Candida auris infection: Difference between revisions
(→Causes) |
Tarek Nafee (talk | contribs) |
||
| (22 intermediate revisions by 3 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
''Candida auris'' is a fungus, recently described as a rare cause of fungal infection with significant resistance to [[antifungal medications]].<ref name="pmidPMID 24357342">{{cite journal| author=Chowdhary A, Anil Kumar V, Sharma C, Prakash A, Agarwal K, Babu R et al.| title=Multidrug-resistant endemic clonal strain of Candida auris in India. | journal=Eur J Clin Microbiol Infect Dis | year= 2014 | volume= 33 | issue= 6 | pages= 919-26 | pmid=PMID 24357342 | doi=10.1007/s10096-013-2027-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24357342 }} </ref> It was first described in the year 2009 in Japan,<ref name="pmidPMID 27832049">{{cite journal| author=Vallabhaneni S, Kallen A, Tsay S, Chow N, Welsh R, Kerins J et al.| title=Investigation of the First Seven Reported Cases of Candida auris, a Globally Emerging Invasive, Multidrug-Resistant Fungus - United States, May 2013-August 2016. | journal=MMWR Morb Mortal Wkly Rep | year= 2016 | volume= 65 | issue= 44 | pages= 1234-1237 | pmid=PMID 27832049 | doi=10.15585/mmwr.mm6544e1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27832049 }} </ref> and since then, reports of ''C. auris'' infection has been published from several countries.<ref name="pmidPMID 27832049" /> However, retrospective testing of collected isolates show the earliest known infection with C. auris occurred in South Korea in 1996.<ref name="cdc2"/><ref name="pmid21715586" /> Serious and prolonged outbreaks have been documented with data showing an innate resilience of ''C.auris'' for survival, persistence in the clinical environment with the ability to rapidly colonize | ''Candida auris'' is a [[fungus]], recently described as a rare cause of [[fungal infection]] with significant resistance to [[Antifungal medication|antifungal medications]].<ref name="pmidPMID 24357342">{{cite journal| author=Chowdhary A, Anil Kumar V, Sharma C, Prakash A, Agarwal K, Babu R et al.| title=Multidrug-resistant endemic clonal strain of Candida auris in India. | journal=Eur J Clin Microbiol Infect Dis | year= 2014 | volume= 33 | issue= 6 | pages= 919-26 | pmid=PMID 24357342 | doi=10.1007/s10096-013-2027-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24357342 }} </ref> It was first described in the year 2009 in Japan,<ref name="pmidPMID 27832049">{{cite journal| author=Vallabhaneni S, Kallen A, Tsay S, Chow N, Welsh R, Kerins J et al.| title=Investigation of the First Seven Reported Cases of Candida auris, a Globally Emerging Invasive, Multidrug-Resistant Fungus - United States, May 2013-August 2016. | journal=MMWR Morb Mortal Wkly Rep | year= 2016 | volume= 65 | issue= 44 | pages= 1234-1237 | pmid=PMID 27832049 | doi=10.15585/mmwr.mm6544e1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27832049 }} </ref> and since then, reports of ''C. auris'' infection has been published from several countries.<ref name="pmidPMID 27832049" /> However, retrospective testing of collected isolates show the earliest known infection with ''C. auris'' occurred in South Korea in 1996.<ref name="cdc2"/><ref name="pmid21715586" /> Serious and prolonged [[outbreaks]] have been documented with data showing an innate resilience of ''C. auris'' for survival, persistence in the clinical environment with the ability to rapidly colonize the skin of patients, and high transmissibility within the healthcare system.<ref name="pmidPMID 27777756" /> The first reported case in Europe involved over fifty cases in a span of more than sixteen months in a cardiothoracic center in London, and it is the largest [[outbreak]] in Europe.<ref name="pmidPMID 27777756" /> The precise mode of transmission within the healthcare facility is unknown.<ref name="cdc1">Centers for Disease Control and Prevention. https://www.cdc.gov/fungal/diseases/candidiasis/candida-auris-alert.html Accessed on November 11th, 2016. </ref><ref name=cdc2>Public Health England.https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/534174/Guidance_Candida__auris.pdf. Accessed on November 11th, 2016.</ref> The high rate of therapeutic failure noted in cases of ''Candida auris'' [[fungemia]] poses significant concerns.<ref name="pmidPMID 24357342" /> Misidentification of ''C. auris'' with related ''[[Candida]]'' species such as ''[[Candida|Candida haemulonii]]'' by commercially available biochemical-based tests poses a challenge.<ref name="cdc1" /> ''C. auris'' is recognized as a globally emerging fungal [[pathogen]] and it requires reproducible laboratory methods for identification and typing.<ref name="pmidPMID 26548511">{{cite journal| author=Prakash A, Sharma C, Singh A, Kumar Singh P, Kumar A, Hagen F et al.| title=Evidence of genotypic diversity among Candida auris isolates by multilocus sequence typing, matrix-assisted laser desorption ionization time-of-flight mass spectrometry and amplified fragment length polymorphism. | journal=Clin Microbiol Infect | year= 2016 | volume= 22 | issue= 3 | pages= 277.e1-9 | pmid=PMID 26548511 | doi=10.1016/j.cmi.2015.10.022 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26548511 }} </ref><ref name="pmidPMID 27777756">{{cite journal| author=Schelenz S, Hagen F, Rhodes JL, Abdolrasouli A, Chowdhary A, Hall A et al.| title=First hospital outbreak of the globally emerging Candida auris in a European hospital. | journal=Antimicrob Resist Infect Control | year= 2016 | volume= 5 | issue= | pages= 35 | pmid=PMID 27777756 | doi=10.1186/s13756-016-0132-5 | pmc=5069812 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27777756 }} </ref> Institution of key infection prevention and control measures,<ref name="cdc2" /> correct identification and standardized [[antifungal]] susceptibility testing for optimal management strategies of patients with invasive [[infections]] can hardly be overemphasized.<ref name="cdc2" /> | ||
==Historical Perspective== | ==Historical Perspective== | ||
* ''C. auris'' was first described in 2009 after being isolated from the external ear canal discharge of a patient in Japan.<ref name="pmidPMID 27832049" /> | * ''C. auris'' was first described in 2009 after being isolated from the external [[ear canal]] [[discharge]] of a patient in Japan.<ref name="pmidPMID 27832049" /> | ||
* The first report of blood stream infection by ''C. auris'' was in 2011 from Korea.<ref name="pmid27634564" /> | * The first report of [[blood stream]] [[infection]] by ''C. auris'' was in 2011 from Korea.<ref name="pmid27634564" /> | ||
* ''C. auris'' was incidentally found by molecular identification of bloodstream isolates of unidentified yeasts recovered in 1996, suggesting the paucity of isolation of ''C. auris'' may partly reflect the difficulty in identifying the | * ''C. auris'' was incidentally found by molecular identification of [[bloodstream]] isolates of unidentified [[Yeast|yeasts]] recovered in 1996, suggesting the paucity of isolation of ''C. auris'' may partly reflect the difficulty in identifying the [[species]].<ref name="pmid21715586">{{cite journal| author=Lee WG, Shin JH, Uh Y, Kang MG, Kim SH, Park KH et al.| title=First three reported cases of nosocomial fungemia caused by Candida auris. | journal=J Clin Microbiol | year= 2011 | volume= 49 | issue= 9 | pages= 3139-42 | pmid=21715586 | doi=10.1128/JCM.00319-11 | pmc=3165631 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21715586 }} </ref> | ||
