Sandbox:Dima
Scabies
Pathophysiology
Overview
The mite Sarcoptes scabieii produces the symptoms by tunneling into the stratum corneum and depositing in the burrow. The disease is transmitted mainly by skin to skin contact.
Pathophysiology
Life Cycle
- The mite Sarcoptes scabiei produces intense, itchy skin rashes when the impregnated female tunnels into the stratum corneum of the skin and deposits eggs in the burrow.
- The larvae, which hatch in 3-10 days, move about on the skin, molt into a "nymphal" stage, and then mature into adult mites. The adult mites live 3-4 weeks in the host's skin.
- The action of the mites moving within the skin and on the skin itself produces an intense itch which may resemble an allergic reaction in appearance. The presence of the eggs produces a massive allergic response which, in turn, produces more itching. The symptoms are caused by an allergic reaction that the body develops over time to the mites and their by-products under the skin, thus the 4-6 week "incubation" period. There are usually relatively few mites on a normal, healthy person's skin; about 11 females in burrows. Scabies are microscopic although sometimes they are visible as a pinpoint of white. The females burrow into the skin and lay eggs there. Males roam on top of the skin, however, they can and do occasionally burrow. Both males and females surface at times, especially at night.
- They can be washed or scratched off (however scratching should be done with a washcloth to avoid cutting the skin as this can lead to infection), which, although not a cure, helps to keep the total population low. Also, humans create antibodies to the scabies mites which do kill some of them.
Transmission
- Scabies is transmitted readily, often throughout an entire household, by skin-to-skin contact with an infected person (e.g. bed partners, schoolmates, daycare), and thus is sometimes, although inaccurately, classed as a sexually transmitted disease. Spread by clothing, bedding, or towels is a less significant risk, though possible.
- It takes approximately 4-6 weeks to develop symptoms after initial infestation. Therefore, a person may have been contagious for at least a month before being diagnosed. This means that person might have passed scabies to anyone at that time with whom they had close contact. Someone who sleeps in the same room with a person with scabies has a high possibility of having scabies as well, although they may not show symptoms.
NH, C and Prognosis
Overview
A delayed hypersensitivity (allergic) response resulting in a papular eruption (red, elevated area on skin) often occurs 30-40 days after infestation.The rash may become secondarily infected; scratching the rash may break the skin and make secondary infection more likely. In persons with severely reduced immunity, such as those with HIV infection, or people being treated with immunosuppressive drugs like steroids, a widespread rash with thick scaling may result in Norwegian scabies.
Natural History, Complications and Prognosis
- A delayed hypersensitivity (allergic) response resulting in a papular eruption (red, elevated area on skin) often occurs 30-40 days after infestation. While there may be hundreds of papules, fewer than 10 burrows are typically found.
- The rash may become secondarily infected; scratching the rash may break the skin and make secondary infection more likely. In persons with severely reduced immunity, such as those with HIV infection, or people being treated with immunosuppressive drugs like steroids, a widespread rash with thick scaling may result. This variety of scabies is called Norwegian scabies.
- Scabies is frequently misdiagnosed as intense pruritus (itching of healthy skin) before papular eruptions form. Upon initial pruritus the burrows appear as small, barely noticeable bumps on the hands and may be slightly shiny and dark in color rather than red. Initially the itching may not exactly correlate to the location of these bumps. As the infestation progresses, these bumps become more red in color.
- People with compromised immune systems may not develop antibodies to the mites and may develop crusted Norwegian scabies. In this case, many form scabs or develop very red skin especially in the elderly and the mentally handicapped where white or gray crusted areas develop with little itching and little or no red bumps and mite population numbers soar to hundreds, thousands, or millions in AIDS patients. These cases require additional treatment options to ensure a complete kill. Ivermectin is the treatment of choice in these patients combined with any other topical treatment.
Evolution of the Infection
-
Day 4
-
Day 8 (treatment begins)
-
Day 12 (under treatment)
-
Healed
History and Symptoms
Overview
The most common symptoms of scabies, itching and a skin rash, are caused by sensitization (a type of “allergic” reaction) to the proteins and feces of the parasite. Severe itching (pruritus), especially at night, is the earliest and most common symptom of scabies. A pimple-like (papular) itchy (pruritic) “scabies rash” is also common.
History and Symptoms
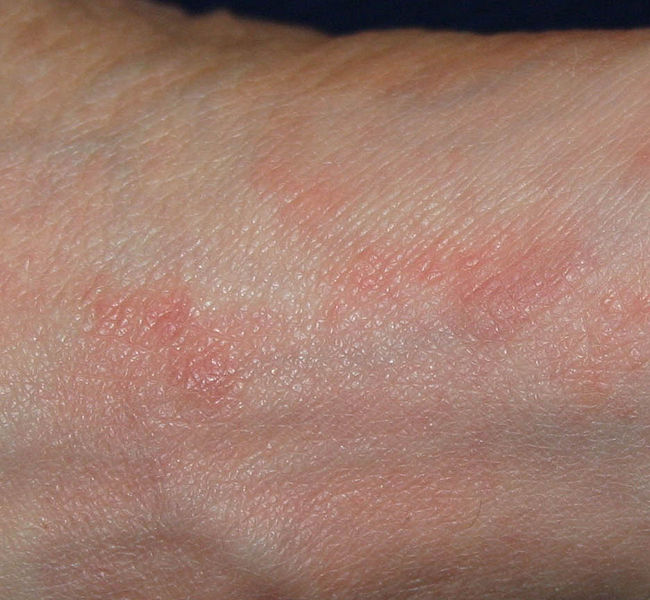
- A delayed hypersensitivity (allergic) response resulting in a papular eruption (red, elevated area on skin) often occurs 30-40 days after infestation. While there may be hundreds of papules, fewer than 10 burrows are typically found. The burrow appears as a fine, wavy and slightly scaly line a few millimeters to one centimeter long. A tiny mite (0.3 to 0.9.08 mm) may sometimes be seen at the end of the burrow. Most burrows occur in the webs of fingers, flexing surfaces of the wrists, around elbows and armpits, the areolae of the breasts in females and on genitals of males, along the belt line, and on the lower buttocks. The face usually does not become involved in adults.
- Generally diagnosis is made by finding burrows, which often may be difficult because they are scarce, and they are obscured by scratch marks, or by secondary dermatitis (unrelated skin irritation). If burrows are not found in the primary areas known to be affected, the entire skin surface of the body should be examined.

