Mantle cell lymphoma pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| (21 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{Akram}} {{AS}} | {{CMG}}; {{AE}} {{Akram}} {{AS}} | ||
==Overview== | ==Overview== | ||
The [[Chromosomal translocation|translocation]] t(11;14)(q13;q32) is considered the precipitating [[oncogenic]] event that induces [[cell cycle]] deregulation in mantle cell lymphoma due to overexpression of [[cyclin D1]]. In addition to the pathogonomic [[Chromosomal translocation|translocation]], [[MCL]] progression is controlled by secondary genetic abberations and dysregulated [[Signaling pathway|signaling pathways]] involved in [[DNA repair|DNA damage repair]], [[proliferation]], and [[apoptosis]]. | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
* The translocation t(11;14)(q13;q32) is considered the precipitating oncogenic event that induces cell cycle deregulation due to overexpression of cyclin D1. | * The [[Chromosomal translocation|translocation]] t(11;14)(q13;q32) is considered the precipitating [[oncogenic]] event that induces [[cell cycle]] deregulation due to overexpression of [[cyclin D1]]. | ||
* This translocation juxtaposes the CCDN1 gene encoding cyclin D1 to the immunoglobulin heavy chain (IgH) leading to its overexpression. However, less commonly, mutations in CCDN2 and CCDN3 have also been identified in cases of mantle cell lymphoma lacking the t(11;14) translocation.<ref>{{Cite journal | * This [[Chromosomal translocation|translocation]] juxtaposes the CCDN1 gene encoding [[cyclin D1]] to the [[immunoglobulin heavy chain]] (IgH) leading to its overexpression. However, less commonly, mutations in CCDN2 and CCDN3 have also been identified in cases of mantle cell lymphoma lacking the t(11;14) translocation.<ref>{{Cite journal | ||
| author = [[Itziar Salaverria]], [[Cristina Royo]], [[Alejandra Carvajal-Cuenca]], [[Guillem Clot]], [[Alba Navarro]], [[Alejandra Valera]], [[Joo Y. Song]], [[Renata Woroniecka]], [[Grzegorz Rymkiewicz]], [[Wolfram Klapper]], [[Elena M. Hartmann]], [[Pierre Sujobert]], [[Iwona Wlodarska]], [[Judith A. Ferry]], [[Philippe Gaulard]], [[German Ott]], [[Andreas Rosenwald]], [[Armando Lopez-Guillermo]], [[Leticia Quintanilla-Martinez]], [[Nancy L. Harris]], [[Elaine S. Jaffe]], [[Reiner Siebert]], [[Elias Campo]] & [[Silvia Bea]] | | author = [[Itziar Salaverria]], [[Cristina Royo]], [[Alejandra Carvajal-Cuenca]], [[Guillem Clot]], [[Alba Navarro]], [[Alejandra Valera]], [[Joo Y. Song]], [[Renata Woroniecka]], [[Grzegorz Rymkiewicz]], [[Wolfram Klapper]], [[Elena M. Hartmann]], [[Pierre Sujobert]], [[Iwona Wlodarska]], [[Judith A. Ferry]], [[Philippe Gaulard]], [[German Ott]], [[Andreas Rosenwald]], [[Armando Lopez-Guillermo]], [[Leticia Quintanilla-Martinez]], [[Nancy L. Harris]], [[Elaine S. Jaffe]], [[Reiner Siebert]], [[Elias Campo]] & [[Silvia Bea]] | ||
| title = CCND2 rearrangements are the most frequent genetic events in cyclin D1(-) mantle cell lymphoma | | title = CCND2 rearrangements are the most frequent genetic events in cyclin D1(-) mantle cell lymphoma | ||
| Line 20: | Line 22: | ||
| pmid = 23255553 | | pmid = 23255553 | ||
}}</ref> | }}</ref> | ||
* In addition to the pathogonomic translocation, MCL progression is controlled by secondary genetic abberations and dysregulated signaling pathways involved in DNA damage | * In addition to the pathogonomic [[Chromosomal translocation|translocation]], [[MCL]] progression is controlled by secondary genetic abberations and dysregulated [[Signaling pathway|signaling pathways]] involved in [[DNA repair|DNA damage repair]], [[proliferation]], and [[apoptosis]].<ref>{{Cite journal | ||
| author = [[Patricia Perez-Galan]], [[Martin Dreyling]] & [[Adrian Wiestner]] | | author = [[Patricia Perez-Galan]], [[Martin Dreyling]] & [[Adrian Wiestner]] | ||
