Bronchiectasis pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 28: | Line 28: | ||
===Immune Response=== | ===Immune Response=== | ||
*Bronchiectasis may involve several processes | *Bronchiectasis may involve several processes | ||
*If there is inflammation, bronchiectasis can result from inflammation via increased levels of: | *If there is [[inflammation]], bronchiectasis can result from [[inflammation]] via increased levels of: | ||
:*Reactive oxygen species (ROS) | :*[[Reactive oxygen species]] (ROS) | ||
::*A by product for the metabolism of oxygen | ::*A by product for the metabolism of [[oxygen]] | ||
::*Increased levels can cause damage to cell structures | ::*Increased levels can cause damage to cell structures | ||
:*Elastase | :*[[Elastase]] | ||
::*Enzyme of a class of proteases that break down elastin | ::*[[Enzyme]] of a class of [[proteases]] that break down [[elastin]] | ||
::*Elastin plus collagen determines the mechanical properties of connective tissue | ::*[[Elastin]] plus [[collagen]] determines the mechanical properties of [[connective tissue]] | ||
:*Matrix metalloproteinases (MMPs) | :*[[Matrix metalloproteinases]] (MMPs) | ||
::*Responsible for the degradation of most of the extracellular proteins during normal tissue turnover | ::*Responsible for the degradation of most of the extracellular proteins during normal tissue turnover | ||
*Inflammation can also lead to epithelial injury and mucus secretion via increased levels of ROS, elastase | *[[Inflammation]] can also lead to epithelial injury and [[mucus]] secretion via increased levels of ROS, [[elastase]] ciliotoxin and [[mucus]] secretogogues | ||
*Epithelial injury and mucus hypersecretion lead to chronic bronchial infection, reduced mucociliary clearance, and plugging of the airway - which all eventually leads to airway damage and bronchiectasis | *[[Epithelial]] injury and [[mucus]] hypersecretion lead to chronic [[bronchial]] infection, reduced mucociliary clearance, and plugging of the airway - which all eventually leads to airway damage and bronchiectasis | ||
Revision as of 19:28, 29 June 2015
|
Bronchiectasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Bronchiectasis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Bronchiectasis pathophysiology |
|
Risk calculators and risk factors for Bronchiectasis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Saarah T. Alkhairy, M.D.
Overview
Bronchiectasis involves bronchi that are permanently dilated inflamed, and easily collapsible. This results in airflow obstruction and impaired clearance of secretions Cole's Cycle describes how infections and a defect in the host defense are factors for this disease. An immune response also plays a role in the pathogenesis.