Physical Exam
Physical Examination
Gallery
Skin
-
Scabies (common location in ventral wrist) [1]
Ears
Extremities
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
Trunk
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
Genitales
Face
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
-
Norwegian scabies. Adapted from Dermatology Atlas.[2]
Physical exam
Overview
Laboratory diagnosis may be confirmed by microscopy of surface scrapings, which are placed on a slide in glycerol, mineral oil or immersion in oil and covered with a coverslip.
Laboratory Findings
- The suspicious area can be rubbed with ink from a fountain pen or alternately a topical tetracycline solution which will glow under a special light. The surface is then wiped off with an alcohol pad; if the person is infected with scabies, the characteristic zigzag or S pattern of the burrow across the skin will appear.
- When a suspected burrow is found, diagnosis may be confirmed by microscopy of surface scrapings, which are placed on a slide in glycerol, mineral oil or immersion in oil and covered with a coverslip. Avoiding potassium hydroxide is necessary because it may dissolve fecal pellets. Positive diagnosis is made when the mite, ova, or fecal pellets are found.
Medical Therapy
Overview
Medical therapy of scabies includes either topical permethrin or oral ivermectin. Patients may become completely asymptomatic within 1-2 weeks following therapy.
Medical Therapy
- All patients with scabies require antimicrobial therapy. Medical therapy of scabies includes either topical permethrin or oral ivermectin.
- Patients may experience worsening pruritus and erythema early during the administration of antimicrobial therapy.
- The parasite is gradually eliminated during the body's natural shedding process.
- Antimicrobial therapy[3]
- 1. Adult
- Preferred regimen (1): Permethrin 5% cream applied to all areas of the body from the neck down and washed off after 8–14 hours
- Preferred regimen (2): Ivermectin 200 ug/kg PO qd and repeated in 2 weeks
- Alternative regimen: Lindane (1%) 1 oz of lotion or 30 g of cream applied in a thin layer to all areas of the body from the neck down and thoroughly washed off after 8 hours
- Note: Patients may experience worsening pruritus and erythema early during the administration of antimicrobial therapy
- 2. Infants and young children
- Preferred regimen: Permethrin 5% cream applied to all areas of the body from the neck down and washed off after 8–14 hours
- Note: Infants and young children aged< 10 years should not be treated with lindane
- 3. Crusted Scabies
- Preferred regimen: (Topical scabicide 5% topical Benzyl benzoate 5% OR topical Permethrin 5% cream (full-body application to be repeated daily for 7 days then twice weekly until discharge or cure) AND treatment with Ivermectin 200 ug/kg PO on days 1,2,8,9, and 15. Additional Ivermectin treatment on days 22 and 29 might be required for severe cases
- 4.Pregnant or Lactating Women
- Preferred regimen: Permethrin 5% cream applied to all areas of the body from the neck down and washed off after 8–14 hours
Primary Prevention
Overview
Scabies is prevented by avoiding direct skin-to-skin contact with an infested person or with items such as clothing or bedding used by an infested person. Scabies treatment usually is recommended for members of the same household, particularly for those who have had prolonged skin-to-skin contact.
Primary Prevention
- All family and close contacts should be treated at the same time, even if asymptomatic. After treatment has been applied or taken, (or directly before treatment if you are careful and wear gloves) cleaning of environment should occur. A person can easily be reinfected with scabies.
- Without a host, scabies mites can on average survive up to 48-72 hours away from human skin. [1] As in cases of Crusted Scabies, they can survive much longer, up to 7 days. Therefore it is recommended, after treatment, to wash all material (such as clothes, bedding, and towels) that has been in contact with all infested persons in the last three days.
- All household members should be treated at the same time and cleaning must be thorough and simultaneous. Either isolate long enough for the mites to die in a plastic bag for at least 1 week, or clean or freeze overnight.
- Vacuuming floors, carpets, and rugs.
- Disinfecting floor and bathroom surfaces by mopping (this only needs to be done after the first treatment).
- Daily washing of recently worn clothes, towels and bedding in hot water and drying in a hot dryer.
- Hot drying pillows for 30 minutes.
- Overnight freezing, in a plastic bag: stuffed animals, brushes, combs, shoes, coats, gloves, hats, robes, wetsuits, etc.
- Quarantine in a plastic bag for two weeks: things that cannot be washed, hot dried, frozen or drycleaned.
- Drycleaning: things that cannot be washed, hot dried or frozen or quarantined.
Primary Prevention for Pets
- Pets and humans get infected with different types of mites. The mites that we get can not survive and reproduce on pets.
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 2.27 2.28 2.29 2.30 2.31 2.32 2.33 2.34 2.35 2.36 2.37 2.38 2.39 2.40 2.41 2.42 2.43 2.44 2.45 2.46 2.47 2.48 "Dermatology Atlas".
- ↑ Workowski, Kimberly A.; Bolan, Gail A. (2015-06-05). "Sexually transmitted diseases treatment guidelines, 2015". MMWR. Recommendations and reports: Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 64 (RR-03): 1–137. ISSN 1545-8601. PMID 26042815.