| title = Mantle cell lymphoma: biology, pathogenesis, and the molecular basis of treatment in the genomic era | | title = Mantle cell lymphoma: biology, pathogenesis, and the molecular basis of treatment in the genomic era | ||
| Line 32: | Line 34: | ||
| pmid = 20940415 | | pmid = 20940415 | ||
}}</ref> | }}</ref> | ||
* | *These secondary genetic alterations and dysregulated signaling pathways are as follows: | ||
* | **Deregulation of [[cell cycle]]:<ref>{{Cite journal | ||
| author = [[Pedro Jares]], [[Dolors Colomer]] & [[Elias Campo]] | |||
| title = Molecular pathogenesis of mantle cell lymphoma | |||
| journal = [[The Journal of clinical investigation]] | |||
| volume = 122 | |||
| issue = 10 | |||
| pages = 3416–3423 | |||
| year = 2012 | |||
| month = October | |||
| doi = 10.1172/JCI61272 | |||
| pmid = 23023712 | |||
}}</ref> | |||
***INK4a/[[CDK4 gene|CDK4]]/[[RB1]] pathway | |||
***ARF/MDM2/p53 pathway | |||
**Deregulation of [[DNA repair|DNA damage repair]]:<ref>{{Cite journal | |||
| author = [[Silvia Bea]], [[Rafael Valdes-Mas]], [[Alba Navarro]], [[Itziar Salaverria]], [[David Martin-Garcia]], [[Pedro Jares]], [[Eva Gine]], [[Magda Pinyol]], [[Cristina Royo]], [[Ferran Nadeu]], [[Laura Conde]], [[Manel Juan]], [[Guillem Clot]], [[Pedro Vizan]], [[Luciano Di Croce]], [[Diana A. Puente]], [[Monica Lopez-Guerra]], [[Alexandra Moros]], [[Gael Roue]], [[Marta Aymerich]], [[Neus Villamor]], [[Lluis Colomo]], [[Antonio Martinez]], [[Alexandra Valera]], [[Jose I. Martin-Subero]], [[Virginia Amador]], [[Luis Hernandez]], [[Maria Rozman]], [[Anna Enjuanes]], [[Pilar Forcada]], [[Ana Muntanola]], [[Elena M. Hartmann]], [[Maria J. Calasanz]], [[Andreas Rosenwald]], [[German Ott]], [[Jesus M. Hernandez-Rivas]], [[Wolfram Klapper]], [[Reiner Siebert]], [[Adrian Wiestner]], [[Wyndham H. Wilson]], [[Dolors Colomer]], [[Armando Lopez-Guillermo]], [[Carlos Lopez-Otin]], [[Xose S. Puente]] & [[Elias Campo]] | |||
| title = Landscape of somatic mutations and clonal evolution in mantle cell lymphoma | |||
| journal = [[Proceedings of the National Academy of Sciences of the United States of America]] | |||
| volume = 110 | |||
| issue = 45 | |||
| pages = 18250–18255 | |||
| year = 2013 | |||
| month = November | |||
| doi = 10.1073/pnas.1314608110 | |||
| pmid = 24145436 | |||
}}</ref> | |||
***Mutation in [[ATM]] gene | |||
***Mutation in [[P53 gene|p53]] gene | |||
**Deregulation of [[apoptosis]]:<ref>{{Cite journal | |||
| author = [[J. M. Adams]] & [[S. Cory]] | |||
| title = The Bcl-2 apoptotic switch in cancer development and therapy | |||
| journal = [[Oncogene]] | |||
| volume = 26 | |||
| issue = 9 | |||
| pages = 1324–1337 | |||
| year = 2007 | |||
| month = February | |||
| doi = 10.1038/sj.onc.1210220 | |||
| pmid = 17322918 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Y. Li]], [[M. N. Bouchlaka]], [[J. Wolff]], [[K. M. Grindle]], [[L. Lu]], [[S. Qian]], [[X. Zhong]], [[N. Pflum]], [[P. Jobin]], [[B. S. Kahl]], [[J. C. Eickhoff]], [[S. M. Wuerzberger-Davis]], [[S. Miyamoto]], [[C. J. Thomas]], [[D. T. Yang]], [[C. M. Capitini]] & [[L. Rui]] | |||
| title = FBXO10 deficiency and BTK activation upregulate BCL2 expression in mantle cell lymphoma | |||
| journal = [[Oncogene]] | |||
| volume = 35 | |||
| issue = 48 | |||
| pages = 6223–6234 | |||
| year = 2016 | |||
| month = December | |||
| doi = 10.1038/onc.2016.155 | |||
| pmid = 27157620 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Joseph D. Khoury]], [[L. Jeffrey Medeiros]], [[George Z. Rassidakis]], [[Timothy J. McDonnell]], [[Lynne V. Abruzzo]] & [[Raymond Lai]] | |||
| title = Expression of Mcl-1 in mantle cell lymphoma is associated with high-grade morphology, a high proliferative state, and p53 overexpression | |||
| journal = [[The Journal of pathology]] | |||
| volume = 199 | |||
| issue = 1 | |||
| pages = 90–97 | |||
| year = 2003 | |||
