Ombitasvir / paritaprevir / ritonavir / dasabuvir
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sonya Gelfand
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
RISK OF HEPATITIS B VIRUS REACTIVATION IN PATIENTS COINFECTED WITH HCV AND HBV
See full prescribing information for complete Boxed Warning.
|
Overview
Ombitasvir / paritaprevir / ritonavir / dasabuvir is a a combination of three direct-acting hepatitis C virus antiviral agents with distinct mechanisms of action that is FDA approved for the treatment of adult patients with chronic hepatitis C virus (HCV). There is a Black Box Warning for this drug as shown here. Common adverse reactions include fatigue, nausea, pruritus, other skin reactions, insomnia and asthenia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is indicated for the treatment of adult patients with chronic hepatitis C virus (HCV):
- genotype 1b without cirrhosis or with compensated cirrhosis
- genotype 1a without cirrhosis or with compensated cirrhosis for use in combination with ribavirin.
Testing Prior to the Initiation of Therapy
- Test all patients for evidence of current or prior HBV infection by measuring hepatitis B surface antigen (HBsAg) and hepatitis B core antibody (anti-HBc) before initiating HCV treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir.
- Prior to initiation of ombitasvir / paritaprevir / ritonavir / dasabuvir, assess for laboratory and clinical evidence of hepatic decompensation.
Recommended Dosage in Adults
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is ombitasvir, paritaprevir, ritonavir fixed dose combination tablets copackaged with dasabuvir tablets.
- The recommended oral dosage of ombitasvir / paritaprevir / ritonavir / dasabuvir is two ombitasvir, paritaprevir, ritonavir tablets once daily (in the morning) and one dasabuvir tablet twice daily (morning and evening). Take ombitasvir / paritaprevir / ritonavir / dasabuvir with a meal without regard to fat or calorie content.
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is used in combination with ribavirin (RBV) in certain patient populations (see TABLE 1). When administered with ombitasvir / paritaprevir / ritonavir / dasabuvir, the recommended dosage of RBV is based on weight: 1000 mg/day for subjects <75 kg and 1200 mg/day for those ≥75 kg, divided and administered twice-daily with food. For ribavirin dosage modifications, refer to the ribavirin prescribing information.
- For patients with HCV/HIV-1 co-infection, follow the dosage recommendations in TABLE 1.
- TABLE 1 shows the recommended ombitasvir / paritaprevir / ritonavir / dasabuvir treatment regimen and duration based on patient population.

Use in Liver Transplant Recipients
- In liver transplant recipients with normal hepatic function and mild fibrosis (Metavir fibrosis score 2 or lower), the recommended duration of ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin is 24 weeks, irrespective of HCV genotype 1 subtype. When ombitasvir / paritaprevir / ritonavir / dasabuvir is administered with calcineurin inhibitors in liver transplant recipients, dosage adjustment of calcineurin inhibitors is needed.
Hepatic Impairment
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is contraindicated in patients with moderate to severe hepatic impairment (Child-Pugh B and C).
Dosage Forms and Strengths
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is ombitasvir, paritaprevir, ritonavir fixed dose combination tablets copackaged with dasabuvir tablets.
- Ombitasvir, paritaprevir, ritonavir 12.5/75/50 mg tablets are pink-colored, film-coated, oblong biconvex shaped, debossed with “AV1” on one side.
- Dasabuvir 250 mg tablets are beige-colored, film-coated, oval-shaped, debossed with “AV2” on one side. Each tablet contains 270.3 mg dasabuvir sodium monohydrate equivalent to 250 mg dasabuvir.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding ombitasvir / paritaprevir / ritonavir / dasabuvir Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding ombitasvir / paritaprevir / ritonavir / dasabuvir Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Ombitasvir / paritaprevir / ritonavir / dasabuvir FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding ombitasvir / paritaprevir / ritonavir / dasabuvir Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding ombitasvir / paritaprevir / ritonavir / dasabuvir Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is contraindicated in patients with moderate to severe hepatic impairment (Child-Pugh B and C) due to risk of potential toxicity.
- If ombitasvir / paritaprevir / ritonavir / dasabuvir is administered with ribavirin, the contraindications to ribavirin also apply to this combination regimen. Refer to the ribavirin prescribing information for a list of contraindications for ribavirin.
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is contraindicated:
- With drugs that are highly dependent on CYP3A for clearance and for which elevated plasma concentrations are associated with serious and/or life-threatening events.