![Scabies (common location in ventral wrist) [1]](/images/7/75/Scabies_%28common_location_is_ventral_wrist%29.jpg)

![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/b/b2/Norwegian_scabies25.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/1/15/Norwegian_scabies26.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/1/18/Norwegian_scabies27.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/e/e1/Norwegian_scabies28.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/5/57/Norwegian_scabies29.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/4/43/Norwegian_scabies30.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/7/76/Norwegian_scabies32.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/9/92/Norwegian_scabies41.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/7/73/Norwegian_scabies42.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/e/ef/Norwegian_scabies43.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/e/e3/Norwegian_scabies44.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/2/25/Norwegian_scabies45.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/b/b4/Norwegian_scabies46.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/d/dd/Norwegian_scabies47.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/b/b4/Norwegian_scabies51.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/5/5b/Norwegian_scabies52.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/4/4c/Norwegian_scabies01.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/8/83/Norwegian_scabies02.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/e/e0/Norwegian_scabies05.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/8/82/Norwegian_scabies06.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/3/30/Norwegian_scabies07.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/5/50/Norwegian_scabies13.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/f/ff/Norwegian_scabies14.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/4/48/Norwegian_scabies15.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/2/2a/Norwegian_scabies16.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/8/8f/Norwegian_scabies17.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/6/60/Norwegian_scabies18.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/3/38/Norwegian_scabies19.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/5/5b/Norwegian_scabies20.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/9/94/Norwegian_scabies21.jpg)










![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/b/bd/Norwegian_scabies08.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/6/61/Norwegian_scabies09.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/e/e8/Norwegian_scabies10.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/5/52/Norwegian_scabies11.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/f/f9/Norwegian_scabies12.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/c/c7/Norwegian_scabies31.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/2/23/Norwegian_scabies33.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/f/fc/Norwegian_scabies34.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/c/c4/Norwegian_scabies48.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/4/45/Norwegian_scabies49.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/8/8d/Norwegian_scabies50.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/f/ff/Norwegian_scabies03.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/4/4c/Norwegian_scabies04.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/d/d3/Norwegian_scabies35.jpg)













![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/a/a9/Norwegian_scabies22.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/b/b1/Norwegian_scabies23.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/6/66/Norwegian_scabies24.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/7/78/Norwegian_scabies36.jpg)
![Norwegian scabies. Adapted from Dermatology Atlas.[2]](/images/6/6a/Norwegian_scabies37.jpg)