| month = January | |||
| doi = 10.1002/path.1254 | |||
| pmid = 12474231 | |||
}}</ref> | |||
***[[BCL2-like 1 (gene)|BCL2]] amplifications | |||
***[[BCL2L11]] deletions | |||
***FBXO10 deficiency | |||
***[[MCL1]] overexpression | |||
**Deregulation of [[chromatin]] modifiers:<ref>{{Cite journal | |||
| author = [[Jenny Zhang]], [[Dereje Jima]], [[Andrea B. Moffitt]], [[Qingquan Liu]], [[Magdalena Czader]], [[Eric D. Hsi]], [[Yuri Fedoriw]], [[Cherie H. Dunphy]], [[Kristy L. Richards]], [[Javed I. Gill]], [[Zhen Sun]], [[Cassandra Love]], [[Paula Scotland]], [[Eric Lock]], [[Shawn Levy]], [[David S. Hsu]], [[David Dunson]] & [[Sandeep S. Dave]] | |||
| title = The genomic landscape of mantle cell lymphoma is related to the epigenetically determined chromatin state of normal B cells | |||
| journal = [[Blood]] | |||
| volume = 123 | |||
| issue = 19 | |||
| pages = 2988–2996 | |||
| year = 2014 | |||
| month = May | |||
| doi = 10.1182/blood-2013-07-517177 | |||
| pmid = 24682267 | |||
}}</ref> | |||
***[[WHSC1]] mutations | |||
***[[MLL2]] mutations | |||
***[[MEF2B]] mutations | |||
**Constitutive activation of [[oncogenic]] pathways:<ref>{{Cite journal | |||
| author = [[Lan V. Pham]], [[Archito T. Tamayo]], [[Linda C. Yoshimura]], [[Piao Lo]] & [[Richard J. Ford]] | |||
| title = Inhibition of constitutive NF-kappa B activation in mantle cell lymphoma B cells leads to induction of cell cycle arrest and apoptosis | |||
| journal = [[Journal of immunology (Baltimore, Md. : 1950)]] | |||
| volume = 171 | |||
| issue = 1 | |||
| pages = 88–95 | |||
| year = 2003 | |||
| month = July | |||
| pmid = 12816986 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Edgar Gil Rizzatti]], [[Roberto Passetto Falcao]], [[Rodrigo Alexandre Panepucci]], [[Rodrigo Proto-Siqueira]], [[Wilma Terezinha Anselmo-Lima]], [[Oswaldo Keith Okamoto]] & [[Marco Antonio Zago]] | |||
| title = Gene expression profiling of mantle cell lymphoma cells reveals aberrant expression of genes from the PI3K-AKT, WNT and TGFbeta signalling pathways | |||
| journal = [[British journal of haematology]] | |||
| volume = 130 | |||
| issue = 4 | |||
| pages = 516–526 | |||
| year = 2005 | |||
| month = August | |||
| doi = 10.1111/j.1365-2141.2005.05630.x | |||
| pmid = 16098065 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Robert Kridel]], [[Barbara Meissner]], [[Sanja Rogic]], [[Merrill Boyle]], [[Adele Telenius]], [[Bruce Woolcock]], [[Jay Gunawardana]], [[Christopher Jenkins]], [[Chris Cochrane]], [[Susana Ben-Neriah]], [[King Tan]], [[Ryan D. Morin]], [[Stephen Opat]], [[Laurie H. Sehn]], [[Joseph M. Connors]], [[Marco A. Marra]], [[Andrew P. Weng]], [[Christian Steidl]] & [[Randy D. Gascoyne]] | |||
| title = Whole transcriptome sequencing reveals recurrent NOTCH1 mutations in mantle cell lymphoma | |||
| journal = [[Blood]] | |||
| volume = 119 | |||
| issue = 9 | |||
| pages = 1963–1971 | |||
| year = 2012 | |||
| month = March | |||
| doi = 10.1182/blood-2011-11-391474 | |||
| pmid = 22210878 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Jamie N. Anastas]] & [[Randall T. Moon]] | |||
| title = WNT signalling pathways as therapeutic targets in cancer | |||
| journal = [[Nature reviews. Cancer]] | |||
| volume = 13 | |||
| issue = 1 | |||
| pages = 11–26 | |||
| year = 2013 | |||
| month = January | |||
| doi = 10.1038/nrc3419 | |||
| pmid = 23258168 | |||
}}</ref> | |||
***Classical [[NF-kB]] pathway | |||
***Alternate [[NF-kB]] pathway | |||
***[[PI3K]]/[[AKT]]/[[mTOR]] pathway | |||
***[[NOTCH1|NOTCH]] pathway | |||
***[[JAK-STAT signaling pathway|JAK/STAT3]] pathway | |||
***[[WNT1|WNT]] pathway | |||
*[[SOX11]], a [[SOX11|SOX]] family [[transcription factor]], has recently been identified as an important molecular feature of [[MCL]] regardless of [[cyclin D1]] status.<ref>{{Cite journal | |||
