Brugada syndrome: Difference between revisions
Sara Mohsin (talk | contribs) No edit summary |
|||
| (40 intermediate revisions by 8 users not shown) | |||
| Line 3: | Line 3: | ||
Name = Brugada syndrome | | Name = Brugada syndrome | | ||
Image = BrugadaS.jpg| | Image = BrugadaS.jpg| | ||
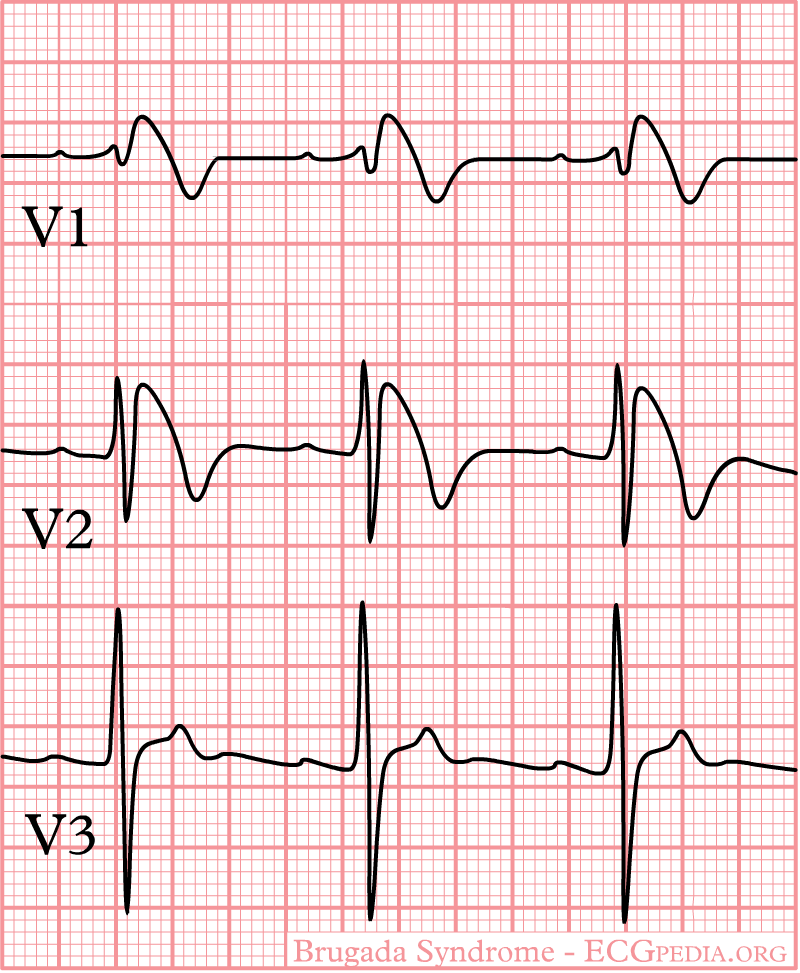
Caption = ECG | Caption = ECG in Type I Brugada Pattern| | ||
}} | }} | ||
'''For patient information, click [[Brugada syndrome (patient information)|here]]''' | |||
{{Brugada syndrome}} | {{Brugada syndrome}} | ||
| Line 17: | Line 11: | ||
{{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | ||
{{SK}} Sudden unexpected death syndrome; SUDS | {{SK}} Sudden unexpected death syndrome; sudden unexplained death syndrome; SUDS; sudden unexpected nocturnal death syndrome; sudden unexplained nocturnal death syndrome; SUNDS; in the Phillipines ''bangungut'' (to rise and moan in sleep); in Thailand ''lai tai''; in Laos ''Dab tsog'' and in Japan ''Pokkuri disease'' | ||
== | ==[[Brugada syndrome overview|Overview]]== | ||
==[[Brugada syndrome classification|Classification]]== | |||
== | ==[[Brugada syndrome historical perspective|Historical Perspective]]== | ||
== | ==[[Brugada syndrome pathophysiology|Pathophysiology]]== | ||
== | ==[[Brugada syndrome differential diagnosis|Differentiating Brugada syndrome from other Diseases]]== | ||
==[[Brugada syndrome epidemiology and demographics|Epidemiology and Demographics]]== | |||
== | ==[[Brugada syndrome risk factors|Risk Factors]]== | ||
==[[Brugada syndrome screening|Screening]]== | |||
==[[Brugada syndrome natural history, complications and prognosis|Natural History, Complications and Prognosis]]== | |||
==Brugada syndrome diagnosis|Diagnosis== | |||
[[Brugada syndrome diagnostic criteria|Diagnostic Criteria]] | [[Brugada syndrome history and symptoms|History and Symptoms]] | [[Brugada syndrome physical examination|Physical Examination]] | [[Brugada syndrome laboratory findings|Laboratory Findings]] | [[Brugada syndrome electrocardiogram|Electrocardiogram]] | [[Brugada syndrome chest x ray|Chest X Ray]] | [[Brugada syndrome echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Brugada syndrome electrophysiologic studies|Electrophysiologic Studies]] | [[Brugada syndrome genetic testing|Genetic Testing]] | |||
==Treatment== | ==Treatment== | ||