* The occurrence of ''C. auris'' in at least nine countries on four continents since 2009 has been reported.<ref name="cdc1" /> | * The occurrence of ''C. auris'' in at least nine countries on four continents since 2009 has been reported.<ref name="cdc1" /> | ||
* ''C. auris'' infections have most commonly been hospital-acquired and occurred several weeks into a patient’s hospital stay.<ref name="cdc1" /> | * ''C. auris'' infections have most commonly been [[Hospital-acquired infection|hospital-acquired]] and occurred several weeks into a patient’s hospital stay.<ref name="cdc1" /> | ||
* It has been documented to cause infection in patients of all ages.<ref name="cdc1" /><ref name="pmid21715586" /><ref name="pmidPMID 25989098">{{cite journal| author=Emara M, Ahmad S, Khan Z, Joseph L, Al-Obaid I, Purohit P et al.| title=Candida auris candidemia in Kuwait, 2014. | journal=Emerg Infect Dis | year= 2015 | volume= 21 | issue= 6 | pages= 1091-2 | pmid=PMID 25989098 | doi=10.3201/eid2106.150270 | pmc=4451886 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25989098 }} </ref> | * It has been documented to cause infection in patients of all ages.<ref name="cdc1" /><ref name="pmid21715586" /><ref name="pmidPMID 25989098">{{cite journal| author=Emara M, Ahmad S, Khan Z, Joseph L, Al-Obaid I, Purohit P et al.| title=Candida auris candidemia in Kuwait, 2014. | journal=Emerg Infect Dis | year= 2015 | volume= 21 | issue= 6 | pages= 1091-2 | pmid=PMID 25989098 | doi=10.3201/eid2106.150270 | pmc=4451886 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25989098 }} </ref> | ||
== Causes == | == Causes == | ||
''Candida auris'' infection is caused by ''C. auris;'' an ascomycetous yeast | ''Candida auris'' infection is caused by ''C. auris;'' an [[Ascomycota|ascomycetous]] [[yeast]] [[species]] belonging to the genus ''[[Candida]]'', and it has a high potential for [[nosocomial]] horizontal transmission.<ref name="pmidPMID 27777756" /><ref name="pmidPMID 27452195">{{cite journal| author=Calvo B, Melo AS, Perozo-Mena A, Hernandez M, Francisco EC, Hagen F et al.| title=First report of Candida auris in America: Clinical and microbiological aspects of 18 episodes of candidemia. | journal=J Infect | year= 2016 | volume= 73 | issue= 4 | pages= 369-74 | pmid=PMID 27452195 | doi=10.1016/j.jinf.2016.07.008 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27452195 }} </ref><ref name="pmid19161556">{{cite journal| author=Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H| title=Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. | journal=Microbiol Immunol | year= 2009 | volume= 53 | issue= 1 | pages= 41-4 | pmid=19161556 | doi=10.1111/j.1348-0421.2008.00083.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19161556 }} </ref> | ||
==Pathophysiology== | ==Pathophysiology== | ||
=== Pathogenesis === | === Pathogenesis === | ||
* ''C. auris'' cases have been identified from clinical sites such as wound swabs, urine samples, vascular devices tips, blood cultures as well as skin screening samples (including nose, oropharynx, axilla, groin and stool samples).<ref name="pmidPMID 27777756" /> | * ''C. auris'' cases have been identified from clinical sites such as wound swabs, urine samples, vascular devices tips, blood cultures as well as skin screening samples (including nose, [[oropharynx]], axilla, [[groin]] and stool samples).<ref name="pmidPMID 27777756" /> | ||
* ''C. auris'' has been reported to cause bloodstream infections, wound infections, and [[otitis media]].<ref name="cdc1" /><ref name="pmid21715586" /> | * ''C. auris'' has been reported to cause [[bloodstream]] infections, wound infections, and [[otitis media]].<ref name="cdc1" /><ref name="pmid21715586" /> | ||
* The occurrence of [[candidemia]] attributed to ''C. auris'' appears increasingly common.<ref name="pmidPMID 27777756" /> | * The occurrence of [[candidemia]] attributed to ''C. auris'' appears increasingly common.<ref name="pmidPMID 27777756" /> | ||
* Evidence of distinct geographic clustering of ''Candida auris'' isolates has been established.<ref name="pmidPMID 26548511" /> | * Evidence of distinct geographic clustering of ''Candida auris'' isolates has been established.<ref name="pmidPMID 26548511" /> | ||
* ''C. auris'' has been isolated from the blood culture of a patient who was already on antifungals for ''C. albicans'' [[candidemia]].<ref name="pmid21715586" /> | * ''C. auris'' has been isolated from the [[blood culture]] of a patient who was already on [[antifungals]] for ''[[Candida albicans|C. albicans]]'' [[candidemia]].<ref name="pmid21715586" /> | ||
* ''C. auris'' optimally grows at 37–40°C and remains viable till 42°C, exhibiting the thermotolerance necessary to infect humans.<ref name="pmid19161556" /> | * ''C. auris'' optimally grows at 37–40°C and remains viable till 42°C, exhibiting the thermotolerance necessary to infect humans.<ref name="pmid19161556" /> | ||
* Clinical information from three continents revealed a median time of 19 days from admission to ''C. auris'' infection.<ref name=CID>Clinical Infectious Diseases.http://cid.oxfordjournals.org/content/early/2016/10/20/cid.ciw691.abstract. Accessed on November 22nd, 2016.</ref> | * Clinical information from three continents revealed a [[median]] time of 19 days from admission to ''C. auris'' infection.<ref name=CID>Clinical Infectious Diseases.http://cid.oxfordjournals.org/content/early/2016/10/20/cid.ciw691.abstract. Accessed on November 22nd, 2016.</ref> | ||
* The exact mode of transmission is unknown.<ref name="cdc1" /><ref name="cdc2" /> | * The exact mode of transmission is unknown.<ref name="cdc1" /><ref name="cdc2" /> | ||
=== Genetics === | === Genetics === | ||
* ''C. auris'' has a complex genome.<ref name="pmidPMID 26548511" /> | * ''C. auris'' has a complex [[genome]].<ref name="pmidPMID 26548511" /> | ||
* It is phylogenetically closely related to ''C. haemulonii.''<ref name="pmidPMID 26548511" /> | * It is [[Phylogenetics|phylogenetically]] closely related to ''[[Candida|C. haemulonii]].''<ref name="pmidPMID 26548511" /> | ||
* Analysis of selected isolates from the affected hospital in the UK using Amplified Fragment Length Polymorphism(AFLP) suggested distinct clustering of the London isolates when compared to other global isolates. The AFLP | * Analysis of selected isolates from the affected hospital in the UK using [[Amplified fragment length polymorphism|Amplified Fragment Length Polymorphism]] ([[AFLP]]) suggested distinct clustering of the London isolates when compared to other global isolates. The [[Amplified fragment length polymorphism|AFLP]] dendrogram is suggestive of the introduction of a single infecting [[genotype]] into the hospital. There is still ongoing analysis of [[Genome sequence|whole-genome sequences]] to confirm this preliminary observation.<ref name="pmidPMID 27777756" /> | ||