| author = [[Ana Mozos]], [[Cristina Royo]], [[Elena Hartmann]], [[Daphne De Jong]], [[Cristina Baro]], [[Alexandra Valera]], [[Kai Fu]], [[Dennis D. Weisenburger]], [[Jan Delabie]], [[Shih-Sung Chuang]], [[Elaine S. Jaffe]], [[Carmen Ruiz-Marcellan]], [[Sandeep Dave]], [[Lisa Rimsza]], [[Rita Braziel]], [[Randy D. Gascoyne]], [[Francisco Sole]], [[Armando Lopez-Guillermo]], [[Dolors Colomer]], [[Louis M. Staudt]], [[Andreas Rosenwald]], [[German Ott]], [[Pedro Jares]] & [[Elias Campo]] | |||
| title = SOX11 expression is highly specific for mantle cell lymphoma and identifies the cyclin D1-negative subtype | |||
| journal = [[Haematologica]] | |||
| volume = 94 | |||
| issue = 11 | |||
| pages = 1555–1562 | |||
| year = 2009 | |||
| month = November | |||
| doi = 10.3324/haematol.2009.010264 | |||
| pmid = 19880778 | |||
}}</ref> | |||
==Genetics== | ==Genetics== | ||
Genes involved in the pathogenesis of mantle cell lymphoma include: | [[Gene|Genes]] involved in the [[pathogenesis]] of mantle cell lymphoma include: | ||
*CCDN1 (primarily) | *CCDN1 (primarily) | ||
*CCDN2 ( | *CCDN2 | ||
* | *CCDN3 | ||
*[[CDK4]] | |||
*[[MDM2]] | |||
*[[BMI1]] | |||
*[[P53 (protein)|P53]] | |||
*[[ATM]] | |||
*[[BCL2-like 1 (gene)|BCL2]] | |||
*[[BCL2L11]] | |||
*FBXO10 | |||
*[[MCL1]] | |||
*[[WHSC1]] | |||
*[[MLL2]] | |||
*[[MEF2B]] | |||
== | ==Microscopic Pathology== | ||
*The typical (classical) morphology of mantle cell lymphoma is seen in about 90% of cases:<ref>{{Cite journal | |||
| author = [[Markus Tiemann]], [[Carsten Schrader]], [[Wolfram Klapper]], [[Martin H. Dreyling]], [[Elias Campo]], [[Andrew Norton]], [[Francoise Berger]], [[Philip Kluin]], [[German Ott]], [[Stephano Pileri]], [[Ennio Pedrinis]], [[Alfred C. Feller]], [[Hartmut Merz]], [[Dirk Janssen]], [[Martin L. Hansmann]], [[Han Krieken]], [[Peter Moller]], [[Harald Stein]], [[Michael Unterhalt]], [[Wolfgang Hiddemann]] & [[Reza Parwaresch]] | |||
| title = Histopathology, cell proliferation indices and clinical outcome in 304 patients with mantle cell lymphoma (MCL): a clinicopathological study from the European MCL Network | |||
| journal = [[British journal of haematology]] | |||
| volume = 131 | |||
| issue = 1 | |||
| pages = 29–38 | |||
| year = 2005 | |||
| month = October | |||
| doi = 10.1111/j.1365-2141.2005.05716.x | |||
| pmid = 16173960 | |||
}}</ref> | |||
**[[Cells]] are slightly larger than [[Lymphocyte|lymphocytes]]. | |||
**The [[nucleus]] is indented or bean-shaped. | |||
**Prominent [[Nucleolus|nucleoli]] are missing. | |||
**The [[chromatin]] structure is less condensed and not as bright as in [[Blast|blasts]] like centroblasts. | |||
**The [[Cytoplasmic|cytoplasmic rim]] is narrow and not [[basophilic]]. | |||
== | * The remaining 10% are the [[Morphology|morphological]] variants:<ref>{{Cite journal | ||
| author = [[Markus Tiemann]], [[Carsten Schrader]], [[Wolfram Klapper]], [[Martin H. Dreyling]], [[Elias Campo]], [[Andrew Norton]], [[Francoise Berger]], [[Philip Kluin]], [[German Ott]], [[Stephano Pileri]], [[Ennio Pedrinis]], [[Alfred C. Feller]], [[Hartmut Merz]], [[Dirk Janssen]], [[Martin L. Hansmann]], [[Han Krieken]], [[Peter Moller]], [[Harald Stein]], [[Michael Unterhalt]], [[Wolfgang Hiddemann]] & [[Reza Parwaresch]] | |||
| title = Histopathology, cell proliferation indices and clinical outcome in 304 patients with mantle cell lymphoma (MCL): a clinicopathological study from the European MCL Network | |||
| journal = [[British journal of haematology]] | |||
| volume = 131 | |||
| issue = 1 | |||
| pages = 29–38 | |||
| year = 2005 | |||
| month = October | |||
| doi = 10.1111/j.1365-2141.2005.05716.x | |||
| pmid = 16173960 | |||
}}</ref> | |||