[[Brugada syndrome medical therapy|Medical Therapy]] | [[Brugada syndrome drugs to avoid|Drugs to Avoid]] | [[Brugada syndrome drugs to preferably avoid|Drugs to Preferably Avoid]] | [[Brugada syndrome cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Brugada syndrome future or investigational therapies|Future or Investigational Therapies]] | |||
==Case Studies== | |||
[[Brugada syndrome case study one|Case #1]] | |||
== | ==Related Chapters== | ||
* [[Cardiac action potential]] | * [[Cardiac action potential]] | ||
* [[Genetics]] | * [[Genetics]] | ||
* [[Ion channel]] | * [[Ion channel]] | ||
* [[Tambocor]] | * [[Tambocor]] | ||
{{Electrocardiography}} | {{Electrocardiography}} | ||
| Line 91: | Line 60: | ||
[[zh:布魯格達氏症候群]] | [[zh:布魯格達氏症候群]] | ||
[[tr:Brugada sendromu]] | [[tr:Brugada sendromu]] | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[CME Category::Cardiology]] | |||
[[Category:Electrophysiology]] | [[Category:Electrophysiology]] | ||
| Line 96: | Line 69: | ||
[[Category:Channelopathy]] | [[Category:Channelopathy]] | ||
[[Category:Genetic disorders]] | [[Category:Genetic disorders]] | ||
Latest revision as of 05:04, 20 August 2020
| Brugada syndrome | |
 | |
|---|---|
| ECG in Type I Brugada Pattern |
For patient information, click here
|
Brugada syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Brugada syndrome On the Web |
|
American Roentgen Ray Society Images of Brugada syndrome |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: Sudden unexpected death syndrome; sudden unexplained death syndrome; SUDS; sudden unexpected nocturnal death syndrome; sudden unexplained nocturnal death syndrome; SUNDS; in the Phillipines bangungut (to rise and moan in sleep); in Thailand lai tai; in Laos Dab tsog and in Japan Pokkuri disease
Overview
Classification
Historical Perspective
Pathophysiology
Differentiating Brugada syndrome from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications and Prognosis
Brugada syndrome diagnosis|Diagnosis
Diagnostic Criteria | History and Symptoms | Physical Examination | Laboratory Findings | Electrocardiogram | Chest X Ray | Echocardiography or Ultrasound | Electrophysiologic Studies | Genetic Testing
Treatment
Medical Therapy | Drugs to Avoid | Drugs to Preferably Avoid | Cost-Effectiveness of Therapy | Future or Investigational Therapies
Case Studies
Related Chapters
de:Brugada-Syndrom
it:Sindrome di Brugada
he:תסמונת ברוגדה
fi:Brugadan oireyhtymä