* Detailed information regarding genotypes/clonal strains endemic to specific geographical locations is lacking.<ref name="pmidPMID 26548511" /> | * Detailed information regarding [[Genotype|genotypes]]/clonal strains [[endemic]] to specific geographical locations is lacking.<ref name="pmidPMID 26548511" /> | ||
=== Microscopic Pathology === | === Microscopic Pathology === | ||
* ''C. auris'' cannot be distinguished from most other ''[[Candida]]'' species on microscopy.<ref name="cdc2" /> | * ''C. auris'' cannot be distinguished from most other ''[[Candida]]'' species on microscopy.<ref name="cdc2" /> | ||
* It is a germ tube test negative budding yeast.<ref name="cdc2" /> | * It is a [[Germ tube|germ tube test]] negative [[Yeast|budding yeast]].<ref name="cdc2" /> | ||
* It has a pale purple/pink color on chromogenic agar.<ref name="cdc2" /> | * It has a pale purple/pink color on [[Agar|chromogenic agar]].<ref name="cdc2" /> | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
===Incidence=== | ===Incidence=== | ||
* Higher incidence in public sector hospitals in India when compared to the private sector hospitals.<ref name="pmid25510301">{{cite journal| author=Chakrabarti A, Sood P, Rudramurthy SM, Chen S, Kaur H, Capoor M et al.| title=Incidence, characteristics and outcome of ICU-acquired candidemia in India. | journal=Intensive Care Med | year= 2015 | volume= 41 | issue= 2 | pages= 285-95 | pmid=25510301 | doi=10.1007/s00134-014-3603-2 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25510301 }} </ref> | * Higher [[incidence]] in public sector hospitals in India when compared to the private sector hospitals.<ref name="pmid25510301">{{cite journal| author=Chakrabarti A, Sood P, Rudramurthy SM, Chen S, Kaur H, Capoor M et al.| title=Incidence, characteristics and outcome of ICU-acquired candidemia in India. | journal=Intensive Care Med | year= 2015 | volume= 41 | issue= 2 | pages= 285-95 | pmid=25510301 | doi=10.1007/s00134-014-3603-2 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25510301 }} </ref> | ||
* Thirteen reported cases in the US,<ref name="cdc3">Center for Disease Control. https://www.cdc.gov/media/releases/2016/p1104-candida-auris.html Accessed on November 18th, 2016</ref> the first seven cases occurred between May 2013-August 2016.<ref name="pmidPMID 27832049" /> | * Thirteen reported cases in the US,<ref name="cdc3">Center for Disease Control. https://www.cdc.gov/media/releases/2016/p1104-candida-auris.html Accessed on November 18th, 2016</ref> the first seven cases occurred between May 2013 - August 2016.<ref name="pmidPMID 27832049" /> | ||
* Over fifty cases in the UK between April 2015-July 2016.<ref name="pmidPMID 27777756" /> | * Over fifty cases in the UK between April 2015 - July 2016.<ref name="pmidPMID 27777756" /> | ||
''First outbreak of C. auris in the UK'' | ''First outbreak of C. auris in the UK'' | ||
{| class="wikitable" | {| class="wikitable" | ||
!Number of C. auris | !Number of C. auris | ||
cases/month | cases / month | ||
!Month/Year | !Month/Year | ||
|- | |- | ||
| Line 101: | Line 99: | ||
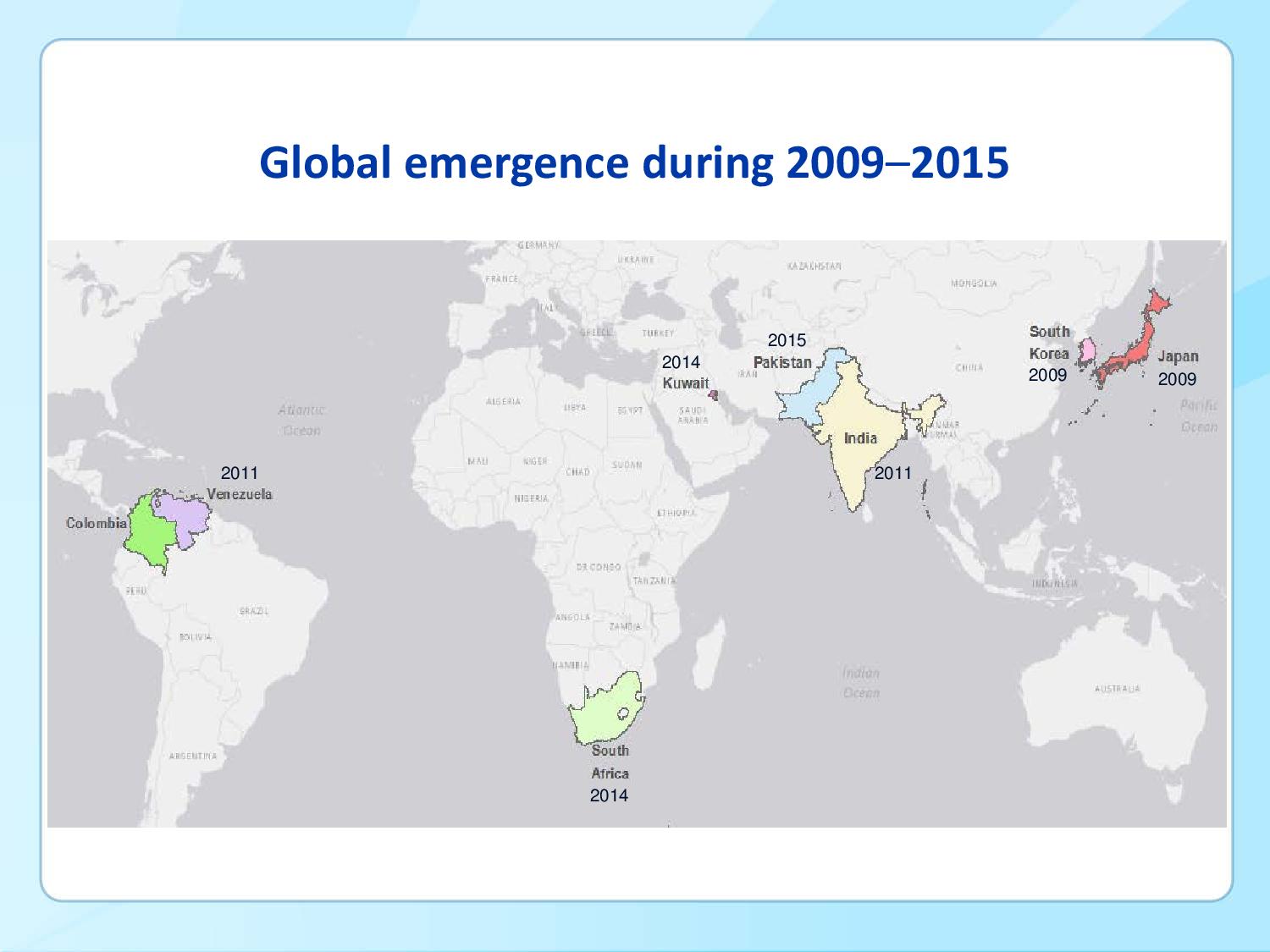
===Geographical Distribution=== | ===Geographical Distribution=== | ||
''Countries with documented isolation of'' ''C. auris'': | ''Countries with documented isolation of'' ''C. auris'' : | ||
# Japan<ref name="pmid19161556"></ref> | # Japan<ref name="pmid19161556"></ref> | ||
# South Korea<ref name="pmid21715586"></ref> | # South Korea<ref name="pmid21715586"></ref> | ||
| Line 114: | Line 112: | ||
# Israel<ref name="pmidPMID 27832049"></ref> | # Israel<ref name="pmidPMID 27832049"></ref> | ||
# Kenya<ref name="pmidPMID 27832049"></ref> | # Kenya<ref name="pmidPMID 27832049"></ref> | ||
[[File:Global emergence of C. auris between 2009-2015.jpeg|700px| | [[File:Global emergence of C. auris between 2009-2015.jpeg|700px|left|thumb|Emergence of C. auris during 2009-2015. Source: World Health Organization]] | ||
<br style="clear:left" /> | |||
=== Geographical Distribution in the US === | === Geographical Distribution in the US === | ||
* ''First seven reported cases in the US (May 2013-August 2016) .''<ref name="pmidPMID 27832049" /> | * ''First seven reported cases in the US (May 2013 - August 2016) .''<ref name="pmidPMID 27832049" /> | ||
{| class="wikitable" | {| class="wikitable" | ||
!Isolation month/year | !Isolation month/year | ||
| Line 127: | Line 126: | ||
|New York | |New York | ||
|Blood | |Blood | ||
|Respiratory failure requiring high-dose corticosteroids | |[[Respiratory failure]] requiring high-dose [[corticosteroids]] | ||
|- | |- | ||
|July 2015 | |July 2015 | ||
|New Jersey | |New Jersey | ||
|Blood | |Blood | ||
|Brain tumor and recent villous adenoma resection | |[[Brain tumor]] and recent [[villous adenoma]] resection | ||
|- | |- | ||
|April 2016 | |April 2016 | ||
|Maryland | |Maryland | ||
|Blood | |Blood | ||
|Hematologic malignancy and bone marrow transplant | |[[Hematological malignancy|Hematologic malignancy]] and [[bone marrow transplant]] | ||
|- | |- | ||
|April 2016 | |April 2016 | ||
|New York | |New York | ||
|Blood | |Blood | ||
|Hematologic malignancy | |[[Leukemia|Hematologic malignancy]] | ||
|- | |- | ||
|May 2016 | |May 2016 | ||
|Illinois | |Illinois | ||
|Blood | |Blood | ||
|Short gut syndrome requiring total parenteral nutrition and high-dose corticosteroid use | |[[Short gut syndrome]] requiring [[total parenteral nutrition]] and high-dose [[corticosteroid]] use | ||
|- | |- | ||
|July 2016 | |July 2016 | ||
|Illinois | |Illinois | ||
|Urine | |Urine | ||
|Paraplegia with long-term, indwelling Foley catheter | |[[Paraplegia]] with long-term, indwelling [[Foley catheter]] | ||
|- | |- | ||
|August 2016 | |August 2016 | ||
|New York | |New York | ||
|Ear | |Ear | ||
|Severe peripheral vascular disease and skull base osteomyelitis | |Severe [[peripheral vascular disease]] and [[osteomyelitis|skull base osteomyelitis]] | ||
|} | |} | ||
==Risk Factors== | ==Risk Factors== | ||
* Stay in the Intensive Care Unit is a major risk factor for ''C. auris'' infection.<ref name="pmidPMID 27777756" /><ref name="pmidPMID 26548511" /> | * Stay in the [[Intensive care unit|Intensive Care Unit]] is a major risk factor for ''C. auris'' infection.<ref name="pmidPMID 27777756" /><ref name="pmidPMID 26548511" /> | ||
* Patients who had a prolonged hospital stay.<ref name="cdc1" /> | * Patients who had a prolonged hospital stay.<ref name="cdc1" /> | ||
* Multiple invasive medical procedures.<ref name="pmidPMID 27452195" /> | * Multiple invasive medical procedures.<ref name="pmidPMID 27452195" /> | ||
* Similar risk factors for infections with other ''[[Candida]]'' spp including diabetes mellitus, recent surgery, recent antibiotics, presence of central venous catheters.<ref name="cdc1" /> | * Similar risk factors for infections with other ''[[Candida]]'' spp including [[diabetes mellitus]], recent surgery, recent [[antibiotics]], presence of [[central venous catheters]].<ref name="cdc1" /> | ||
