Serotonin syndrome
| Serotonin syndrome | |
 | |
|---|---|
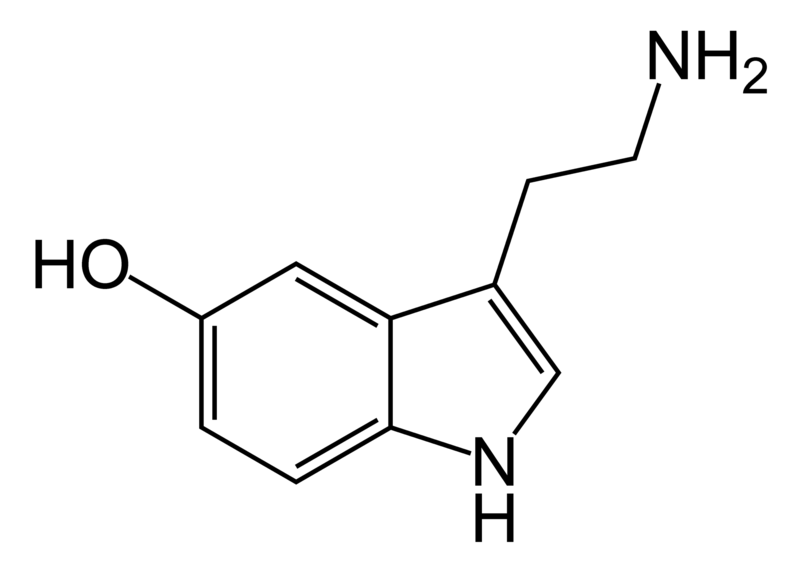
| Serotonin |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Serotonin syndrome is a rare, but potentially life-threatening adverse drug reaction that results from intentional self-poisoning, therapeutic drug use, or inadvertent interactions between drugs. It is an iatrogenic (i.e. caused by medical treatment) toxidrome. It is most commonly referred to as serotonin syndrome, however, serotonin toxicity or serotonin toxidrome (from toxic + syndrome) are more accurate as it reflects the fact that it is a form of poisoning.[1][2] Rarely it may also be called serotonin storm.
Serotonin syndrome is not a spontaneous drug reaction, it is a consequence of excess serotonergic activity at central nervous system (CNS) and peripheral serotonin receptors. This excess serotonin activity produces a specific spectrum of clinical findings which may range from barely perceptible to fatal.[3]
Mechanism
Serotonin syndrome is caused by increased serotonin in the central nervous system. It is the result of overstimulation of 5-HT1A receptors in central grey nuclei and the medulla and, perhaps, of overstimulation of 5-HT2 receptors.[3][4] These changes are more pronounced following supra-therapeutic doses and overdoses, and they merge in a continuum with the toxic effects.[5][6][7]
Drugs Which May Contribute
A large number of drugs and drug combinations have been associated with the serotonin syndrome.
| Class | Drugs |
|---|---|
| herbs | St John's Wort, Yohimbe |
| antidepressants | Monoamine oxidase inhibitors (MAOs), TCAs, SSRIs, SNRIs, mirtazapine, venlafaxine, duloxetine |
| opioids | tramadol, pethidine, oxycodone, morphine, meperidine |
| CNS stimulants | phentermine, diethylpropion, amphetamines, sibutramine, methylphenidate |
| 5-HT1 agonists | triptans (Naratriptan) |
| 5-HT3 antagonists | granisetron |
| illicit drugs | methylenedioxymethamphetamine (MDMA or ecstasy), lysergic acid diethylamide (LSD), cocaine, PMA |
| others | tryptophan, buspirone,dolasetron mesylate, kanna, lithium, linezolid, Lorcaserin, dextromethorphan (DXM), 5-Hydroxytryptophan, chlorpheniramine, Cyclobenzaprine, bupropion, Methylene blue, Netupitant and palonosetron,[8], risperidone, Sumatriptan[9] |
| Reference: Rossi, 2005;[10] National Prescribing Service, 2005[11] | |
The combination of MAOIs and other serotonin agonists or precursors poses a particularly severe risk of a life-threatening serotonin syndrome episode. Many MAOIs inhibit monoamine oxidase irreversibly, so that the enzyme cannot function until it has been replaced by the body, which can take at least two weeks. A dangerous serotonin syndrome reaction can occur unless serotonin agonists and even serotonin precursors such as foods containing tryptophan are strictly avoided until the monoamine oxidase has been replaced.
There have been no peer-reviewed case studies linking a combination of SSRIs and marijuana to serotonin syndrome, though numerous anecdotal reports exist on the internet.
