Follicular thyroid cancer diagnostic study of choice: Difference between revisions
No edit summary |
Farima Kahe (talk | contribs) No edit summary |
||
| (6 intermediate revisions by 3 users not shown) | |||
| Line 10: | Line 10: | ||
*[[Biopsy]] is the [[Gold standard (test)|gold standard]] for [[Diagnosis|diagnosing]] thyroid cancer.<ref>{{Cite web|url=https://www.cancer.org/cancer/thyroid-cancer/detection-diagnosis-staging/how-diagnosed.html|title=|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref> | *[[Biopsy]] is the [[Gold standard (test)|gold standard]] for [[Diagnosis|diagnosing]] thyroid cancer.<ref>{{Cite web|url=https://www.cancer.org/cancer/thyroid-cancer/detection-diagnosis-staging/how-diagnosed.html|title=|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref> | ||
*[[Biopsy]] can be taken by the following methods: | *[[Biopsy]] can be taken by the following methods: | ||
**'''Fine Needle Aspiration Biopsy (FNAC)''' | |||
* It involves [[extraction]] of [[thyroid]] [[Tissue (biology)|tissue]] using a thin needle. | *** It involves [[extraction]] of [[thyroid]] [[Tissue (biology)|tissue]] using a thin needle. | ||
*The needle is inserted through the [[skin]] into the [[thyroid]]. Several [[Tissue (biology)|tissue]] samples are taken from different parts of the [[thyroid]]. | ***The needle is inserted through the [[skin]] into the [[thyroid]]. Several [[Tissue (biology)|tissue]] samples are taken from different parts of the [[thyroid]]. | ||
**'''Surgical Biopsy''' | |||
***Surgical [[biopsy]] is the removal of the [[thyroid]] nodule or one [[lobe]] of the [[thyroid]] during [[surgery]]. | |||
* Surgical biopsy is the removal of the thyroid nodule or one lobe of the thyroid during surgery. | *** On microscopic examination, trabecular follicular tumor cells that invade [[tumor]] capsule or surrounding vascular structures, are found. | ||
* On microscopic examination, trabecular follicular tumor cells that invade tumor capsule or surrounding vascular structures are found. | |||
====Images of Biopsy Specimen==== | ====Images of Biopsy Specimen==== | ||
| Line 24: | Line 23: | ||
</gallery> | </gallery> | ||
===Staging<ref | ===Staging<ref name="urlThyroid Cancer Treatment (Adult) (PDQ®)–Health Professional Version - National Cancer Institute">{{cite web |url=https://www.cancer.gov/types/thyroid/hp/thyroid-treatment-pdq#_441_toc |title=Thyroid Cancer Treatment (Adult) (PDQ®)–Health Professional Version - National Cancer Institute |format= |work= |accessdate=}}</ref>=== | ||
( | |||
<br> | <br> | ||
{| | {| class="wikitable" | ||
|+ | |+ | ||
! style="background: #4479BA; | |||
! colspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" + |Primary tumor | |||
|- | |- | ||
| align="center" style="background:#f0f0f0;" |'''Tumor size''' | |||
| style="background: # | | align="center" style="background:#f0f0f0;" |'''Sub-stage''' | ||
| align="center" style="background:#f0f0f0;" |'''Finding''' | |||
|'''Image''' | |||
|- | |- | ||
| T0 | |||