* Serious underlying medical conditions such as hematologic malignancies, respiratory failure requiring high dose steroids, short gut syndrome requiring total parenteral nutrition, paraplegia with a chronic urinary catheter, etc.<ref name="pmidPMID 27832049" /> | * Serious underlying medical conditions such as [[Hematological malignancies|hematologic malignancies]], [[respiratory failure]] requiring high dose [[steroids]], [[short gut syndrome]] requiring [[total parenteral nutrition]], [[paraplegia]] with a chronic [[urinary catheter]], etc.<ref name="pmidPMID 27832049" /> | ||
* Co-infection with other ''[[Candida]]'' spp.<ref name="pmid21715586" /><ref name="cdc1" /> | * Co-infection with other ''[[Candida]]'' spp.<ref name="pmid21715586" /><ref name="cdc1" /> | ||
| Line 176: | Line 175: | ||
* Persistent colonization of patients reported from affected hospitals around the world.<ref name="cdc2" /> | * Persistent colonization of patients reported from affected hospitals around the world.<ref name="cdc2" /> | ||
* Colonization with ''C. auris'' is difficult to eradicate.<ref name="cdc2" /> | * Colonization with ''C. auris'' is difficult to eradicate.<ref name="cdc2" /> | ||
* Recurrence of ''C. auris'' candidemia three to four months after an initial episode has been reported in at least two patients.<ref name="pmidPMID 27832049" /> | * Recurrence of ''C. auris'' [[candidemia]] three to four months after an initial episode has been reported in at least two patients.<ref name="pmidPMID 27832049" /> | ||
=== Complications === | === Complications === | ||
* Invasive wound infections<ref name="pmidPMID 27832049" /> | * Invasive wound infections<ref name="pmidPMID 27832049" /> | ||
* Otitis media<ref name="cdc1" /> | * [[Otitis media]]<ref name="cdc1" /> | ||
* Candidemia with high mortality<ref name="pmidPMID 27832049" /><ref name="pmidPMID 27777756" /> | * [[Candidemia]] with high [[mortality]]<ref name="pmidPMID 27832049" /><ref name="pmidPMID 27777756" /> | ||
* Septic shock<ref name="pmid21715586" /> | * [[Septic shock]]<ref name="pmid21715586" /> | ||
=== Prognosis === | === Prognosis === | ||
* [[Candidemia]] attributed to ''C auris'' is associated with mortality of up to 50 % in some countries.<ref name="pmidPMID 27777756" /> | * [[Candidemia]] attributed to ''C auris'' is associated with [[mortality]] of up to 50 % in some countries.<ref name="pmidPMID 27777756" /> | ||
==Diagnosis== | ==Diagnosis== | ||
| Line 191: | Line 190: | ||
=== History and Symptoms === | === History and Symptoms === | ||
====History==== | ====History==== | ||
Patients with ''Candida auris'' infection often present with underlying | Patients with ''Candida auris'' infection often present with underlying risk factors, such as: | ||
* An underlying serious medical condition.<ref name="pmidPMID 27832049" /> | * An underlying serious medical condition.<ref name="pmidPMID 27832049" /> | ||
* A history of a prolonged hospital stay.<ref name="cdc1" /> | * A history of a prolonged hospital stay.<ref name="cdc1" /> | ||
| Line 197: | Line 196: | ||
====Symptoms==== | ====Symptoms==== | ||
''C. auris'' infection can present like ''Candida'' infection caused by other ''Candida'' species. However, unlike the other Candida species, ''C. auris'' has been noted to persistently colonize the healthcare environment.<ref name="pmidPMID 27777756" /> Presenting symptoms depend on the affected part of the body and can include the following: | ''C. auris'' infection can present like ''[[Candidiasis|Candida]]'' [[Candidiasis|infection]] caused by other ''[[Candida]]'' [[Candida|species]]. However, unlike the other [[Candida|Candida species]], ''C. auris'' has been noted to persistently colonize the healthcare environment.<ref name="pmidPMID 27777756" /> Presenting symptoms depend on the affected part of the body and can include the following: | ||
* Ear discharge<ref name="pmid19161556" /> | * [[Ear discharge]]<ref name="pmid19161556" /> | ||
* Vaginal discharge<ref name="pmid25881537">{{cite journal| author=Kumar D, Banerjee T, Pratap CB, Tilak R| title=Itraconazole-resistant Candida auris with phospholipase, proteinase and hemolysin activity from a case of vulvovaginitis. | journal=J Infect Dev Ctries | year= 2015 | volume= 9 | issue= 4 | pages= 435-7 | pmid=25881537 | doi=10.3855/jidc.4582 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25881537 }} </ref> | * [[Vaginal discharge]]<ref name="pmid25881537">{{cite journal| author=Kumar D, Banerjee T, Pratap CB, Tilak R| title=Itraconazole-resistant Candida auris with phospholipase, proteinase and hemolysin activity from a case of vulvovaginitis. | journal=J Infect Dev Ctries | year= 2015 | volume= 9 | issue= 4 | pages= 435-7 | pmid=25881537 | doi=10.3855/jidc.4582 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25881537 }} </ref> | ||
* Vaginal itching<ref name="pmid25881537">{{cite journal| author=Kumar D, Banerjee T, Pratap CB, Tilak R| title=Itraconazole-resistant Candida auris with phospholipase, proteinase and hemolysin activity from a case of vulvovaginitis. | journal=J Infect Dev Ctries | year= 2015 | volume= 9 | issue= 4 | pages= 435-7 | pmid=25881537 | doi=10.3855/jidc.4582 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25881537 }} </ref> | * Vaginal itching<ref name="pmid25881537">{{cite journal| author=Kumar D, Banerjee T, Pratap CB, Tilak R| title=Itraconazole-resistant Candida auris with phospholipase, proteinase and hemolysin activity from a case of vulvovaginitis. | journal=J Infect Dev Ctries | year= 2015 | volume= 9 | issue= 4 | pages= 435-7 | pmid=25881537 | doi=10.3855/jidc.4582 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25881537 }} </ref> | ||
Symptoms of ''Candida auris'' blood infection can include: | Symptoms of ''Candida auris'' blood infection can include: | ||
* Fever<ref name="pmid21715586" /> | * [[Fever]]<ref name="pmid21715586" /> | ||
* [[ | * [[Septic shock]]<ref name="pmid21715586" /> | ||
* [[Multiorgan failure]] | * [[Multiorgan failure]]<ref name="pmid21715586" /> | ||
=== Physical Examination === | === Physical Examination === | ||
| Line 211: | Line 210: | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
'''Microscopy''' | '''Microscopy''' | ||
* ''C. auris'' is indistinguishable from most other ''[[Candida]]'' species.<ref name="cdc2" /> | * ''C. auris'' is indistinguishable from most other ''[[Candida]]'' [[Candida|species]].<ref name="cdc2" /> | ||
* It is a germ tube test negative budding yeast, however some strains can form rudimentary pseudohyphae on cornmeal agar. | * It is a [[germ tube]] test negative budding [[yeast]], however some [[strains]] can form rudimentary pseudohyphae on [[Agar|cornmeal agar]]. | ||