Pathophysiology[1]
- Dilation of the bronchial walls results in airflow obstruction and impaired clearance of secretions
- The dilated areas interrupt normal air pressure of the bronchial tubes, causing sputum to pool inside the dilated areas instead of being pushed upward
- The pooled sputum provides an environment favorable to the growth of infectious pathogens
- The more infections that the lungs experience, the more damaged the alveoli in the lung become
- With more damage to the lung tissue, the bronchial tubes become more inelastic and dilated
- This creates a perpetual, destructive cycle
- The biopsies indicate that the infiltrate contains neutrophils, T lymphocytes and macrophages
- The sputum contains elastase, interleukin-8, tumor necrosis factor a (TNF-a), and prostanoids
Cole's Cycle[2]
- Also known as Cole's "vicious cycle hypothesis"
- The most widely known model of the development of bronchiectasis
- Impaired muco-ciliary clearance due to genetic susceptibility causes environmental insult
- Results in persistence of microbes in the sinobronchial tree
- The microbial infection causes chronic inflammation
- This results in tissue damage and impaired mucociliary motility
- This leads to more infection with a cycle of inflammation causing lung damage
- Two factors required for the development of this condition are persistent infection and a defect in host defense
Immune Response
- Bronchiectasis may involve several processes
- If there is inflammation, bronchiectasis can result from inflammation via increased levels of:
- Reactive oxygen species (ROS)
- A by product for the metabolism of oxygen
- Increased levels can cause damage to cell structures
- Matrix metalloproteinases (MMPs)
- Responsible for the degradation of most of the extracellular proteins during normal tissue turnover
- Inflammation can also lead to epithelial injury and mucus secretion via increased levels of ROS, elastase ciliotoxin and mucus secretogogues
- Epithelial injury and mucus hypersecretion lead to chronic bronchial infection, reduced mucociliary clearance, and plugging of the airway - which all eventually leads to airway damage and bronchiectasis
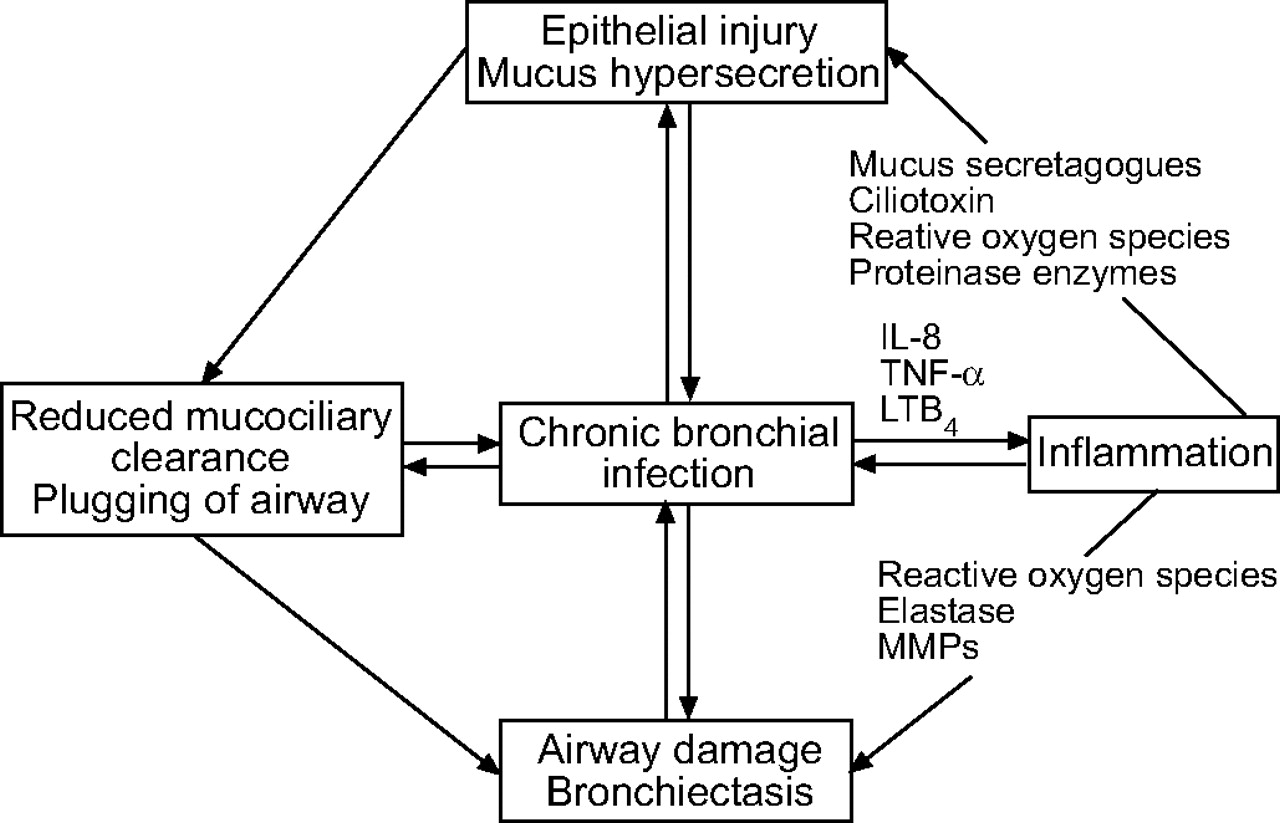
The diagram below depicts the immune response for bronchiectasis
-
Schematic representation of a vicious circle of events which occurs during chronic bronchial infection. IL: interleukin; TNF: tumour necrosis factor; LT: leukotriene; MMP: matrix metalloproteinase
European Respiratory Journal