- With drugs that are moderate or strong inducers of CYP3A and strong inducers of CYP2C8 and may lead to reduced efficacy of ombitasvir / paritaprevir / ritonavir / dasabuvir.
- With drugs that are strong inhibitors of CYP2C8 and may increase dasabuvir plasma concentrations and the risk of QT prolongation.
- In patients with known hypersensitivity to ritonavir (e.g. toxic epidermal necrolysis (TEN) or Stevens-Johnson syndrome).
- TABLE 2 lists drugs that are contraindicated with ombitasvir / paritaprevir / ritonavir / dasabuvir.

Warnings
|
RISK OF HEPATITIS B VIRUS REACTIVATION IN PATIENTS COINFECTED WITH HCV AND HBV
See full prescribing information for complete Boxed Warning.
|
Risk of Hepatitis B Virus Reactivation in Patients Coinfected with HCV and HBV
- Hepatitis B virus (HBV) reactivation has been reported in HCV/HBV coinfected patients who were undergoing or had completed treatment with HCV direct acting antivirals, and who were not receiving HBV antiviral therapy. Some cases have resulted in fulminant hepatitis, hepatic failure and death. Cases have been reported in patients who are HBsAg positive and also in patients with serologic evidence of resolved HBV infection (i.e., HBsAg negative and anti-HBc positive). HBV reactivation has also been reported in patients receiving certain immunosuppressant or chemotherapeutic agents; the risk of HBV reactivation associated with treatment with HCV direct-acting antivirals may be increased in these patients.
- HBV reactivation is characterized as an abrupt increase in HBV replication manifesting as a rapid increase in serum HBV DNA level. In patients with resolved HBV infection reappearance of HBsAg can occur. Reactivation of HBV replication may be accompanied by hepatitis, i.e., increases in aminotransferase levels and, in severe cases, increases in bilirubin levels, liver failure, and death can occur.
- Test all patients for evidence of current or prior HBV infection by measuring HBsAg and anti-HBc before initiating HCV treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir. In patients with serologic evidence of HBV infection, monitor for clinical and laboratory signs of hepatitis flare or HBV reactivation during HCV treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir and during post-treatment follow-up. Initiate appropriate patient management for HBV infection as clinically indicated.
Risk of Hepatic Decompensation and Hepatic Failure in Patients with Cirrhosis
- Hepatic decompensation and hepatic failure, including liver transplantation or fatal outcomes, have been reported postmarketing in patients treated with ombitasvir / paritaprevir / ritonavir / dasabuvir. Most patients with these severe outcomes had evidence of advanced cirrhosis prior to initiating therapy with ombitasvir / paritaprevir / ritonavir / dasabuvir. Reported cases typically occurred within one to four weeks of initiating therapy and were characterized by the acute onset of rising direct serum bilirubin levels without ALT elevations in association with clinical signs and symptoms of hepatic decompensation. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is contraindicated in patients with moderate to severe hepatic impairment (Child-Pugh B and C).
- For patients with cirrhosis:
- Monitor for clinical signs and symptoms of hepatic decompensation (such as ascites, hepatic encephalopathy, variceal hemorrhage).
- Hepatic laboratory testing including direct bilirubin levels should be performed at baseline and during the first 4 weeks of starting treatment and as clinically indicated.
- Discontinue ombitasvir / paritaprevir / ritonavir / dasabuvir in patients who develop evidence of hepatic decompensation.
Increased Risk of ALT Elevations
- During clinical trials with ombitasvir / paritaprevir / ritonavir / dasabuvir with or without ribavirin, elevations of ALT to greater than 5 times the upper limit of normal (ULN) occurred in approximately 1% of all subjects. ALT elevations were typically asymptomatic, occurred during the first 4 weeks of treatment, and declined within two to eight weeks of onset with continued dosing of ombitasvir / paritaprevir / ritonavir / dasabuvir with or without ribavirin.
- These ALT elevations were significantly more frequent in female subjects who were using ethinyl estradiol-containing medications such as combined oral contraceptives, contraceptive patches or contraceptive vaginal rings. Ethinyl estradiol-containing medications must be discontinued prior to starting therapy with ombitasvir / paritaprevir / ritonavir / dasabuvir. Alternative methods of contraception (e.g, progestin only contraception or non-hormonal methods) are recommended during ombitasvir / paritaprevir / ritonavir / dasabuvir therapy. Ethinyl estradiol-containing medications can be restarted approximately 2 weeks following completion of treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir.