* Most ''C. auris'' isolates are a pale purple or pink colour on the chromogenic agar; CHROMagar Candida, in common with several other non-C. albicans species. Growth on this and other chromogenic agars (which may display a different colour) cannot be used as a primary identification method. | * Most ''C. auris'' isolates are a pale purple or pink colour on the [[Agar|chromogenic agar]]; CHROMagar Candida, in common with several other non-C. albicans species. Growth on this and other [[Agar|chromogenic agars]] (which may display a different colour) cannot be used as a primary identification method. | ||
* Chromogenic agars are useful to identify mixed cultures including the presence of ''[[C. albicans]]''. | * [[Agar|Chromogenic agars]] are useful to identify mixed cultures including the presence of ''[[C. albicans]]''. | ||
* When there is evidence of non-C. albicans on chromogenic agar, these should be sub-cultured on Sabouraud’s agar and identified according to local laboratory protocols.<ref name="cdc2" /> | * When there is evidence of non-C. albicans on [[Agar|chromogenic agar]], these should be sub-cultured on [[Agar|Sabouraud’s agar]] and identified according to local laboratory protocols.<ref name="cdc2" /> | ||
'''Biochemical-based test''' | '''Biochemical-based test''' | ||
* Laboratories are advised to check the databases provided for their current methods. | * Laboratories are advised to check the databases provided for their current methods. | ||
* Currently available biochemical-based tests highly unlikely to include C. auris in their database as it is a newly recognized species. | * Currently available biochemical-based tests highly unlikely to include C. auris in their database as it is a newly recognized [[Species|species.]] | ||
* Commercially available biochemical-based tests, including API AUX 20C and VITEK-2 YST, used in many front line diagnostic laboratories can misidentify ''C. auris'' as ''Candida haemulonii'', ''Saccharomyces cerevisiae, Rhodotorula glutinis''.<ref name="cdc2" /> <ref name="pmidPMID 26548511" /> | * Commercially available biochemical-based tests, including API AUX 20C and VITEK-2 YST, used in many front line diagnostic laboratories can misidentify ''C. auris'' as ''[[Candida|Candida haemulonii]]'', ''[[Saccharomyces cerevisiae]], [[Rhodotorula|Rhodotorula glutinis]]''.<ref name="cdc2" /> <ref name="pmidPMID 26548511" /> | ||
* ''[[Candida]]'' spp associated with invasive infections and isolates from superficial sites in patients from high intensity settings, and those transferred from an affected hospital should be analysed to species level. | * ''[[Candida]]'' spp associated with invasive infections and isolates from superficial sites in patients from high intensity settings, and those transferred from an affected hospital should be analysed to species level. | ||
'''Molecular-based test''' | '''Molecular-based test''' | ||
* If ''Candida haemulonii'', ''Candida famata'', ''Candida sake'' or ''Saccharomyces cerevisiae'' are identified, it is pertinent to ensure that they are not ''C. auris''. This would involve either molecular sequencing of the D1/D2 domain or MALDI-TOF(matrix-assisted laser desorption ionization time-of-flight mass spectrometry) Biotyper analysis with ''C. auris'' either already present or added to the database.<ref name="cdc2" /> | * If ''[[Candida|Candida haemulonii]]'', ''[[Candida|Candida famata]]'', ''[[Candida|Candida sake]]'' or ''[[Saccharomyces cerevisiae]]'' are identified, it is pertinent to ensure that they are not ''C. auris''. This would involve either molecular sequencing of the D1/D2 domain or [[MALDI-TOF]]([[Matrix-assisted laser desorption/ionization|matrix-assisted laser desorption ionization time-of-flight mass spectrometry]]) Biotyper analysis with ''C. auris'' either already present or added to the database.<ref name="cdc2" /> | ||
== Differentiating ''Candida auris'' from other ''[[non-Candida albicans]]'' species == | == Differentiating ''Candida auris'' from other ''[[non-Candida albicans]]'' species == | ||
* | * ''C.auris'' can be differentiated from other non-''Candida albicans'' species via reliable methods for [[speciation]] that are molecular-based such as [[PCR]], [[AFLP]]([[amplified fragment length polymorphism]]) fingerprinting, [[Sequence analysis|sequencing analysis]], and [[Matrix-assisted laser desorption/ionization|MALDI-TOF biotyping]].<ref name="cdc2" /><ref name="pmidPMID 27777756" /> | ||
==Treatment== | ==Treatment== | ||
=== Medical Therapy === | === Medical Therapy === | ||
*'''Early identification''' of ''Candida'' species to ensure appropriate use of antifungal medication and also for prompt implementation of infection control measures.<ref name="pmidPMID 27777756" /> | *'''Early identification''' of ''[[Candida]]'' [[Candida|species]] to ensure appropriate use of [[antifungal medication]] and also for prompt implementation of [[infection control]] measures.<ref name="pmidPMID 27777756" /> | ||
* '''Antifungal susceptibility testing''': Candida auris isolates from north and south Indian hospitals, Japan and Korea were all found to be resistant to the antifungal medication fluconazole.<ref name="pmidPMID 24357342" />Some isolates were also noted to be resistant to antifungal medications such as flucytosine and voriconazole.<ref name="pmidPMID 24357342" />There are no established minimum inhibitory concentration (MIC) breakpoints at present for ''C. auris''. Using breakpoints for other ''Candida'' spp, the Centers for Disease Control and Prevention (CDC) demonstrated that nearly all isolates from the global outbreaks being investigated are highly resistant to fluconazole. In their analysis, more than half of ''C. auris'' isolates were resistant to voriconazole, one- third were resistant to amphotericin B (MIC ≥2 mg/L), and a few were resistant to echinocandins. Some isolates have demonstrated elevated MICs to all three major antifungal classes, including azoles, echinocandins, and polyenes, indicating that treatment options would be limited. Whole genome sequencing of the organism has found resistant determinants to a variety of antifungal agents.<ref name="cdc2" /> | * '''Antifungal susceptibility testing''': Candida auris isolates from north and south Indian hospitals, Japan and Korea were all found to be resistant to the antifungal medication [[fluconazole]].<ref name="pmidPMID 24357342" /> Some isolates were also noted to be resistant to [[Antifungal medication|antifungal medications]] such as [[flucytosine]] and [[voriconazole]].<ref name="pmidPMID 24357342" />There are no established [[Minimum inhibitory concentration|minimum inhibitory concentration (MIC)]] breakpoints at present for ''C. auris''. Using breakpoints for other ''Candida'' spp, the [[Centers for Disease Control and Prevention|Centers for Disease Control and Prevention (CDC)]] demonstrated that nearly all isolates from the global [[outbreaks]] being investigated are highly resistant to [[fluconazole]]. In their analysis, more than half of ''C. auris'' isolates were resistant to [[voriconazole]], one- third were resistant to [[amphotericin B]] ([[MIC]] ≥2 mg/L), and a few were resistant to [[echinocandins]]. Some isolates have demonstrated elevated [[MIC|MICs]] to all three major antifungal classes, including [[azoles]], [[echinocandins]], and [[Polyene antimycotic|polyenes]], indicating that treatment options would be limited. Whole [[genome sequencing]] of the organism has found resistant determinants to a variety of [[Antifungal drug|antifungal agents]].<ref name="cdc2" /> | ||