| | | || | ||
* No evidence of primary [[tumor]] | * No evidence of primary [[tumor]] | ||
| | |||
|- | |||
| T1 | |||
| || | |||
* [[Tumor]] ≤2 cm in greatest dimension limited to the [[thyroid]] | |||
| | |||
|- | |||
| T1 | |||
| a|| | |||
* [[Tumor]] ≤1 cm, limited to the [[thyroid]] | |||
| [[Image:Diagram showing stage T1a thyroid cancer CRUK 250.png|200px|thumb|none]] | |||
|- | |||
| T1 | |||
| b|| | |||
* [[Tumor]] >1 cm but ≤2 cm in greatest dimension, limited to the [[thyroid]] | |||
| [[Image:Diagram showing stage T1b thyroid cancer CRUK 251.svg.png|200px|thumb|none]] | |||
|- | |- | ||
| T2 | |||
| | | || | ||
* [[Tumor]] | * [[Tumor]] >2 cm but ≤4 cm in greatest dimension, limited to the [[thyroid]] | ||
| | |||
|- | |- | ||
| T3 | |||
| | | || | ||
* [[Tumor]] | * [[Tumor]] >4 cm limited to the [[thyroid]], or gross extrathyroidal extension invading only strap [[muscles]] | ||
| [[Image:Diagram showing stage T3 thyroid cancer CRUK 265.png|200px|thumb|none]] | |||
|- | |- | ||
|T3 | |||
| | |a | ||
* [[Tumor]] > | | | ||
* [[Tumor]] >4 cm limited to the [[thyroid]] | |||
| | |||
|- | |- | ||
|T3 | |||
| | |b | ||
* [[ | | | ||
* Gross extrathyroidal extension invading only strap [[muscles]] ([[sternohyoid]], [[sternothyroid]], [[thyrohyoid]], or [[Omohyoid muscle|omohyoid muscles]]) from a [[tumor]] of any size | |||
| | |||
|- | |- | ||
| T4 | |||
| | | || | ||
* [[Tumor]] | * [[Tumor]] includes gross extrathyroidal extension beyond the strap [[muscles]] | ||
| | |||
|- | |- | ||
| T4 | |||
| | | a|| | ||
* | * [[Tumor]] with gross extrathyroidal extension invading subcutaneous [[Soft tissue|soft tissues]], [[larynx]], [[trachea]], [[esophagus]], or [[recurrent laryngeal nerve]] from a [[tumor]] of any size | ||
|[[Image:Diagram showing stage T4a thyroid cancer CRUK 272.png|200px|thumb|none]] | |||
|- | |- | ||
| | | T4 | ||
* [[Tumor]] | | b|| | ||
* [[Tumor]] with gross extrathyroidal extension invading [[prevertebral fascia]] or encasing the [[carotid artery]] or [[mediastinal]] vessels from a [[tumor]] of any size. | |||
|[[Image:Diagram showing stage T4b thyroid cancer CRUK 273.png|200px|thumb|none]] | |||
|- | |- | ||
| TX | |||
| | | || | ||
* | * Primary [[tumor]] cannot be assessed | ||
| | |||
|- | |- | ||
| style="background: # | |+ | ||
* [[ | |||
| | ! colspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" + |Regional lymph node involvement | ||
|- | |||
| align="center" style="background:#f0f0f0;" |'''Node involvement''' | |||
| | | align="center" style="background:#f0f0f0;" |'''Sub-stage''' | ||
| align="center" style="background:#f0f0f0;" |'''Finding''' | |||
|'''Image''' | |||
|- | |||
| N0 | |||
| || | |||
* No [[lymph node]] involvement | |||
| | |||
|- | |||
|N0 | |||
|a | |||
| | |||
* One or more cytologically or [[histologically]] confirmed benign [[lymph nodes]] | |||
| | |||
|- | |||
|N0 | |||
|b | |||
| | |||
* No [[Radiological|radiologic]] or clinical evidence of locoregional [[lymph node]] [[metastasis]] | |||