** Small cell type''':''' They resemble [[CLL]] [[Cytology|cytologically]] but the [[prolymphocytes]] and paraimmunoblasts are usually missing. This variant usually shows a very low proliferative activity. | |||
** [[Pleomorphic]] and blastic type(together known as the [[blastoid]] variant): The [[pleomorphic]] type are similar to [[Diffuse large B cell lymphoma|diffuse large B-cell lymphoma]] ([[DLBCL]]). The blastic type resemble [[lymphoblastic lymphoma]] or [[Lymphoid leukemia|leukemia]] and have monomorphic roundish [[Blast|blasts]]. The [[blastoid]] variant usually have numerous [[mitotic]] figures and are very highly proliferative. | |||
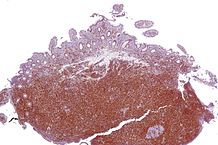
* Scattered non-granumloma forming [[epithelioid]] [[macrophages]], hyalinized vessels and a few reactive [[T cells]] or [[mast cells]] are seen along with the [[lymphoma]] [[cells]] in [[MCL]]. [[Follicular dendritic cells]] (FDC) are a hallmark of mantle cell lymphoma and may also be involved in its [[pathogenesis]].<ref>{{Cite journal | |||
| author = [[Carsten Schrader]], [[Peter Meusers]], [[Gunter Brittinger]], [[Dirk Janssen]], [[Afshin Teymoortash]], [[Jens U. Siebmann]], [[Reza Parwaresch]] & [[Markus Tiemann]] | |||
| title = Growth pattern and distribution of follicular dendritic cells in mantle cell lymphoma: a clinicopathological study of 96 patients | |||
| journal = [[Virchows Archiv : an international journal of pathology]] | |||
| volume = 448 | |||
| issue = 2 | |||
| pages = 151–159 | |||
| year = 2006 | |||
| month = February | |||
| doi = 10.1007/s00428-005-0049-5 | |||
| pmid = 16133361 | |||
}}</ref> | |||
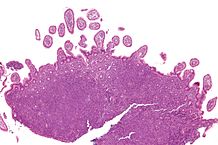
* Three types of growth pattern are observed in mantle cell lymphoma:<ref>{{Cite journal | |||
| author = [[L. H. Argatoff]], [[J. M. Connors]], [[R. J. Klasa]], [[D. E. Horsman]] & [[R. D. Gascoyne]] | |||
| title = Mantle cell lymphoma: a clinicopathologic study of 80 cases | |||
| journal = [[Blood]] | |||
| volume = 89 | |||
| issue = 6 | |||
| pages = 2067–2078 | |||
| year = 1997 | |||
| month = March | |||
| pmid = 9058729 | |||
}}</ref> | |||
**[[Mantle zone]]: [[Nodular]] with [[germinal centers]] | |||
**[[Nodular]]: >50% nodular growth | |||
**Diffuse: <50% nodular growth | |||
==References== | ==References== | ||
| Line 53: | Line 263: | ||
{{WS}} | {{WS}} | ||
[[Category: (name of the system)]] | [[Category: (name of the system)]] | ||
<gallery widths="200px"> | <gallery widths="200px"> | ||
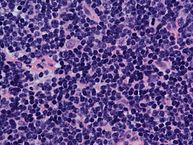
Image:97px-Mantle cell lymphoma - intermed mag.jpg|Intermediate magnification micrograph of mantle cell lymphoma of the terminal ileum. Endoscopic biopsy. H&E stain. Histomorphologic features: Monomorphic small lymphoid cells less than twice the size of a resting lymphocyte. Abundant mitoses. Sclerosed blood vessels. Scattered epithelioid histiocytes. | Image:97px-Mantle cell lymphoma - intermed mag.jpg|Intermediate magnification micrograph of mantle cell lymphoma of the terminal ileum. Endoscopic biopsy. H&E stain. Histomorphologic features: Monomorphic small lymphoid cells less than twice the size of a resting lymphocyte. Abundant mitoses. Sclerosed blood vessels. Scattered epithelioid histiocytes. | ||
Latest revision as of 19:44, 7 January 2019
|
Mantle cell lymphoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mantle cell lymphoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Mantle cell lymphoma pathophysiology |
|
Risk calculators and risk factors for Mantle cell lymphoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ali Akram, M.B.B.S.[2] Sowminya Arikapudi, M.B,B.S. [3]
Overview
The translocation t(11;14)(q13;q32) is considered the precipitating oncogenic event that induces cell cycle deregulation in mantle cell lymphoma due to overexpression of cyclin D1. In addition to the pathogonomic translocation, MCL progression is controlled by secondary genetic abberations and dysregulated signaling pathways involved in DNA damage repair, proliferation, and apoptosis.