Spectrum Concept
A recently postulated ‘spectrum concept’ of serotonin toxicity emphasises the role that progressively increasing serotonin levels play in mediating the clinical picture as side effects merge into toxicity. The dose effect relationship is the term used to describe the effects of progressive elevation of serotonin, either by raising the dose of one drug, or combining it with another serotonergic drug (which may produce large elevations in serotonin levels).[12]
Risk and Severity
The relative risk and severity of serotonergic side effects and serotonin toxicity, with individual drugs and combinations, is complex. The serotonergic toxicity of SSRIs increases with dose, but even in over-dose it is insufficient to cause fatalities from serotonin syndrome in healthy adults. The syndrome occurs in approximately 14 to 16 percent of persons who overdose on SSRIs.[6] It is usually only when drugs with different mechanisms of action are mixed together that elevations of central nervous system serotonin reach potentially fatal levels. The most frequent (and perhaps the only) combination of therapeutic drugs likely to elevate serotonin to that degree is the combination of monoamine oxidase inhibitors with serotonin reuptake inhibitors (various drugs, other than SSRIs, have clinically significant potency as serotonin reuptake inhibitors, e.g. tramadol, amphetamine, and mdma[13].
The relative risk of serotonin toxicity provides some clues and insights about the nature and extent of drugs’ serotonergic effects. For example, it suggests mirtazapine, which has no serotonergic toxicity, has no significant serotonergic effects at all, and is not in fact a dual action drug.[14]
Symptoms
Symptom onset is usually rapid, often occurring within minutes after self-poisoning or a change in medication. Serotonin syndrome encompasses a wide range of clinical findings. Mild symptoms may only consist of tachycardia, and shivering, diaphoresis, mydriasis, intermittent tremor or myoclonus, as well as overactive or overresponsive reflexes. In addition moderate intoxication includes abnormalities such as hyperactive bowel sounds, hypertension and hyperthermia; a temperature as high as 40°C (104°F) is common in moderate intoxication. The overactive reflexes and clonus in moderate cases may be greater in the lower limbs than in the upper limbs. Mental status changes include hypervigilance and agitation.[3]
Severe symptoms include severe hypertension and tachycardia that may lead to shock. Severe case often have agitated delirium as well as muscular rigidity and high muscular tension. Temperature may rise to above 41.1°C (105.98°F) in life-threatening cases. Other abnormalities include metabolic acidosis, rhabdomyolysis, seizures, renal failure, and disseminated intravascular coagulation.[3]
The symptoms are often described as a clinical triad of abnormalities:
- Cognitive effects: mental confusion, hypomania, hallucinations, agitation, headache, coma.
- Autonomic effects: shivering, sweating, fever, hypertension, tachycardia, nausea, diarrhea.
- Somatic effects: myoclonus/clonus (muscle twitching), hyperreflexia, tremor.
Diagnosis
There is no lab test for serotonin syndrome, so diagnosis is by symptom observation and the patient’s history. Serotonin toxicity is a toxidrome (i.e. has a characteristic picture). It is unique and hard to confuse with other medical conditions but in some situations it may go unrecognized because it may be mistaken for a viral illness, anxiety, neurological disorder, or worsening psychiatric condition.[15] Much confusion has been produced by muddling it with side effects from serotonergic drugs. These rarely, if ever, become dangerous or fatal. Clinicians must also differentiate between serotonin syndrome and neuroleptic malignant syndrome, which has similar symptoms. Patients taking serotonergic drugs and who have sudden onset of symptoms should immediately seek medical care.
The findings of serotonin syndrome, with use of Sternbach, Radomski and Hunter diagnostic criteria and comparison to malignant hypothermia, have been systematically reviewed.[16]
An important finding is clonus.[3]
Differential diagnosis
The distinction between serotonin syndrome, neuroleptic malignant syndrome, malignant hyperthermia, and toxicity from cholinergic agents has been reviewed (see chart).[3] The most difficult distinction is between serotonin syndrome and neuroleptic malignant syndrome as patients may be on drugs that could cause either disorder. Serotonin syndrome shows hyperkinesia, hyperreflexia, and hyperactive bowel sounds, while neuroleptic malignant syndrome shows bradykinesia, bradyreflexia and normal or diminished bowel sounds. A helpful guide is that "dopamine antagonists [such as used to sedate a psychosis] produce bradykinesia, whereas serotonin agonists [such as used to reduce depression] produce hyperkinesia".[3] Lastly, neuroleptic malignant syndrome may develop over several days while serotonin syndrome develops faster.
Management
There is no antidote to the condition itself, and management involves the removal of the precipitating drugs, the initiation of supportive care, the control of agitation, the administration of serotonin antagonists (cyproheptadine or methysergide), the control of autonomic instability, and the control of hyperthermia.[17][3]
The intensity of therapy depends on the severity of symptoms. If the symptoms are mild, treatment may only consist of discontinuation of the offending medication or medications, offering supportive measures, giving benzodiazepines, and waiting for the symptoms to resolve. If the offending medication is discontinued, the condition will often resolve on its own within 24 hours.[18][19] Moderate cases should have all thermal and cardiorespiratory abnormalities corrected and can benefit from serotonin antagonists (i.e. cyproheptadine). Critically ill patients should receive the above therapies as well as sedation, neuromuscular paralysis, and intubation.[3]
Neuroleptic Malignant Syndrome and Serotonin Syndrome
The clinical features of neuroleptic malignant syndrome (NMS) and serotonergic syndrome are very similar. This can make differentiating them very difficult.[20]
Features, classically present in NMS, that are useful for differentiating the two syndromes are:[21]
- Fever
- Muscle rigidity
- Labratory values (increased WBC and CK)
Famous Cases
The death of Libby Zion was due to serotonin syndrome caused by a combination of meperidine and phenelzine.[3] This case had a profound impact on graduate medical education and residency work hour limitations.[22]
References
- ↑ Gillman P (2004). "Comment on: Serotonin syndrome due to co-administration of linezolid and venlafaxine". J Antimicrob Chemother. 54 (4): 844–5. PMID 15317745.