* '''First-line therapy''' is an echinocandin pending specific susceptibility testing which should be undertaken as soon as possible.<ref name="pmid27634564">{{cite journal| author=Chowdhary A, Voss A, Meis JF| title=Multidrug-resistant Candida auris: 'new kid on the block' in hospital-associated infections? | journal=J Hosp Infect | year= 2016 | volume= 94 | issue= 3 | pages= 209-212 | pmid=27634564 | doi=10.1016/j.jhin.2016.08.004 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27634564 }} </ref>There is evidence that resistance can evolve quite rapidly in this species and ongoing vigilance for evolving resistance is advised in patients found to be infected or colonized with ''C. auris''.<ref name="cdc2" /><ref name="pmid27634564" /> | * '''First-line therapy''' is an [[echinocandin]] pending specific susceptibility testing which should be undertaken as soon as possible.<ref name="pmid27634564">{{cite journal| author=Chowdhary A, Voss A, Meis JF| title=Multidrug-resistant Candida auris: 'new kid on the block' in hospital-associated infections? | journal=J Hosp Infect | year= 2016 | volume= 94 | issue= 3 | pages= 209-212 | pmid=27634564 | doi=10.1016/j.jhin.2016.08.004 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27634564 }} </ref> There is evidence that resistance can evolve quite rapidly in this species and ongoing vigilance for evolving [[Drug resistance|resistance]] is advised in patients found to be infected or colonized with ''C. auris''.<ref name="cdc2" /><ref name="pmid27634564" /> | ||
* '''Combination therapy''': Evidence supporting combination therapy in invasive infections with ''C. auris'' is lacking and clinicians are advised to make decisions on a case by case basis.<ref name="cdc2" /> | * '''Combination therapy''': Evidence supporting combination therapy in invasive infections with ''C. auris'' is lacking and clinicians are advised to make decisions on a case by case basis.<ref name="cdc2" /> | ||
=== '''Primary Prevention''' === | === '''Primary Prevention''' === | ||
* Isolation of colonized or infected patients with en suite facilities wherever possible.<ref name="cdc2" /> | * Isolation of colonized or infected patients with en suite facilities wherever possible.<ref name="cdc2" /> | ||
* Adherence to strict | * Adherence to strict infection prevention and control precautions, including hand hygiene using soap and water followed by alcohol hand rub, use of personal protective equipment in the form of gloves and aprons (or gowns if there is a high risk of soiling with blood or body fluids).<ref name="cdc2" /> | ||
* A chlorine releasing agent is currently recommended for cleaning of the environment at 1000 ppm of available chlorine.<ref name="cdc2" /> | * A [[chlorine]] releasing agent is currently recommended for cleaning of the environment at 1000 ppm of available [[chlorine]].<ref name="cdc2" /> | ||
* A terminal clean should be undertaken once the patient has left the environment preferably using hydrogen peroxide vapour. All equipment should be cleaned in accordance with manufacturer’s instructions and where relevant, returned to the company for cleaning. Particular attention should be paid to cleaning of multiple-use equipment (such as BP cuffs, thermometers, computers on wheels, | * A terminal clean should be undertaken once the patient has left the environment preferably using [[hydrogen peroxide]] vapour. All equipment should be cleaned in accordance with manufacturer’s instructions and where relevant, returned to the company for cleaning. Particular attention should be paid to cleaning of multiple-use equipment (such as BP cuffs, thermometers, computers on wheels, ultrasound machines) from the bed spaces of infected/colonized patient.<ref name="cdc2"/> | ||
== References == | == References == | ||
{{reflist|2}} | {{reflist|2}} | ||
Latest revision as of 19:38, 15 August 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Fatimo Biobaku M.B.B.S [2]
Overview
Candida auris is a fungus, recently described as a rare cause of fungal infection with significant resistance to antifungal medications.[1] It was first described in the year 2009 in Japan,[2] and since then, reports of C. auris infection has been published from several countries.[2] However, retrospective testing of collected isolates show the earliest known infection with C. auris occurred in South Korea in 1996.[3][4] Serious and prolonged outbreaks have been documented with data showing an innate resilience of C. auris for survival, persistence in the clinical environment with the ability to rapidly colonize the skin of patients, and high transmissibility within the healthcare system.[5] The first reported case in Europe involved over fifty cases in a span of more than sixteen months in a cardiothoracic center in London, and it is the largest outbreak in Europe.[5] The precise mode of transmission within the healthcare facility is unknown.[6][3] The high rate of therapeutic failure noted in cases of Candida auris fungemia poses significant concerns.[1] Misidentification of C. auris with related Candida species such as Candida haemulonii by commercially available biochemical-based tests poses a challenge.[6] C. auris is recognized as a globally emerging fungal pathogen and it requires reproducible laboratory methods for identification and typing.[7][5] Institution of key infection prevention and control measures,[3] correct identification and standardized antifungal susceptibility testing for optimal management strategies of patients with invasive infections can hardly be overemphasized.[3]
Historical Perspective
- C. auris was first described in 2009 after being isolated from the external ear canal discharge of a patient in Japan.[2]
- The first report of blood stream infection by C. auris was in 2011 from Korea.[8]
- C. auris was incidentally found by molecular identification of bloodstream isolates of unidentified yeasts recovered in 1996, suggesting the paucity of isolation of C. auris may partly reflect the difficulty in identifying the species.[4]
- The occurrence of C. auris in at least nine countries on four continents since 2009 has been reported.[6]
- C. auris infections have most commonly been hospital-acquired and occurred several weeks into a patient’s hospital stay.[6]
- It has been documented to cause infection in patients of all ages.[6][4][9]
Causes
Candida auris infection is caused by C. auris; an ascomycetous yeast species belonging to the genus Candida, and it has a high potential for nosocomial horizontal transmission.[5][10][11]
Pathophysiology
Pathogenesis
- C. auris cases have been identified from clinical sites such as wound swabs, urine samples, vascular devices tips, blood cultures as well as skin screening samples (including nose, oropharynx, axilla, groin and stool samples).[5]