- Women using estrogens other than ethinyl estradiol, such as estradiol and conjugated estrogens used in hormone replacement therapy had a rate of ALT elevation similar to those not receiving any estrogens; however, due to the limited number of subjects taking these other estrogens, caution is warranted for co-administration with ombitasvir / paritaprevir / ritonavir / dasabuvir.
- Hepatic laboratory testing should be performed during the first 4 weeks of starting treatment and as clinically indicated thereafter. If ALT is found to be elevated above baseline levels, it should be repeated and monitored closely:
- Patients should be instructed to consult their health care professional without delay if they have onset of fatigue, weakness, lack of appetite, nausea and vomiting, jaundice or discolored feces.
- Consider discontinuing ombitasvir / paritaprevir / ritonavir / dasabuvir if ALT levels remain persistently greater than 10 times the ULN.
- Discontinue ombitasvir / paritaprevir / ritonavir / dasabuvir if ALT elevation is accompanied by signs or symptoms of liver inflammation or increasing direct bilirubin, alkaline phosphatase, or INR.
Risks Associated With Ribavirin Combination Treatment
- If ombitasvir / paritaprevir / ritonavir / dasabuvir is administered with ribavirin, the warnings and precautions for ribavirin, in particular the pregnancy avoidance warning, apply to this combination regimen. Refer to the ribavirin prescribing information for a full list of the warnings and precautions for ribavirin.
Risk of Adverse Reactions or Reduced Therapeutic Effect Due to Drug Interactions
- The concomitant use of ombitasvir / paritaprevir / ritonavir / dasabuvir and certain other drugs may result in known or potentially significant drug interactions, some of which may lead to:
- Loss of therapeutic effect of ombitasvir / paritaprevir / ritonavir / dasabuvir and possible development of resistance
- Possible clinically significant adverse reactions from greater exposures of concomitant drugs or components of ombitasvir / paritaprevir / ritonavir / dasabuvir.
- See TABLE 5 for steps to prevent or manage these possible and known significant drug interactions, including dosing recommendations. Consider the potential for drug interactions prior to and during ombitasvir / paritaprevir / ritonavir / dasabuvir therapy; review concomitant medications during ombitasvir / paritaprevir / ritonavir / dasabuvir therapy; and monitor for the adverse reactions associated with the concomitant drugs.
Risk of HIV-1 Protease Inhibitor Drug Resistance in HCV/HIV-1 Co-infected Patients
- The ritonavir component of ombitasvir / paritaprevir / ritonavir / dasabuvir is also an HIV-1 protease inhibitor and can select for HIV-1 protease inhibitor resistance-associated substitutions. Any HCV/HIV-1 co-infected patients treated with ombitasvir / paritaprevir / ritonavir / dasabuvir should also be on a suppressive antiretroviral drug regimen to reduce the risk of HIV-1 protease inhibitor drug resistance.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of ombitasvir / paritaprevir / ritonavir / dasabuvir cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The safety assessment was based on data from seven clinical trials in more than 2,000 subjects who received ombitasvir / paritaprevir / ritonavir / dasabuvir with or without ribavirin for 12 or 24 weeks.
- The safety of ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with ribavirin was assessed in 770 subjects with chronic HCV genotype 1 (GT1) infection in two placebo-controlled trials (SAPPHIRE-I and -II). Adverse reactions that occurred more often in subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with ribavirin compared to placebo were fatigue, nausea, pruritus, other skin reactions, insomnia, and asthenia (see TABLE 3). The majority of the adverse reactions were mild in severity. Two percent of subjects experienced a serious adverse event (SAE). The proportion of subjects who permanently discontinued treatment due to adverse reactions was less than 1%.

- Ombitasvir / paritaprevir / ritonavir / dasabuvir with and without ribavirin was assessed in 401 and 509 subjects with chronic HCV infection, respectively, in three clinical trials (PEARL-II, PEARL-III and PEARL-IV). Pruritus, nausea, insomnia, and asthenia were identified as adverse events occurring more often in subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with ribavirin (see TABLE 4). The majority of adverse events were mild to moderate in severity. The proportion of subjects who permanently discontinued treatment due to adverse events was less than 1% for both ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with ribavirin and ombitasvir / paritaprevir / ritonavir / dasabuvir alone.

- Ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin was assessed in 380 subjects with genotype 1 infection and compensated cirrhosis who were treated with ombitasvir / paritaprevir / ritonavir / dasabuvir plus ribavirin for 12 (n=208) or 24 (n=172) weeks duration (TURQUOISE-II). The type and severity of adverse events in subjects with compensated cirrhosis was comparable to non-cirrhotic subjects in other phase 3 trials. Fatigue, skin reactions and dyspnea occurred at least 5% more often in subjects treated for 24 weeks. The majority of adverse events occurred during the first 12 weeks of dosing in both treatment arms. Most of the adverse events were mild to moderate in severity. The proportion of subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir for 12 and 24 weeks with SAEs was 6% and 5%, respectively and 2% of subjects permanently discontinued treatment due to adverse events in each treatment arm.
- Ombitasvir / paritaprevir / ritonavir / dasabuvir without ribavirin for 12 weeks was assessed in 60 subjects with genotype 1b infection and compensated cirrhosis (TURQUOISE-III). The type and severity of adverse events and laboratory abnormalities in genotype 1b-infected subjects with compensated cirrhosis were comparable to subjects in other trials without ribavirin.
Skin Reactions
- In PEARL-II, -III and -IV, 7% of subjects receiving ombitasvir / paritaprevir / ritonavir / dasabuvir alone and 10% of subjects receiving ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin reported rash-related events. In SAPPHIRE-I and -II 16% of subjects receiving ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin and 9% of subjects receiving placebo reported skin reactions. In TURQUOISE-II, 18% and 24% of subjects receiving ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin for 12 or 24 weeks reported skin reactions. The majority of events were graded as mild in severity.
Laboratory Abnormalities
Serum ALT Elevations
- Approximately 1% of subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir experienced post-baseline serum ALT levels greater than 5 times the upper limit of normal (ULN) after starting treatment. The incidence increased to 25% (4/16) among women taking a concomitant ethinyl estradiol containing medication. The incidence of clinically relevant ALT elevations among women using estrogens other than ethinyl estradiol, such as estradiol and conjugated estrogens used in hormone replacement therapy was 3% (2/59).
- ALT elevations were typically asymptomatic, generally occurred during the first 4 weeks of treatment (mean time 20 days, range 8-57 days) and most resolved with ongoing therapy. The majority of these ALT elevations were assessed as drug-related liver injury. Elevations in ALT were generally not associated with bilirubin elevations. Cirrhosis was not a risk factor for elevated ALT.
Serum Bilirubin Elevations
- Post-baseline elevations in bilirubin at least 2 x ULN were observed in 15% of subjects receiving ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin compared to 2% in those receiving ombitasvir / paritaprevir / ritonavir / dasabuvir alone. These bilirubin increases were predominately indirect and related to the inhibition of the bilirubin transporters OATP1B1/1B3 by paritaprevir and ribavirin-induced hemolysis. Bilirubin elevations occurred after initiation of treatment, peaked by study Week 1, and generally resolved with ongoing therapy. Bilirubin elevations were not associated with serum ALT elevations.
Anemia/Decreased Hemoglobin
- Across all Phase 3 studies, the mean change from baseline in hemoglobin levels in subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with ribavirin was -2.4 g/dL and the mean change in subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir alone was -0.5 g/dL. Decreases in hemoglobin levels occurred early in treatment (Week 1-2) with further reductions through Week 3. Hemoglobin values remained low during the remainder of treatment and returned towards baseline levels by post-treatment Week 4. Less than 1% of subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin had hemoglobin levels decrease to less than 8.0 g/dL during treatment. Seven percent of subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with ribavirin underwent a ribavirin dose reduction due to a decrease in hemoglobin levels; three subjects received a blood transfusion and five required erythropoietin. One patient discontinued therapy due to anemia. No subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir alone had a hemoglobin level less than 10 g/dL.
- Ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin was assessed in 63 subjects with HCV/HIV-1 co-infection who were on stable antiretroviral therapy. The most common adverse events occurring in at least 10% of subjects were fatigue (48%), insomnia (19%), nausea (17%), headache (16%), pruritus (13%), cough (11%), irritability (10%), and ocular icterus (10%).
