WBR0735
| Author | [[PageAuthor::Yazan Daaboul, M.D. (Reviewed by Yazan Daaboul, M.D.)]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Pharmacology, MainCategory::Physiology |
| Sub Category | SubCategory::Vascular |
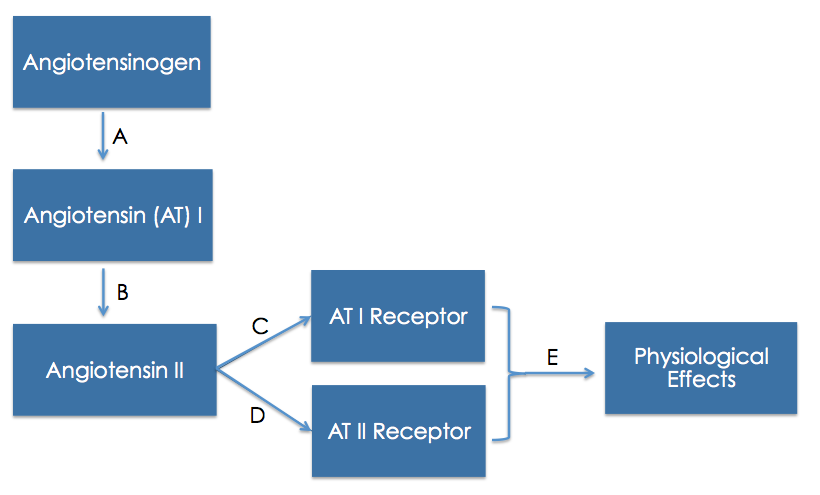
| Prompt | [[Prompt::A 52-year-old man presents to the physician's office complaining of headache and blurry vision. His past medical history is only significant for dyslipidemia. He states that he often uses an electronic sphygmomanometer while resting at home. His blood pressure was elevated on several previous occasions in the past, but he has not been receiving any anti-hypertensive medication. In the clinic, the patient's blood pressure is 158/92 mmHg, heart rate is 72/min, and temperature is 36.8 °C (98.24 °F). The physician decides to start the patient on a medication that also inhibits the breakdown of bradykinin. Based on the diagram below, at which level of the renin-angiotensin pathway does the prescribed medication act? |
| Answer A | AnswerA::A |
| Answer A Explanation | AnswerAExp::Renin is the enzyme that converts angiotensinogen to angiotensin I. Renin inhibitors act at this level. |
| Answer B | AnswerB::B |
| Answer B Explanation | AnswerBExp::ACE is the enzyme that converts angiotensin I to angiotensin II. ACE-inhibitors act at this level. |
| Answer C | AnswerC::C |
| Answer C Explanation | AnswerCExp::ACE-I does not act at the level of the AT-I receptor. |
| Answer D | AnswerD::D |
| Answer D Explanation | AnswerDExp::Angiotensin II receptor blockers (ARB) act at this level of the pathway. |
| Answer E | AnswerE::E |
| Answer E Explanation | AnswerEExp::ACE-I does not act at this level of the pathway. |
| Right Answer | RightAnswer::B |
| Explanation | [[Explanation::The renin-angiotensin aldosterone system (RAAS) is a major hormonal pathway that plays a significant role in the control of arterial blood pressure, tissue perfusion, and extracellular volume. The RAAS pathway begins by the expression and secretion of renin, the rate-limiting processing enzyme that is synthesized as a preprohormone. Renin is mainly synthesized and stored in the juxtraglomerular (JG) apparatus, composed of JG cells and macula densa. The JG apparatus lines the afferent arteriole of the renal glomerulus.
Four important factors interplay to regulate the secretion of renin: Renin cleaves the N-terminal portion of angiotensinogen, a compound that is mainly expressed by the liver at a stable rate. Angiotensinogen cleavage results in the formation of angiotensin I, a biologically inert decapeptide. Angiotensin I is hydrolyzed by angiotensin-converting enzyme (ACE) or kininase II, an enzyme on plasma membranes of endothelial cells, neuroepithelial cells, and renal proximal tubule cells. ACE acts by removing the C-terminal dipeptide to form angiotensin II, an octapeptide. Also, ACE has a role in metabolizing bradykinin and kallidin, which are important vasodilator peptides. Unlike angiotensin I, angiotensin II is an active potent vasoconstrictor. Angiotensin II is the primary effector of numerous actions. The prescribed medication to treat the patient's hypertension is most likely an ACE-inhibitor. It is indicated as first line agent for the management of hypertension, and has compelling indications in specific cases such as diabetic nephropathy and left ventricular hypertrophy. Classical adverse effects of ACE-I are angioedema, cough, and hyperkalemia. Cough is caused by the action of ACE-I that inhibits the physiological breakdown of bradykinin induced by ACE, resulting in the accumulation of bradykinin with activation of inflammatory peptides and release of histamine. |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Angiotensin, WBRKeyword::Angiotensin I, WBRKeyword::Angiotensin II, WBRKeyword::Angiotensin 1, WBRKeyword::Angiotensin 2, WBRKeyword::AldosteroneAngiotensinogen, WBRKeyword::RAAS, WBRKeyword::Pathway, WBRKeyword::Receptor, WBRKeyword::Blocker, WBRKeyword::Converting, WBRKeyword::Adverse effect, WBRKeyword::Adverse, WBRKeyword::Enzyme, WBRKeyword::ACE, WBRKeyword::Inhibitor, WBRKeyword::ACE inhibitor, WBRKeyword::Cough, WBRKeyword::Bradykinin, WBRKeyword::Side, WBRKeyword::effect |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |