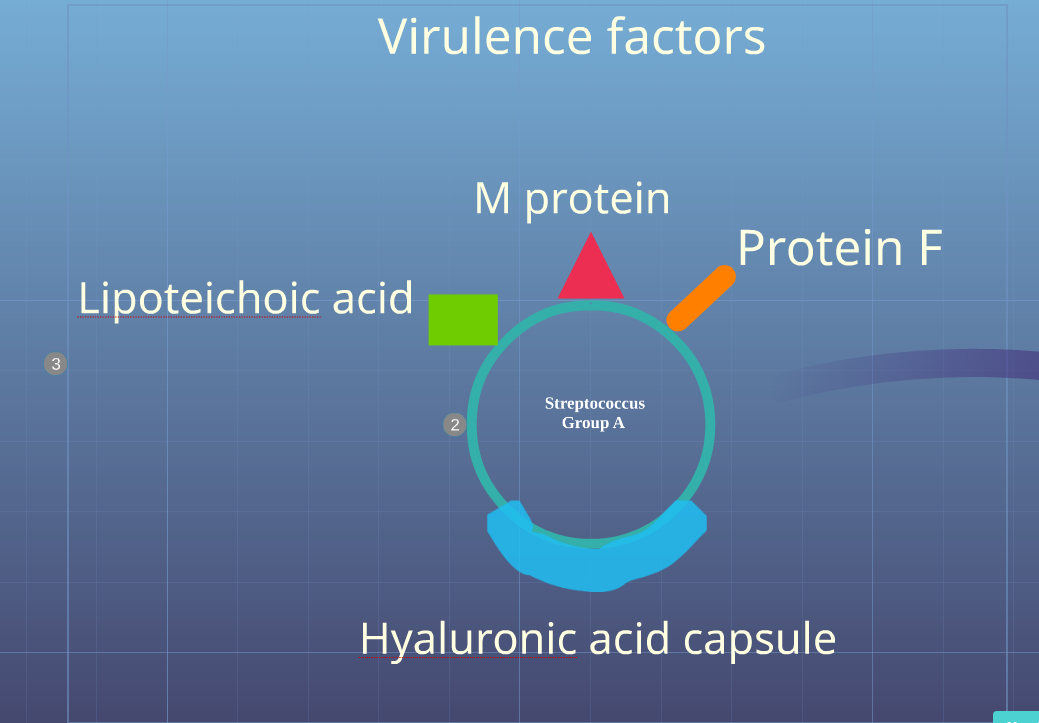
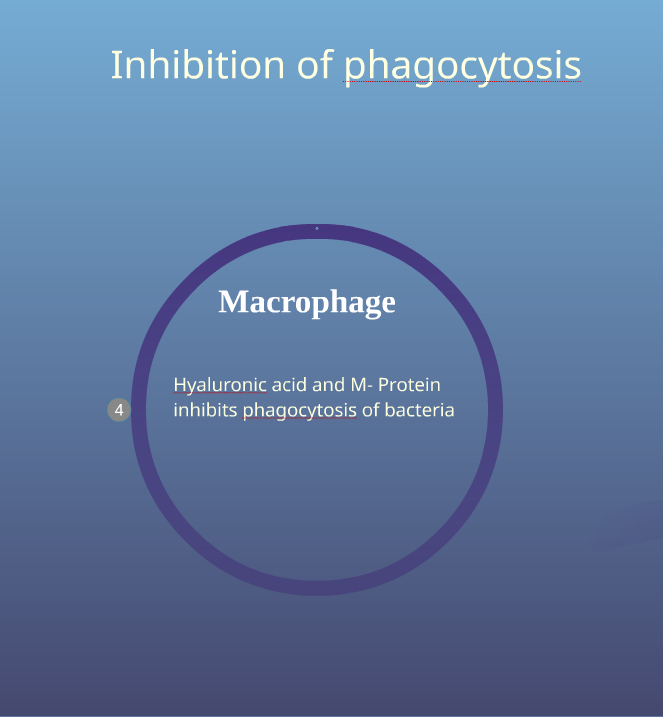
:*Inhibition of phagocytosis of bacteria by hyaluronic acid capsule and M protein | :*Inhibition of [[phagocytosis]] of bacteria by [[hyaluronic acid capsule]] and [[M protein]] | ||
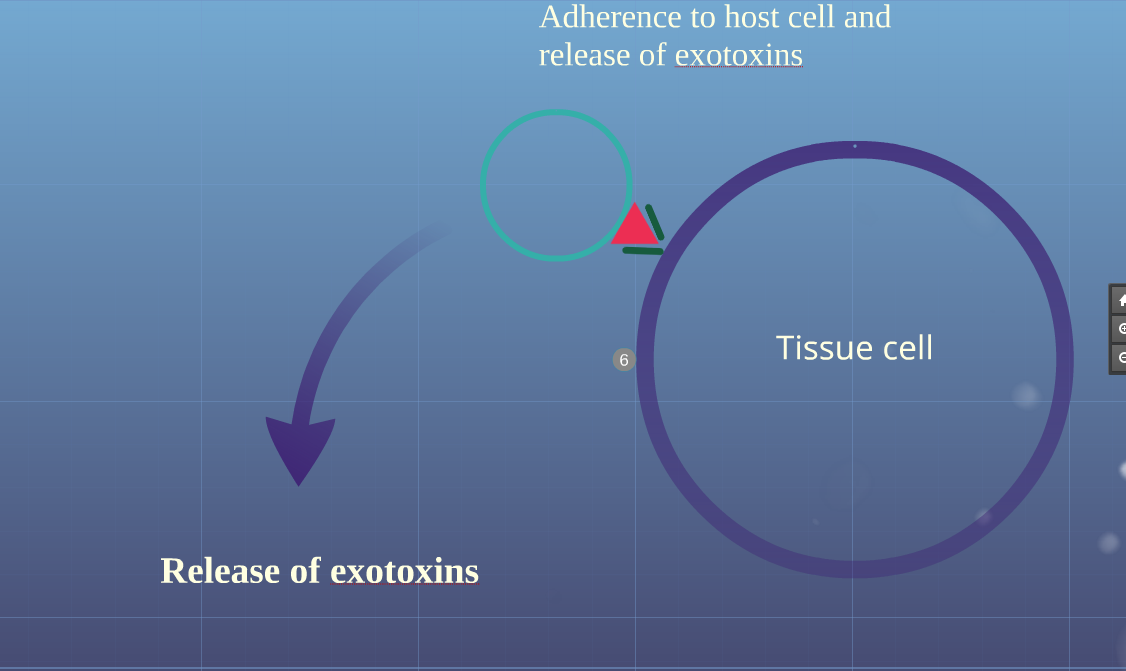
:*Adherence of bacteria to host cell through adherence factors such as M protein, protein F and lipoteichoic acid | :*Adherence of bacteria to host cell through adherence factors such as [[M protein]], [[protein F]] and [[lipoteichoic acid]] | ||
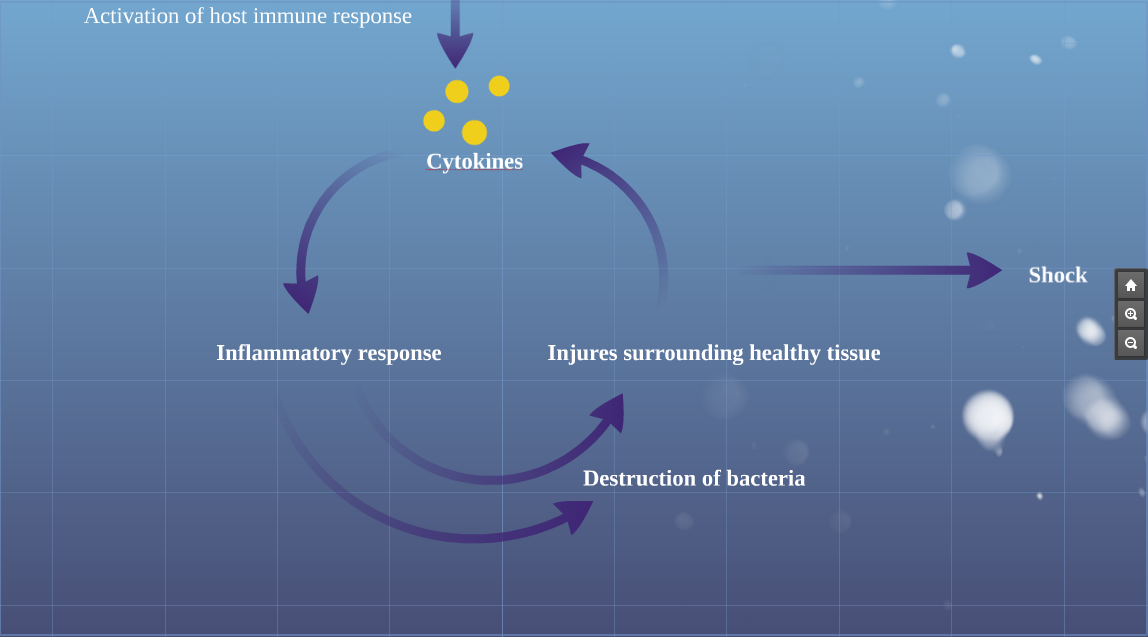
:*Release of exotoxins (streptococcal pyogenic exotoxins and superantigens) into blood produce massive proliferation of T cells and cascading release of cytokines activating inflammatory process | :*Release of [[exotoxins]] (streptococcal pyogenic exotoxins and [[superantigens]]) into blood produce massive proliferation of [[T cells]] and cascading release of [[cytokines]] activating inflammatory process | ||
:*Activation of inflammatory process which begins to kill bacteria | :*Activation of inflammatory process which begins to kill bacteria | ||
:*The streptococci release massive amounts of enzymes, hemolysins, DNAase, proteases and collagenases which destroy the normal skin and surrounding tissue with progressive coagulative necrosis | :*The streptococci release massive amounts of [[enzymes]], [[hemolysins]], [[DNAase]], [[proteases]] and [[collagenases]] which destroy the normal skin and surrounding tissue with progressive [[Necrosis|coagulative necrosis]] | ||
:*The inflamed cells release more cytokines that stimulate more inflammatory cells | :*The inflamed cells release more [[cytokines]] that stimulate more inflammatory cells | ||
:*The massive release of cytokines result in systemic inflammatory response syndrome resulting in shock, organ failure, depression of myocardial function and immune suppression | :*The massive release of cytokines result in [[systemic inflammatory response syndrome]] resulting in [[shock]], organ failure, depression of myocardial function and immune suppression | ||
:*Stimulation of T-cells by superantigens causes activation of complement pathway, the bradykinin-kallikrein system, and the coagulation cascade, worsening small vessel thrombosis and tissue ischemia. Tissue ischemia impedes oxidative destruction of bacteria by polymorphonuclear cells and prevents adequate delivery of antibiotics. | :*Stimulation of [[T-cells]] by [[superantigens]] causes activation of [[complement pathway]], the [[bradykinin-kallikrein system]], and the [[coagulation cascade]], worsening small vessel [[thrombosis]] and tissue ischemia. [[Ischemia|Tissue ischemia]] impedes oxidative destruction of [[bacteria]] by [[polymorphonuclear cells]] and prevents adequate delivery of antibiotics. | ||
:*The blood flow to local tissue is compromised due to thrombosis of large number of dermal capillaries by the local hypercoaguable state, platelet-neutrophil plugging of vessels and increased interstitial pressure. | :*The blood flow to local tissue is compromised due to thrombosis of large number of dermal capillaries by the local [[Coagulation|hypercoaguable state]], [[platelet]]-[[neutrophil]] plugging of vessels and increased [[interstitial pressure]]. | ||
*Nerves supplying the necrotizing areas of skin die, the central areas become anaesthetic and peripheral areas remain tender. | *Nerves supplying the necrotizing areas of skin die, the central areas become [[anaesthetic]] and peripheral areas remain tender. | ||
*In later stages, infection from deeper layers ascends, producing | *In later stages, infection from deeper layers ascends, producing [[edema]] of epidermal and dermal layers ([[peau d'orange]]) and a woody firmness of the tissues | ||
*The fascial and nerve destruction results in sensory and motor deficits, which causes progression of hemorrhagic bullae to cutaneous gangrene. | *The fascial and nerve destruction results in [[sensory]] and [[motor|motor deficits]], which causes progression of hemorrhagic bullae to cutaneous gangrene. | ||
<gallery> | <gallery> | ||
Image:Virulence_factors.PNG|Virulence Factors of Group A Streptococcus | Image:Virulence_factors.PNG|Virulence Factors of Group A Streptococcus | ||
Image:Inhibition_of_Phagocytosis.PNG|Inhibition of phagocytosis | Image:Inhibition_of_Phagocytosis.PNG|Inhibition of [[phagocytosis]] | ||
Image:Adherence.PNG|Adherance to host cell and release of exotoxins | Image:Adherence.PNG|Adherance to host cell and release of [[exotoxins]] | ||
Image:Host_immune_response.PNG|Activation of host immune response | Image:Host_immune_response.PNG|Activation of host immune response | ||
| Line 64: | Line 65: | ||