- Elevations in total bilirubin greater than 2 x ULN (mostly indirect) occurred in 34 (54%) subjects. Fifteen of these subjects were also receiving atazanavir at the time of bilirubin elevation and nine also had adverse events of ocular icterus, jaundice or hyperbilirubinemia. None of the subjects with hyperbilirubinemia had concomitant elevations of aminotransferases. No subject experienced a grade 3 ALT elevation.
- Seven subjects (11%) had at least one post-baseline hemoglobin value of less than 10 g/dL, and six of these subjects had a ribavirin dose modification; no subject in this small cohort required a blood transfusion or erythropoietin.
- Median declines in CD4+ T-cell counts of 47 cells/mm3 and 62 cells/mm3 were observed at the end of 12 and 24 weeks of treatment, respectively, and most returned to baseline levels post-treatment. Two subjects had CD4+ T-cell counts decrease to less than 200 cells/mm3 during treatment without a decrease in CD4%. No subject experienced an AIDS-related opportunistic infection.
- Ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin was assessed in 34 post-liver transplant subjects with recurrent HCV infection. Adverse events occurring in more than 20% of subjects included fatigue 50%, headache 44%, cough 32%, diarrhea 26%, insomnia 26%, asthenia 24%, nausea 24%, muscle spasms 21% and rash 21%. Ten subjects (29%) had at least one post-baseline hemoglobin value of less than 10 g/dL. Ten subjects underwent a ribavirin dose modification due to decrease in hemoglobin and 3% (1/34) had an interruption of ribavirin. Five subjects received erythropoietin, all of whom initiated ribavirin at the starting dose of 1000 to 1200 mg daily. No subject received a blood transfusion.
Postmarketing Experience
- The following adverse reactions have been identified during post approval use of ombitasvir / paritaprevir / ritonavir / dasabuvir. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Immune System Disorders: Hypersensitivity reactions (including angioedema).
- Hepatobiliary Disorders: Hepatic decompensation, hepatic failure.
- Skin and Subcutaneous Tissue Disorders: Erythema multiforme (EM).
Drug Interactions
- Potential for Ombitasvir / paritaprevir / ritonavir / dasabuvir to Affect Other Drugs
- Potential for Other Drugs to Affect One or More Components of ombitasvir / paritaprevir / ritonavir / dasabuvir
- Established and Other Potential Drug Interactions
- Drugs without Clinically Significant Interactions with ombitasvir / paritaprevir / ritonavir / dasabuvir
- Ombitasvir, paritaprevir, and dasabuvir are inhibitors of UGT1A1, and ritonavir is an inhibitor of CYP3A4. Paritaprevir is an inhibitor of OATP1B1 and OATP1B3 and paritaprevir, ritonavir and dasabuvir are inhibitors of BCRP. Co-administration of ombitasvir / paritaprevir / ritonavir / dasabuvir with drugs that are substrates of CYP3A, UGT1A1, BCRP, OATP1B1 or OATP1B3 may result in increased plasma concentrations of such drugs.
- Fluctuations in INR values may occur in patients receiving warfarin concomitant with HCV treatment, including treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir. If ombitasvir / paritaprevir / ritonavir / dasabuvir is coadministered with warfarin, close monitoring of INR values is recommended during treatment and post-treatment follow-up.
- Paritaprevir and ritonavir are primarily metabolized by CYP3A enzymes. Co-administration of ombitasvir / paritaprevir / ritonavir / dasabuvir with strong inhibitors of CYP3A may increase paritaprevir and ritonavir concentrations. Dasabuvir is primarily metabolized by CYP2C8 enzymes. Co-administration of ombitasvir / paritaprevir / ritonavir / dasabuvir with drugs that inhibit CYP2C8 may increase dasabuvir plasma concentrations. Ombitasvir is primarily metabolized via amide hydrolysis while CYP enzymes play a minor role in its metabolism. Ombitasvir, paritaprevir, dasabuvir and ritonavir are substrates of P-gp. Ombitasvir, paritaprevir and dasabuvir are substrates of BCRP. Paritaprevir is a substrate of OATP1B1 and OATP1B3. Inhibition of P-gp, BCRP, OATP1B1 or OATP1B3 may increase the plasma concentrations of the various components of ombitasvir / paritaprevir / ritonavir / dasabuvir.
Established and Other Potential Drug Interactions
- If dose adjustments of concomitant medications are made due to treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir, doses should be re-adjusted after administration of ombitasvir / paritaprevir / ritonavir / dasabuvir is completed. Dose adjustment is not required for ombitasvir / paritaprevir / ritonavir / dasabuvir.