Pathophysiology
Pathogenesis
- The translocation t(11;14)(q13;q32) is considered the precipitating oncogenic event that induces cell cycle deregulation due to overexpression of cyclin D1.
- This translocation juxtaposes the CCDN1 gene encoding cyclin D1 to the immunoglobulin heavy chain (IgH) leading to its overexpression. However, less commonly, mutations in CCDN2 and CCDN3 have also been identified in cases of mantle cell lymphoma lacking the t(11;14) translocation.[1]
- In addition to the pathogonomic translocation, MCL progression is controlled by secondary genetic abberations and dysregulated signaling pathways involved in DNA damage repair, proliferation, and apoptosis.[2]
- These secondary genetic alterations and dysregulated signaling pathways are as follows:
- SOX11, a SOX family transcription factor, has recently been identified as an important molecular feature of MCL regardless of cyclin D1 status.[13]
Genetics
Genes involved in the pathogenesis of mantle cell lymphoma include:
Microscopic Pathology
- The typical (classical) morphology of mantle cell lymphoma is seen in about 90% of cases:[14]
- Cells are slightly larger than lymphocytes.
- The nucleus is indented or bean-shaped.
- Prominent nucleoli are missing.
- The chromatin structure is less condensed and not as bright as in blasts like centroblasts.
- The cytoplasmic rim is narrow and not basophilic.
- The remaining 10% are the morphological variants:[15]
- Small cell type: They resemble CLL cytologically but the prolymphocytes and paraimmunoblasts are usually missing. This variant usually shows a very low proliferative activity.
- Pleomorphic and blastic type(together known as the blastoid variant): The pleomorphic type are similar to diffuse large B-cell lymphoma (DLBCL). The blastic type resemble lymphoblastic lymphoma or leukemia and have monomorphic roundish blasts. The blastoid variant usually have numerous mitotic figures and are very highly proliferative.
- Scattered non-granumloma forming epithelioid macrophages, hyalinized vessels and a few reactive T cells or mast cells are seen along with the lymphoma cells in MCL. Follicular dendritic cells (FDC) are a hallmark of mantle cell lymphoma and may also be involved in its pathogenesis.[16]
- Three types of growth pattern are observed in mantle cell lymphoma:[17]
- Mantle zone: Nodular with germinal centers
- Nodular: >50% nodular growth
- Diffuse: <50% nodular growth
References
- ↑ Itziar Salaverria, Cristina Royo, Alejandra Carvajal-Cuenca, Guillem Clot, Alba Navarro, Alejandra Valera, Joo Y. Song, Renata Woroniecka, Grzegorz Rymkiewicz, Wolfram Klapper, Elena M. Hartmann, Pierre Sujobert, Iwona Wlodarska, Judith A. Ferry, Philippe Gaulard, German Ott, Andreas Rosenwald, Armando Lopez-Guillermo, Leticia Quintanilla-Martinez, Nancy L. Harris, Elaine S. Jaffe, Reiner Siebert, Elias Campo & Silvia Bea (2013). "CCND2 rearrangements are the most frequent genetic events in cyclin D1(-) mantle cell lymphoma". Blood. 121 (8): 1394–1402. doi:10.1182/blood-2012-08-452284. PMID 23255553. Unknown parameter
|month=ignored (help) - ↑ Patricia Perez-Galan, Martin Dreyling & Adrian Wiestner (2011). "Mantle cell lymphoma: biology, pathogenesis, and the molecular basis of treatment in the genomic era". Blood. 117 (1): 26–38. doi:10.1182/blood-2010-04-189977. PMID 20940415. Unknown parameter
|month=ignored (help) - ↑ Pedro Jares, Dolors Colomer & Elias Campo (2012). "Molecular pathogenesis of mantle cell lymphoma". The Journal of clinical investigation. 122 (10): 3416–3423. doi:10.1172/JCI61272. PMID 23023712. Unknown parameter