Recurrent NF is seen in following conditions: | Recurrent NF is seen in following conditions: | ||
*Methicillin resistant staphylococcus aureus [[MRSA]] | *Methicillin resistant staphylococcus aureus [[MRSA]] | ||
*Complement C4 deficiency | *[[Complement|Complement C4 deficiency]] | ||
===Gross pathology=== | ===Gross pathology=== | ||
On gross pathology the characteristic findings of necrotizing fasciitis include:<ref name=NF>Librae pathology(2015) https://librepathology.org/wiki/Necrotizing_fasciitis Accessed on September 2,2016 </ref> | On gross pathology the characteristic findings of necrotizing fasciitis include:<ref name=NF>Librae pathology(2015) https://librepathology.org/wiki/Necrotizing_fasciitis Accessed on September 2,2016 </ref> | ||
*Subcutaneous emphysema | *[[Emphysema|Subcutaneous emphysema]] | ||
*Edema | *[[Edema]] | ||
*Erythema | *[[Erythema]] | ||
*Bulae | *[[Bulae]] | ||
*Skin sloughing | *Skin sloughing | ||
*Dull grey discoloration | *Dull grey discoloration | ||
| Line 85: | Line 86: | ||
On microscopic histopathological analysis, the characteristic findings of necrotizing fasciitis are<ref name=NF>Librae pathology(2015) https://librepathology.org/wiki/Necrotizing_fasciitis Accessed on September 2,2016 </ref> | On microscopic histopathological analysis, the characteristic findings of necrotizing fasciitis are<ref name=NF>Librae pathology(2015) https://librepathology.org/wiki/Necrotizing_fasciitis Accessed on September 2,2016 </ref> | ||
*Early stages | *Early stages | ||
:*Obliterative vasculitis with microangiopathic thrombosis | :*[[Vasculitis|Obliterative vasculitis]] with microangiopathic thrombosis | ||
:*Acute inflammation of subcutaneous tissue | :*Acute inflammation of subcutaneous tissue | ||
:*Superficial hyaline necrosis along with edema and inflammation of the dermis and subcutaneous fat | :*Superficial hyaline necrosis along with [[edema]] and [[inflammation]] of the dermis and subcutaneous fat | ||
:*Dense neutrophil-predominant inflammatory infiltrate | :*Dense [[neutrophil]]-predominant inflammatory infiltrate | ||
*Late stages | *Late stages | ||
:*Noninflammatory intravascular coagulation and hemorrhage | :*Noninflammatory [[Coagulation|intravascular coagulation]] and [[hemorrhage]] | ||
:*Myonecrosis | :*[[Myonecrosis]] | ||
<gallery> | <gallery> | ||
Revision as of 19:08, 12 September 2016