| | |||
|- | |||
| N1 | |||
| || | |||
* [[Metastasis]] to regional nodes | |||
| | |||
|- | |||
| N1 | |||
| a|| | |||
* [[Metastasis]] to level VI or VII ([[Pretracheal lymph nodes|pretracheal]], [[Paratracheal lymph nodes|paratracheal]], or [[Prelaryngeal lymph nodes|prelaryngeal]]/Delphian, or upper mediastinal) [[lymph nodes]]. This can be unilateral or bilateral [[disease]] | |||
|[[Image:Diagram showing stage N1a thyroid cancer CRUK 242.png|200px|thumb|none]] | |||
|- | |||
| N1 | |||
| b|| | |||
* [[Metastasis]] to unilateral, bilateral, or contralateral [[Cervical lymph nodes|cervical]] neck [[lymph nodes]] (levels I, II, III, IV, or V) or [[retropharyngeal lymph nodes]] | |||
|[[Image:Diagram showing stage N1b thyroid cancer CRUK 243.png|200px|thumb|none]] | |||
|- | |- | ||
| NX | |||
| | | || | ||
* Regional [[lymph node]] cannot be assessed | * Regional [[lymph node]] cannot be assessed | ||
| | |||
|- | |- | ||
! style="background: # | |+ | ||
! colspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" + |Distant metastasis | |||
|- | |- | ||
| align="center" style="background:#f0f0f0;" |'''Presence of metastasis''' | |||
| style="background: # | | align="center" style="background:#f0f0f0;" |'''Sub-stage''' | ||
* | | align="center" style="background:#f0f0f0;" |'''Finding''' | ||
|'''Image''' | |||
|- | |||
| M0 | |||
| || | |||
* No distant [[metastasis]] | |||
| | |||
|- | |- | ||
| M1 | |||
| | | IV|| | ||
* [[ | * Distant [[metastasis]] | ||
|[[Image:Stage M1 Thyroid cancer.png|200px|thumb|none]] | |||
|- | |- | ||
|} | |} | ||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px;" align=center | ||
|+ | |+ | ||
|- | |||
|- | |- | ||
| | |- | ||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |- | ||
|- | |||
|} | |||
<br /> | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px;" align=center | ||
|+'''''Anatomic Stage/Prognostic Groups''''' | |+'''''Anatomic Stage/Prognostic Groups''''' | ||
! style="background: #4479BA; width: | ! style="background: #4479BA; width: 120px;" | {{fontcolor|#FFF|Stage}} | ||
! style="background: #4479BA; width: | ! style="background: #4479BA; width: 550px;" | {{fontcolor|#FFF|T}} | ||
! style="background: #4479BA; width: | ! style="background: #4479BA; width: 550px;" | {{fontcolor|#FFF|N}} | ||
! style="background: #4479BA; width: | ! style="background: #4479BA; width: 550px;" | {{fontcolor|#FFF|M}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" colspan=4 align=center| '''Follicular thyroid carcinoma''' | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" colspan=4 align=center| '''Follicular thyroid carcinoma''' | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" colspan=4 | '''YOUNGER THAN | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" colspan=4 | '''YOUNGER THAN 55 YEARS''' | ||
|- | |- | ||
! style="background: #DCDCDC;" |I | ! style="background: #DCDCDC;" |I | ||
! style="background: #F5F5F5;" |Any T | |||