- C. auris has been reported to cause bloodstream infections, wound infections, and otitis media.[6][4]
- The occurrence of candidemia attributed to C. auris appears increasingly common.[5]
- Evidence of distinct geographic clustering of Candida auris isolates has been established.[7]
- C. auris has been isolated from the blood culture of a patient who was already on antifungals for C. albicans candidemia.[4]
- C. auris optimally grows at 37–40°C and remains viable till 42°C, exhibiting the thermotolerance necessary to infect humans.[11]
- Clinical information from three continents revealed a median time of 19 days from admission to C. auris infection.[12]
- The exact mode of transmission is unknown.[6][3]
Genetics
- C. auris has a complex genome.[7]
- It is phylogenetically closely related to C. haemulonii.[7]
- Analysis of selected isolates from the affected hospital in the UK using Amplified Fragment Length Polymorphism (AFLP) suggested distinct clustering of the London isolates when compared to other global isolates. The AFLP dendrogram is suggestive of the introduction of a single infecting genotype into the hospital. There is still ongoing analysis of whole-genome sequences to confirm this preliminary observation.[5]
- Detailed information regarding genotypes/clonal strains endemic to specific geographical locations is lacking.[7]
Microscopic Pathology
- C. auris cannot be distinguished from most other Candida species on microscopy.[3]
- It is a germ tube test negative budding yeast.[3]
- It has a pale purple/pink color on chromogenic agar.[3]
Epidemiology and Demographics
Incidence
- Higher incidence in public sector hospitals in India when compared to the private sector hospitals.[13]
- Thirteen reported cases in the US,[14] the first seven cases occurred between May 2013 - August 2016.[2]
- Over fifty cases in the UK between April 2015 - July 2016.[5]
First outbreak of C. auris in the UK
| Number of C. auris
cases / month |
Month/Year |
|---|---|
| 2 | April/2015 |
| 2 | June/2015 |
| 3 | October/2015 |
| 2 | November/2015 |
| 1 | December/2015 |
| 7 | June/2016 |
| 5 | February/2016 |
| 10 | March/2016 |
| 8 | April/2016 |
| 4 | May 2016 |
| 3 | June/2016 |
| 4 | July/2016 |
Age
Gender
- No known gender predilection.
Race
- No known racial predilection.
Geographical Distribution
Countries with documented isolation of C. auris :
- Japan[11]
- South Korea[4]
- India[2]
- Kuwait[9]
- South Africa[2]
- Venezuela[10]
- USA[2]
- UK[5]
- Colombia[2]
- Pakistan[2]
- Israel[2]
- Kenya[2]
Geographical Distribution in the US
- First seven reported cases in the US (May 2013 - August 2016) .[2]
| Isolation month/year | State | Site of C.auris isolation | Underlying medical condition(s) |
|---|---|---|---|
| May 2013 | New York | Blood | Respiratory failure requiring high-dose corticosteroids |
| July 2015 | New Jersey | Blood | Brain tumor and recent villous adenoma resection |
| April 2016 | Maryland | Blood | Hematologic malignancy and bone marrow transplant |
| April 2016 | New York | Blood | Hematologic malignancy |
| May 2016 | Illinois | Blood | Short gut syndrome requiring total parenteral nutrition and high-dose corticosteroid use |
| July 2016 | Illinois | Urine | Paraplegia with long-term, indwelling Foley catheter |
| August 2016 | New York | Ear | Severe peripheral vascular disease and skull base osteomyelitis |
Risk Factors
- Stay in the Intensive Care Unit is a major risk factor for C. auris infection.[5][7]
- Patients who had a prolonged hospital stay.[6]
- Multiple invasive medical procedures.[10]
- Similar risk factors for infections with other Candida spp including diabetes mellitus, recent surgery, recent antibiotics, presence of central venous catheters.[6]
- Serious underlying medical conditions such as hematologic malignancies, respiratory failure requiring high dose steroids, short gut syndrome requiring total parenteral nutrition, paraplegia with a chronic urinary catheter, etc.[2]
- Co-infection with other Candida spp.[4][6]
Screening
Screening is advised for patients coming from other affected hospitals / units in the UK and abroad.[6]
Natural History, Complications, and Prognosis
Natural History
- Persistent colonization of patients reported from affected hospitals around the world.[3]
- Colonization with C. auris is difficult to eradicate.[3]
- Recurrence of C. auris candidemia three to four months after an initial episode has been reported in at least two patients.[2]
Complications
- Invasive wound infections[2]
- Otitis media[6]
- Candidemia with high mortality[2][5]
- Septic shock[4]
Prognosis
- Candidemia attributed to C auris is associated with mortality of up to 50 % in some countries.[5]
Diagnosis
History and Symptoms
History
Patients with Candida auris infection often present with underlying risk factors, such as:
- An underlying serious medical condition.[2]
- A history of a prolonged hospital stay.[6]
- A history of admission into the ICU.[5]
Symptoms
C. auris infection can present like Candida infection caused by other Candida species. However, unlike the other Candida species, C. auris has been noted to persistently colonize the healthcare environment.[5] Presenting symptoms depend on the affected part of the body and can include the following:
- Ear discharge[11]
- Vaginal discharge[15]
- Vaginal itching[15]
Symptoms of Candida auris blood infection can include:
Physical Examination
The physical examination findings in C. auris infection is not well documented.
Laboratory Findings
Microscopy
- C. auris is indistinguishable from most other Candida species.[3]
- It is a germ tube test negative budding yeast, however some strains can form rudimentary pseudohyphae on cornmeal agar.
- Most C. auris isolates are a pale purple or pink colour on the chromogenic agar; CHROMagar Candida, in common with several other non-C. albicans species. Growth on this and other chromogenic agars (which may display a different colour) cannot be used as a primary identification method.
- Chromogenic agars are useful to identify mixed cultures including the presence of C. albicans.
- When there is evidence of non-C. albicans on chromogenic agar, these should be sub-cultured on Sabouraud’s agar and identified according to local laboratory protocols.[3]
Biochemical-based test
- Laboratories are advised to check the databases provided for their current methods.
- Currently available biochemical-based tests highly unlikely to include C. auris in their database as it is a newly recognized species.
- Commercially available biochemical-based tests, including API AUX 20C and VITEK-2 YST, used in many front line diagnostic laboratories can misidentify C. auris as Candida haemulonii, Saccharomyces cerevisiae, Rhodotorula glutinis.[3] [7]
- Candida spp associated with invasive infections and isolates from superficial sites in patients from high intensity settings, and those transferred from an affected hospital should be analysed to species level.