|
Necrotizing fasciitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Necrotizing fasciitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Necrotizing fasciitis pathophysiology |
|
Risk calculators and risk factors for Necrotizing fasciitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yamuna Kondapally, M.B.B.S[2]
Overview
The pathophysiology of necrotizing fasciitis is common to all types but the speed of development and associated clinical features differs depending on the causative organisms. Following transmission, the bacteria uses the entry site to invade the fascial planes which causes the wide spread necrosis of superficial fascia, deep fascia, subcutaneous fat, nerves, arteries, and veins. Necrotizing fasciitis can be a serious complication of omphalitis in the neonate.The pathogenesis of necrotizing fasciitis is the result of bacterial and host factors. The exact pathogenesis of type 1 necrotizing fasciitis is not fully understood but polymicrobial species work together to enhance the spread of infection (Synergistic). Group A streptococcus is the most common causative agent of type 2 NF. Bacterial virulence factors, exotoxins, superantigens and host immune system plays a major role in the pathogenesis of type II NF. Recurrent NF is caused by MRSA. On gross pathology, the characteristic findings of NF include subcutaneous emphysema, skin sloughing, bulae and necrosis. Inflammatory changes are seen on microscopic histopathology.
Pathophysiology
The pathophysiology of necrotizing fasciitis is common to all types of NF but the speed of development and associated clinical features differs depending on the causative organisms.
- The transmission of pathogens occurs through the following routes:
- External trauma (e.g., laceration, abrasion, burn, insect bite)
- Direct spread from a perforated viscus (particularly colon, rectum, or anus) or another surgical procedure (e.g., vasectomy, hemorrhoidectomy)
- Urogenital organ
- Perirectal abscess
- Decubitus ulcer
- Following transmission, the bacteria uses the entry site to invade the fascial planes which causes the wide spread necrosis of superficial fascia, deep fascia, [[Fat
|subcutaneous fat]], nerves, arteries, and veins.
- Superficial skin and deeper muscles are typically spared.
- In late stages, lesions develop liquefaction necrosis at all tissue levels.