! style="background: #F5F5F5;" |Any N | |||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #DCDCDC;" |II | ! style="background: #DCDCDC;" |II | ||
! style="background: #F5F5F5;" |Any T | |||
! style="background: #F5F5F5;" |Any N | |||
! style="background: #F5F5F5;" |M1 | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" colspan=4 | ''' | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" colspan=4 | '''55 YEARS AND OLDER''' | ||
|- | |- | ||
! style="background: #DCDCDC;" |I | ! style="background: #DCDCDC;" |I | ||
! style="background: #F5F5F5;" |T1 | |||
! style="background: #F5F5F5;" |Any N | |||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #DCDCDC;" |II | ! rowspan="4" style="background: #DCDCDC;" |II | ||
! style="background: #F5F5F5;" |T1 | |||
! style="background: #F5F5F5;" |N1 | |||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #F5F5F5;" |T2 | |||
! | ! style="background: #F5F5F5;" |N1 | ||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #F5F5F5;" |T3a | |||
! | ! style="background: #F5F5F5;" |Any N | ||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #F5F5F5;" |T3b | |||
! | ! style="background: #F5F5F5;" |Any N | ||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #DCDCDC;" | | ! style="background: #DCDCDC;" |III | ||
! style="background: #F5F5F5;" |T4a | |||
! style="background: #F5F5F5;" |Any N | |||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #DCDCDC;" |IVA | ! style="background: #DCDCDC;" |IVA | ||
! style="background: #F5F5F5;" |T4b | |||
! style="background: #F5F5F5;" |Any N | |||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #DCDCDC;" | | ! rowspan="6" style="background: #DCDCDC;" |IVB | ||
! style="background: #F5F5F5;" |Any T | |||
! style="background: #F5F5F5;" |Any N | |||
! style="background: #F5F5F5;" |M1 | |||
|- | |- | ||
! style="background: #F5F5F5;" |T1 | |||
! | ! style="background: #F5F5F5;" |N1 | ||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #F5F5F5;" |T2 | |||
! | ! style="background: #F5F5F5;" |N1 | ||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #F5F5F5;" |T3a | |||
! | ! style="background: #F5F5F5;" |N1 | ||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #F5F5F5;" |T3b | |||
! | ! style="background: #F5F5F5;" |Any N | ||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #F5F5F5;" |T4 | |||
! | ! style="background: #F5F5F5;" |Any N | ||
! style="background: #F5F5F5;" |M0 | |||
|- | |- | ||
! style="background: #DCDCDC;" | | ! style="background: #DCDCDC;" |IVC | ||
! style="background: #F5F5F5;" |Any T | |||
! style="background: #F5F5F5;" |Any N | |||
! style="background: #F5F5F5;" |M1 | |||
|} | |} | ||
Latest revision as of 15:42, 29 October 2019
|
Follicular thyroid cancer Microchapters |
|
Differentiating Follicular thyroid cancer from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Follicular thyroid cancer diagnostic study of choice On the Web |
|
American Roentgen Ray Society Images of Follicular thyroid cancer diagnostic study of choice |
|
Follicular thyroid cancer diagnostic study of choice in the news |