- ↑ Gillman PK (2005). "Serotonin toxicity, serotonin syndrome: 2005 update, overview and analysis". Retrieved 17.11. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Check date values in:|accessdate=(help) - ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Boyer EW, Shannon M (2005). "The serotonin syndrome". N. Engl. J. Med. 352 (11): 1112–20. doi:10.1056/NEJMra041867. PMID 15784664.
- ↑ Gillman PK (1999). "The serotonin syndrome and its treatment". J. Psychopharmacol. (Oxford). 13 (1): 100–9. PMID 10221364.
- ↑ Whyte IM, Serotonin Toxicity (Syndrome). in Medical Toxicology, Dart RC, Editor. 2004, Lippincott Williams & Wilkins: Baltimore. p. 103–6.
- ↑ 6.0 6.1 Isbister G, Bowe S, Dawson A, Whyte I (2004). "Relative toxicity of selective serotonin reuptake inhibitors (SSRIs) in overdose". J Toxicol Clin Toxicol. 42 (3): 277–85. PMID 15362595.
- ↑ Whyte I, Dawson A, Buckley N (2003). "Relative toxicity of venlafaxine and selective serotonin reuptake inhibitors in overdose compared to tricyclic antidepressants". QJM. 96 (5): 369–74. PMID 12702786.
- ↑ Munhoz RP (2004). "Serotonin syndrome induced by a combination of bupropion and SSRIs". Clinical neuropharmacology. 27 (5): 219–22. PMID 15602102.
- ↑ Karki SD, Masood GR (2003). "Combination risperidone and SSRI-induced serotonin syndrome". The Annals of pharmacotherapy. 37 (3): 388–91. PMID 12639169.
- ↑ Rossi S, editor. Australian Medicines Handbook 2005. Adelaide: Australian Medicines Handbook; 2005. ISBN 0-9578521-9-3
- ↑ "Prescribing Practice Review 32: Managing depression in primary care". National Prescribing Service Limited. 2005. Retrieved 16 July. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Check date values in:|accessdate=(help) - ↑ Gillman PK (2006). "Serotonin toxicity: 3 Spectrum concept". Retrieved 17 November. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Check date values in:|accessdate=(help) - ↑ Vuori E, Henry J, Ojanperä I, Nieminen R, Savolainen T, Wahlsten P, Jäntti M (2003). "Death following ingestion of MDMA (ecstasy) and moclobemide". Addiction. 98 (3): 365–8. PMID 12603236.
- ↑ Gillman P (2006). "A systematic review of the serotonergic effects of mirtazapine in humans: implications for its dual action status". Hum Psychopharmacol. 21 (2): 117–25. PMID 16342227.
- ↑ Fennell J, Hussain M (2005). "Serotonin syndrome:case report and current concepts". Ir Med J. 98 (5): 143–4. PMID 16010782.
- ↑ Werneke U, Jamshidi F, Taylor DM, Ott M (2016). "Conundrums in neurology: diagnosing serotonin syndrome - a meta-analysis of cases". BMC Neurol. 16: 97. doi:10.1186/s12883-016-0616-1. PMC 4941011. PMID 27406219.
- ↑ Sporer K (1995). "The serotonin syndrome. Implicated drugs, pathophysiology and management". Drug Saf. 13 (2): 94–104. PMID 7576268.
- ↑ Prator B (2006). "Serotonin syndrome". J Neurosci Nurs. 38 (2): 102–5. PMID 16681290.
- ↑ Jaunay E, Gaillac V, Guelfi J (2001). "[Serotonin syndrome. Which treatment and when?]". Presse Med. 30 (34): 1695–700. PMID 11760601.
- ↑ Christensen V, Glenthøj B (2001). "[Malignant neuroleptic syndrome or serotonergic syndrome]". Ugeskr Laeger. 163 (3): 301–2. PMID 11219110.
- ↑ Birmes P, Coppin D, Schmitt L, Lauque D (2003). "Serotonin syndrome: a brief review". CMAJ. 168 (11): 1439–42. PMID 12771076. Full Free Text.
- ↑ Brensilver JM, Smith L, Lyttle CS (1998). "Impact of the Libby Zion case on graduate medical education in internal medicine". Mt. Sinai J. Med. 65 (4): 296–300. PMID 9757752.
External links
- Dr P K Gillman's site, 'PsychoTropicalResearch', devoted to Serotonin and 'Serotonin Syndrome' research.
- Template:FPnotebook
- Great article with a plethora of information on the toxidrome; its causes and statistics involving the subsidiation of the toxidrome.
de:Serotonin-Syndrom no:Serotonin syndrome fi:Serotoniinioireyhtymä sv:Serotonergt syndrom