Neonate
- Necrotizing fasciitis can be a serious complication of omphalitis in the neonate.
- The omphalitis may progress resulting in purplish discoloration and periumbilical necrosis.
- The necrosis may extend to the flanks and even onto the chest wall.
Pathogenesis
The pathogenesis of necrotizing fasciitis is the result of bacterial and host factors.
Type 1 NF
- The exact pathogenesis of type 1 necrotizing fasciitis is not fully understood.
- It is thought that type 1 NF is caused by polymicrobial species that work together to enhance the spread of infection (Synergistic).
- Synergistic NF is comparatively slow process evolving over days.
- It usually develops in the area where gut flora breaches the mucosa, entering the tissue planes.
Type 2 NF
- Group A streptococcus is the most common causative agent of type 2 NF.[1]
- Type 2 NF is initially insidious in onset but progress more rapidly.
- The disease may appear spontaneously with no obvious focus. Hematogenous infection from many foci such as skin, throat, ascending vaginitis, primary peritonitis reaches the fascial layer or seeds vimentin exposed by muscle damage.
- Direct inoculation of GAS through wounds or associated surgery is less common.
- The pathogenesis of type 2 NF is the result of the following process:
- Inhibition of phagocytosis of bacteria by hyaluronic acid capsule and M protein
- Adherence of bacteria to host cell through adherence factors such as M protein, protein F and lipoteichoic acid
- Release of exotoxins (streptococcal pyogenic exotoxins and superantigens) into blood produce massive proliferation of T cells and cascading release of cytokines activating inflammatory process
- Activation of inflammatory process which begins to kill bacteria
- The streptococci release massive amounts of enzymes, hemolysins, DNAase, proteases and collagenases which destroy the normal skin and surrounding tissue with progressive coagulative necrosis
- The inflamed cells release more cytokines that stimulate more inflammatory cells
- The massive release of cytokines result in systemic inflammatory response syndrome resulting in shock, organ failure, depression of myocardial function and immune suppression
- Stimulation of T-cells by superantigens causes activation of complement pathway, the bradykinin-kallikrein system, and the coagulation cascade, worsening small vessel thrombosis and tissue ischemia. Tissue ischemia impedes oxidative destruction of bacteria by polymorphonuclear cells and prevents adequate delivery of antibiotics.
- The blood flow to local tissue is compromised due to thrombosis of large number of dermal capillaries by the local hypercoaguable state, platelet-neutrophil plugging of vessels and increased interstitial pressure.
- Nerves supplying the necrotizing areas of skin die, the central areas become anaesthetic and peripheral areas remain tender.
- In later stages, infection from deeper layers ascends, producing edema of epidermal and dermal layers (peau d'orange) and a woody firmness of the tissues
- The fascial and nerve destruction results in sensory and motor deficits, which causes progression of hemorrhagic bullae to cutaneous gangrene.
-
Virulence Factors of Group A Streptococcus
-
Inhibition of phagocytosis
-
Adherance to host cell and release of exotoxins
-
Activation of host immune response
Recurrent necrotizing fasciitis
Recurrent NF is seen in following conditions:
- Methicillin resistant staphylococcus aureus MRSA
- Complement C4 deficiency
Gross pathology
On gross pathology the characteristic findings of necrotizing fasciitis include:[2]
- Subcutaneous emphysema
- Edema
- Erythema
- Bulae
- Skin sloughing
- Dull grey discoloration
Microscopic histopathological analysis
On microscopic histopathological analysis, the characteristic findings of necrotizing fasciitis are[2]
- Early stages
- Obliterative vasculitis with microangiopathic thrombosis
- Acute inflammation of subcutaneous tissue
- Superficial hyaline necrosis along with edema and inflammation of the dermis and subcutaneous fat
- Dense neutrophil-predominant inflammatory infiltrate
- Late stages
- Noninflammatory intravascular coagulation and hemorrhage
- Myonecrosis
References
- ↑ Leitch HA, Palepu A, Fernandes CM (2000). "Necrotizing fasciitis secondary to group A streptococcus. Morbidity and mortality still high". Can Fam Physician. 46: 1460–6. PMC 2144855. PMID 10925760.
- ↑ 2.0 2.1 2.2 2.3 Librae pathology(2015) https://librepathology.org/wiki/Necrotizing_fasciitis Accessed on September 2,2016
![Beginning of necrotizing fasciitis[2]](/images/a/a5/Beginning_of_Necrotizing_Fasciitis_01.jpg)
![Necrotizing fasciitis of left leg[2]](/images/0/0a/800px-Necrotizing_fasciitis_left_leg.JPEG)