|
Blogs on Follicular thyroid cancer diagnostic study of choice |
|
Risk calculators and risk factors for Follicular thyroid cancer diagnostic study of choice |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Overview
Biopsy is the gold standard for diagnosing thyroid cancer. According to the American Joint Committee on Cancer (AJCC), there are 4 stages of follicular thyroid cancer based on the clinical features and findings on imaging. Each stage is assigned a letter and a number that designate the tumor size, number of lymph node regions involved, and metastasis.
Diagnostic Study of Choice
Study of Choice
- Biopsy is the gold standard for diagnosing thyroid cancer.[1]
- Biopsy can be taken by the following methods:
- Fine Needle Aspiration Biopsy (FNAC)
- Surgical Biopsy
Images of Biopsy Specimen
Staging[4]
| Primary tumor | |||
|---|---|---|---|
| Tumor size | Sub-stage | Finding | Image |
| T0 |
|
||
| T1 | |||
| T1 | a | 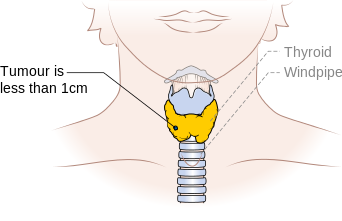 | |
| T1 | b | 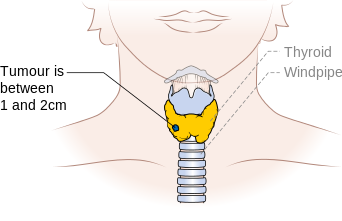 | |
| T2 | |||
| T3 | 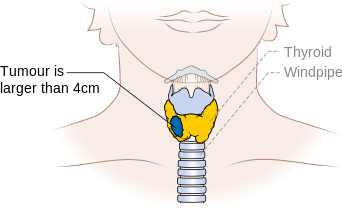 | ||
| T3 | a | ||
| T3 | b |
|
|
| T4 | |||
| T4 | a |
|
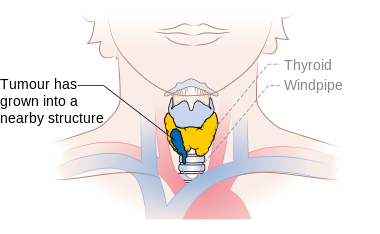 |
| T4 | b |
|
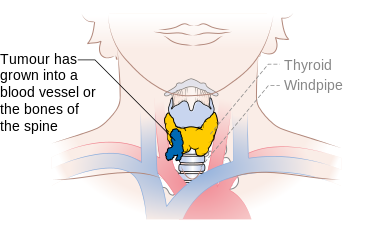 |
| TX |
|
||
| Regional lymph node involvement | |||
| Node involvement | Sub-stage | Finding | Image |
| N0 |
|
||
| N0 | a |
|
|
| N0 | b |
|
|
| N1 |
|
||
| N1 | a |
|
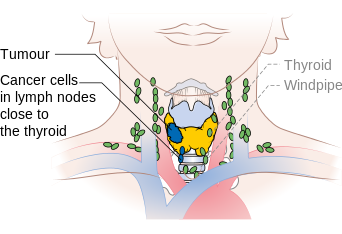 |
| N1 | b |
|
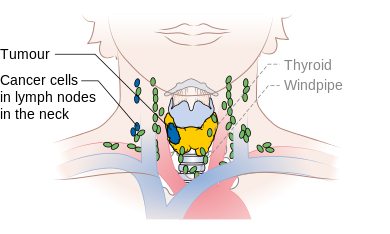 |
| NX |
|
||
| Distant metastasis | |||
| Presence of metastasis | Sub-stage | Finding | Image |
| M0 |
|
||
| M1 | IV |
|
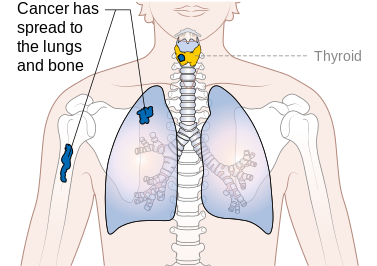 |
| Stage | T | N | M |
|---|---|---|---|
| Follicular thyroid carcinoma | |||
| YOUNGER THAN 55 YEARS | |||
| I | Any T | Any N | M0 |
| II | Any T | Any N | M1 |
| 55 YEARS AND OLDER | |||
| I | T1 | Any N | M0 |
| II | T1 | N1 | M0 |
| T2 | N1 | M0 | |
| T3a | Any N | M0 | |
| T3b | Any N | M0 | |
| III | T4a | Any N | M0 |
| IVA | T4b | Any N | M0 |
| IVB | Any T | Any N | M1 |
| T1 | N1 | M0 | |
| T2 | N1 | M0 | |
| T3a | N1 | M0 | |
| T3b | Any N | M0 | |
| T4 | Any N | M0 | |
| IVC | Any T | Any N | M1 |
Reference
- ↑ https://www.cancer.org/cancer/thyroid-cancer/detection-diagnosis-staging/how-diagnosed.html. Missing or empty
|title=(help) - ↑ http://librepathology.org/wiki/index.php/File:Metastatic_follicular_thyroid_carcinoma_-_Case_264_(8558730243).jpg Accessed on October, 29 2015
- ↑ http://librepathology.org/wiki/index.php/File:Metastatic_follicular_thyroid_carcinoma_-_Case_264_(8559837390).jpg Accessed on October, 29 2015
- ↑ "Thyroid Cancer Treatment (Adult) (PDQ®)–Health Professional Version - National Cancer Institute".
![Metastatic follicular thyroid carcinoma[2]](/images/b/b5/Metastatic_follicular_thyroid_carcinoma_-_Case_264_%288558730243%29.jpg)
![Metastatic follicular thyroid carcinoma[3]](/images/8/87/Metastatic_follicular_thyroid_carcinoma_-_Case_264.jpg)