|month=ignored (help) - ↑ Silvia Bea, Rafael Valdes-Mas, Alba Navarro, Itziar Salaverria, David Martin-Garcia, Pedro Jares, Eva Gine, Magda Pinyol, Cristina Royo, Ferran Nadeu, Laura Conde, Manel Juan, Guillem Clot, Pedro Vizan, Luciano Di Croce, Diana A. Puente, Monica Lopez-Guerra, Alexandra Moros, Gael Roue, Marta Aymerich, Neus Villamor, Lluis Colomo, Antonio Martinez, Alexandra Valera, Jose I. Martin-Subero, Virginia Amador, Luis Hernandez, Maria Rozman, Anna Enjuanes, Pilar Forcada, Ana Muntanola, Elena M. Hartmann, Maria J. Calasanz, Andreas Rosenwald, German Ott, Jesus M. Hernandez-Rivas, Wolfram Klapper, Reiner Siebert, Adrian Wiestner, Wyndham H. Wilson, Dolors Colomer, Armando Lopez-Guillermo, Carlos Lopez-Otin, Xose S. Puente & Elias Campo (2013). "Landscape of somatic mutations and clonal evolution in mantle cell lymphoma". Proceedings of the National Academy of Sciences of the United States of America. 110 (45): 18250–18255. doi:10.1073/pnas.1314608110. PMID 24145436. Unknown parameter
|month=ignored (help) - ↑ J. M. Adams & S. Cory (2007). "The Bcl-2 apoptotic switch in cancer development and therapy". Oncogene. 26 (9): 1324–1337. doi:10.1038/sj.onc.1210220. PMID 17322918. Unknown parameter
|month=ignored (help) - ↑ Y. Li, M. N. Bouchlaka, J. Wolff, K. M. Grindle, L. Lu, S. Qian, X. Zhong, N. Pflum, P. Jobin, B. S. Kahl, J. C. Eickhoff, S. M. Wuerzberger-Davis, S. Miyamoto, C. J. Thomas, D. T. Yang, C. M. Capitini & L. Rui (2016). "FBXO10 deficiency and BTK activation upregulate BCL2 expression in mantle cell lymphoma". Oncogene. 35 (48): 6223–6234. doi:10.1038/onc.2016.155. PMID 27157620. Unknown parameter
|month=ignored (help) - ↑ Joseph D. Khoury, L. Jeffrey Medeiros, George Z. Rassidakis, Timothy J. McDonnell, Lynne V. Abruzzo & Raymond Lai (2003). "Expression of Mcl-1 in mantle cell lymphoma is associated with high-grade morphology, a high proliferative state, and p53 overexpression". The Journal of pathology. 199 (1): 90–97. doi:10.1002/path.1254. PMID 12474231. Unknown parameter
|month=ignored (help) - ↑ Jenny Zhang, Dereje Jima, Andrea B. Moffitt, Qingquan Liu, Magdalena Czader, Eric D. Hsi, Yuri Fedoriw, Cherie H. Dunphy, Kristy L. Richards, Javed I. Gill, Zhen Sun, Cassandra Love, Paula Scotland, Eric Lock, Shawn Levy, David S. Hsu, David Dunson & Sandeep S. Dave (2014). "The genomic landscape of mantle cell lymphoma is related to the epigenetically determined chromatin state of normal B cells". Blood. 123 (19): 2988–2996. doi:10.1182/blood-2013-07-517177. PMID 24682267. Unknown parameter
|month=ignored (help) - ↑ Lan V. Pham, Archito T. Tamayo, Linda C. Yoshimura, Piao Lo & Richard J. Ford (2003). "Inhibition of constitutive NF-kappa B activation in mantle cell lymphoma B cells leads to induction of cell cycle arrest and apoptosis". Journal of immunology (Baltimore, Md. : 1950). 171 (1): 88–95. PMID 12816986. Unknown parameter
|month=ignored (help) - ↑ Edgar Gil Rizzatti, Roberto Passetto Falcao, Rodrigo Alexandre Panepucci, Rodrigo Proto-Siqueira, Wilma Terezinha Anselmo-Lima, Oswaldo Keith Okamoto & Marco Antonio Zago (2005). "Gene expression profiling of mantle cell lymphoma cells reveals aberrant expression of genes from the PI3K-AKT, WNT and TGFbeta signalling pathways". British journal of haematology. 130 (4): 516–526. doi:10.1111/j.1365-2141.2005.05630.x. PMID 16098065. Unknown parameter
|month=ignored (help) - ↑ Robert Kridel, Barbara Meissner, Sanja Rogic, Merrill Boyle, Adele Telenius, Bruce Woolcock, Jay Gunawardana, Christopher Jenkins, Chris Cochrane, Susana Ben-Neriah, King Tan, Ryan D. Morin, Stephen Opat, Laurie H. Sehn, Joseph M. Connors, Marco A. Marra, Andrew P. Weng, Christian Steidl & Randy D. Gascoyne (2012). "Whole transcriptome sequencing reveals recurrent NOTCH1 mutations in mantle cell lymphoma". Blood. 119 (9): 1963–1971. doi:10.1182/blood-2011-11-391474. PMID 22210878. Unknown parameter