Molecular-based test
- If Candida haemulonii, Candida famata, Candida sake or Saccharomyces cerevisiae are identified, it is pertinent to ensure that they are not C. auris. This would involve either molecular sequencing of the D1/D2 domain or MALDI-TOF(matrix-assisted laser desorption ionization time-of-flight mass spectrometry) Biotyper analysis with C. auris either already present or added to the database.[3]
Differentiating Candida auris from other non-Candida albicans species
- C.auris can be differentiated from other non-Candida albicans species via reliable methods for speciation that are molecular-based such as PCR, AFLP(amplified fragment length polymorphism) fingerprinting, sequencing analysis, and MALDI-TOF biotyping.[3][5]
Treatment
Medical Therapy
- Early identification of Candida species to ensure appropriate use of antifungal medication and also for prompt implementation of infection control measures.[5]
- Antifungal susceptibility testing: Candida auris isolates from north and south Indian hospitals, Japan and Korea were all found to be resistant to the antifungal medication fluconazole.[1] Some isolates were also noted to be resistant to antifungal medications such as flucytosine and voriconazole.[1]There are no established minimum inhibitory concentration (MIC) breakpoints at present for C. auris. Using breakpoints for other Candida spp, the Centers for Disease Control and Prevention (CDC) demonstrated that nearly all isolates from the global outbreaks being investigated are highly resistant to fluconazole. In their analysis, more than half of C. auris isolates were resistant to voriconazole, one- third were resistant to amphotericin B (MIC ≥2 mg/L), and a few were resistant to echinocandins. Some isolates have demonstrated elevated MICs to all three major antifungal classes, including azoles, echinocandins, and polyenes, indicating that treatment options would be limited. Whole genome sequencing of the organism has found resistant determinants to a variety of antifungal agents.[3]
- First-line therapy is an echinocandin pending specific susceptibility testing which should be undertaken as soon as possible.[8] There is evidence that resistance can evolve quite rapidly in this species and ongoing vigilance for evolving resistance is advised in patients found to be infected or colonized with C. auris.[3][8]
- Combination therapy: Evidence supporting combination therapy in invasive infections with C. auris is lacking and clinicians are advised to make decisions on a case by case basis.[3]
Primary Prevention
- Isolation of colonized or infected patients with en suite facilities wherever possible.[3]
- Adherence to strict infection prevention and control precautions, including hand hygiene using soap and water followed by alcohol hand rub, use of personal protective equipment in the form of gloves and aprons (or gowns if there is a high risk of soiling with blood or body fluids).[3]
- A chlorine releasing agent is currently recommended for cleaning of the environment at 1000 ppm of available chlorine.[3]
- A terminal clean should be undertaken once the patient has left the environment preferably using hydrogen peroxide vapour. All equipment should be cleaned in accordance with manufacturer’s instructions and where relevant, returned to the company for cleaning. Particular attention should be paid to cleaning of multiple-use equipment (such as BP cuffs, thermometers, computers on wheels, ultrasound machines) from the bed spaces of infected/colonized patient.[3]
References
- ↑ 1.0 1.1 1.2 1.3 Chowdhary A, Anil Kumar V, Sharma C, Prakash A, Agarwal K, Babu R; et al. (2014). "Multidrug-resistant endemic clonal strain of Candida auris in India". Eur J Clin Microbiol Infect Dis. 33 (6): 919–26. doi:10.1007/s10096-013-2027-1. PMID 24357342 PMID 24357342 Check
|pmid=value (help). - ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 Vallabhaneni S, Kallen A, Tsay S, Chow N, Welsh R, Kerins J; et al. (2016). "Investigation of the First Seven Reported Cases of Candida auris, a Globally Emerging Invasive, Multidrug-Resistant Fungus - United States, May 2013-August 2016". MMWR Morb Mortal Wkly Rep. 65 (44): 1234–1237. doi:10.15585/mmwr.mm6544e1. PMID 27832049 PMID 27832049 Check
|pmid=value (help). - ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 Public Health England.https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/534174/Guidance_Candida__auris.pdf. Accessed on November 11th, 2016.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 Lee WG, Shin JH, Uh Y, Kang MG, Kim SH, Park KH; et al. (2011). "First three reported cases of nosocomial fungemia caused by Candida auris". J Clin Microbiol. 49 (9): 3139–42. doi:10.1128/JCM.00319-11. PMC 3165631. PMID 21715586.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 Schelenz S, Hagen F, Rhodes JL, Abdolrasouli A, Chowdhary A, Hall A; et al. (2016). "First hospital outbreak of the globally emerging Candida auris in a European hospital". Antimicrob Resist Infect Control. 5: 35. doi:10.1186/s13756-016-0132-5. PMC 5069812. PMID 27777756 PMID 27777756 Check
|pmid=value (help). - ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 Centers for Disease Control and Prevention. https://www.cdc.gov/fungal/diseases/candidiasis/candida-auris-alert.html Accessed on November 11th, 2016.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Prakash A, Sharma C, Singh A, Kumar Singh P, Kumar A, Hagen F; et al. (2016). "Evidence of genotypic diversity among Candida auris isolates by multilocus sequence typing, matrix-assisted laser desorption ionization time-of-flight mass spectrometry and amplified fragment length polymorphism". Clin Microbiol Infect. 22 (3): 277.e1–9. doi:10.1016/j.cmi.2015.10.022. PMID 26548511 PMID 26548511 Check
|pmid=value (help). - ↑ 8.0 8.1 8.2 Chowdhary A, Voss A, Meis JF (2016). "Multidrug-resistant Candida auris: 'new kid on the block' in hospital-associated infections?". J Hosp Infect. 94 (3): 209–212. doi:10.1016/j.jhin.2016.08.004. PMID 27634564.
- ↑ 9.0 9.1 9.2 Emara M, Ahmad S, Khan Z, Joseph L, Al-Obaid I, Purohit P; et al. (2015). "Candida auris candidemia in Kuwait, 2014". Emerg Infect Dis. 21 (6): 1091–2. doi:10.3201/eid2106.150270. PMC 4451886. PMID 25989098 PMID 25989098 Check
|pmid=value (help). - ↑ 10.0 10.1 10.2 Calvo B, Melo AS, Perozo-Mena A, Hernandez M, Francisco EC, Hagen F; et al. (2016). "First report of Candida auris in America: Clinical and microbiological aspects of 18 episodes of candidemia". J Infect. 73 (4): 369–74. doi:10.1016/j.jinf.2016.07.008. PMID 27452195 PMID 27452195 Check
|pmid=value (help). - ↑ 11.0 11.1 11.2 11.3 Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H (2009). "Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital". Microbiol Immunol. 53 (1): 41–4. doi:10.1111/j.1348-0421.2008.00083.x. PMID 19161556.
- ↑ Clinical Infectious Diseases.http://cid.oxfordjournals.org/content/early/2016/10/20/cid.ciw691.abstract. Accessed on November 22nd, 2016.
- ↑ Chakrabarti A, Sood P, Rudramurthy SM, Chen S, Kaur H, Capoor M; et al. (2015). "Incidence, characteristics and outcome of ICU-acquired candidemia in India". Intensive Care Med. 41 (2): 285–95. doi:10.1007/s00134-014-3603-2. PMID 25510301.
- ↑ Center for Disease Control. https://www.cdc.gov/media/releases/2016/p1104-candida-auris.html Accessed on November 18th, 2016
- ↑ 15.0 15.1 Kumar D, Banerjee T, Pratap CB, Tilak R (2015). "Itraconazole-resistant Candida auris with phospholipase, proteinase and hemolysin activity from a case of vulvovaginitis". J Infect Dev Ctries. 9 (4): 435–7. doi:10.3855/jidc.4582. PMID 25881537.