|month=ignored (help) - ↑ Jamie N. Anastas & Randall T. Moon (2013). "WNT signalling pathways as therapeutic targets in cancer". Nature reviews. Cancer. 13 (1): 11–26. doi:10.1038/nrc3419. PMID 23258168. Unknown parameter
|month=ignored (help) - ↑ Ana Mozos, Cristina Royo, Elena Hartmann, Daphne De Jong, Cristina Baro, Alexandra Valera, Kai Fu, Dennis D. Weisenburger, Jan Delabie, Shih-Sung Chuang, Elaine S. Jaffe, Carmen Ruiz-Marcellan, Sandeep Dave, Lisa Rimsza, Rita Braziel, Randy D. Gascoyne, Francisco Sole, Armando Lopez-Guillermo, Dolors Colomer, Louis M. Staudt, Andreas Rosenwald, German Ott, Pedro Jares & Elias Campo (2009). "SOX11 expression is highly specific for mantle cell lymphoma and identifies the cyclin D1-negative subtype". Haematologica. 94 (11): 1555–1562. doi:10.3324/haematol.2009.010264. PMID 19880778. Unknown parameter
|month=ignored (help) - ↑ Markus Tiemann, Carsten Schrader, Wolfram Klapper, Martin H. Dreyling, Elias Campo, Andrew Norton, Francoise Berger, Philip Kluin, German Ott, Stephano Pileri, Ennio Pedrinis, Alfred C. Feller, Hartmut Merz, Dirk Janssen, Martin L. Hansmann, Han Krieken, Peter Moller, Harald Stein, Michael Unterhalt, Wolfgang Hiddemann & Reza Parwaresch (2005). "Histopathology, cell proliferation indices and clinical outcome in 304 patients with mantle cell lymphoma (MCL): a clinicopathological study from the European MCL Network". British journal of haematology. 131 (1): 29–38. doi:10.1111/j.1365-2141.2005.05716.x. PMID 16173960. Unknown parameter
|month=ignored (help) - ↑ Markus Tiemann, Carsten Schrader, Wolfram Klapper, Martin H. Dreyling, Elias Campo, Andrew Norton, Francoise Berger, Philip Kluin, German Ott, Stephano Pileri, Ennio Pedrinis, Alfred C. Feller, Hartmut Merz, Dirk Janssen, Martin L. Hansmann, Han Krieken, Peter Moller, Harald Stein, Michael Unterhalt, Wolfgang Hiddemann & Reza Parwaresch (2005). "Histopathology, cell proliferation indices and clinical outcome in 304 patients with mantle cell lymphoma (MCL): a clinicopathological study from the European MCL Network". British journal of haematology. 131 (1): 29–38. doi:10.1111/j.1365-2141.2005.05716.x. PMID 16173960. Unknown parameter
|month=ignored (help) - ↑ Carsten Schrader, Peter Meusers, Gunter Brittinger, Dirk Janssen, Afshin Teymoortash, Jens U. Siebmann, Reza Parwaresch & Markus Tiemann (2006). "Growth pattern and distribution of follicular dendritic cells in mantle cell lymphoma: a clinicopathological study of 96 patients". Virchows Archiv : an international journal of pathology. 448 (2): 151–159. doi:10.1007/s00428-005-0049-5. PMID 16133361. Unknown parameter
|month=ignored (help) - ↑ L. H. Argatoff, J. M. Connors, R. J. Klasa, D. E. Horsman & R. D. Gascoyne (1997). "Mantle cell lymphoma: a clinicopathologic study of 80 cases". Blood. 89 (6): 2067–2078. PMID 9058729. Unknown parameter
|month=ignored (help)
-
Intermediate magnification micrograph of mantle cell lymphoma of the terminal ileum. Endoscopic biopsy. H&E stain. Histomorphologic features: Monomorphic small lymphoid cells less than twice the size of a resting lymphocyte. Abundant mitoses. Sclerosed blood vessels. Scattered epithelioid histiocytes.
-
Mantle cell lymphoma. Notice the irregular nuclear contours of the medium-sized lymphoma cells and the presence of a pink histiocyte. By immunohistochemistry the lymphoma cells expressed CD20, CD5 and Cyclin D1 (high power view, H&E).
-
Lymph node with mantle cell lymphoma (low power view, H&E).
-
Micrograph of terminal ileum with mantle cell lymphoma (bottom of image). H&E stain.
-
Micrograph of terminal ileum with mantle cell lymphoma (bottom of image - brown colour). Cyclin D1 immunostain.