- TABLE 5 provides the effect of co-administration of ombitasvir / paritaprevir / ritonavir / dasabuvir on concentrations of concomitant drugs and the effect of concomitant drugs on the various components of ombitasvir / paritaprevir / ritonavir / dasabuvir. Refer to the ritonavir prescribing information for other potentially significant drug interactions with ritonavir.

- No dose adjustments are recommended when ombitasvir / paritaprevir / ritonavir / dasabuvir is co-administered with the following medications: abacavir, dolutegravir, digoxin, duloxetine, emtricitabine/tenofovir disoproxil fumarate, escitalopram, lamivudine, methadone, progestin only contraceptives, raltegravir, sofosbuvir, sulfamethoxazole, trimethoprim, and zolpidem.
Use in Specific Populations
Pregnancy
Risk Summary
- If ombitasvir / paritaprevir / ritonavir / dasabuvir is administered with ribavirin, the combination regimen is contraindicated in pregnant women and in men whose female partners are pregnant. Refer to the ribavirin prescribing information for more information on use in pregnancy.
- No adequate human data are available to establish whether or not ombitasvir / paritaprevir / ritonavir / dasabuvir poses a risk to pregnancy outcomes. In animal reproduction studies, no adverse developmental effects were observed when the components of ombitasvir / paritaprevir / ritonavir / dasabuvir were administered separately during organogenesis and lactation. During organogenesis, the exposures were up to 28 and 4 times (mice and rabbits, respectively; ombitasvir), 98 and 8 times (mice and rats, respectively; paritaprevir, ritonavir), and 24 and 6 times (rats and rabbits, respectively; dasabuvir) exposures at the recommended clinical dose of ombitasvir / paritaprevir / ritonavir / dasabuvir. In rodent pre/postnatal developmental studies, maternal systemic exposures (AUC) to ombitasvir, paritaprevir and dasabuvir were approximately 25, 17 and 44 times, respectively, the exposure in humans at the recommended clinical dose.
- The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data (Animal)
Ombitasvir
- Ombitasvir was administered orally to pregnant mice (0, 15, 50, or 150 mg/kg/day) and rabbits (0, 10 or 60 mg/kg/day) during the period of organogenesis (on gestation days (GD) 6 to 15, and GD 7 to 19, respectively). There were no ombitasvir-related embryofetal effects (malformations or fetal toxicity) at any dose level in either species. The systemic exposures at the highest doses were 28-times higher (mice) and 4-times higher (rabbits) than the exposures in humans at the recommended clinical dose.
- In a pre- and postnatal developmental study in mice, ombitasvir was administered orally at 0, 10, 40, or 200 mg/kg/day from GD 6 to lactation day 20. There were no ombitasvir-related effects at maternal exposures 25-times higher than exposures in humans at the recommended clinical dose.
- The major human metabolites of ombitasvir, M29 and M36, were tested in pregnant mice during the period of organogenesis from GD 6 to 15. M29 was administered orally at doses of 0, 1, 2.5 or 4.5 mg/kg/day. M36 was dosed orally at doses 1.5, 3, or 6 mg/kg/day. In both cases, there were no treatment related embryofetal effects (malformations or fetal toxicity) at any dose level. The highest doses produced exposures approximately 26-times higher than the exposures in humans at the recommended clinical dose.
Paritaprevir/ritonavir
- Paritaprevir/ritonavir was administered orally to pregnant rats (0/0, 30/15, 100/15, 450/45 mg/kg/day) and mice (0/0, 30/30, 100/30, or 300/30 mg/kg/day) during the period of organogenesis (on GD 6 to 17, and GD 6 to 15, respectively). There were no test article-related embryofetal effects (malformations or fetal toxicity) at any dose level in either species. The highest systemic exposure of paritaprevir was 8-times higher (rats) and 98-times higher (mice) than the exposures in humans at the recommended clinical dose.
- In a pre- and postnatal developmental study in rats, paritaprevir/ritonavir were administered orally at 0/0, 6/30, 30/30, or 300/30 mg/kg/day from GD 7 to lactation day 20. There were no treatment related effects at maternal exposures 17-times higher than exposures in humans at the recommended clinical dose.
Dasabuvir
- Dasabuvir was administered orally to pregnant rats (0, 60, 300 and 800 mg/kg/day) and rabbits (0, 100, 200 or 400 mg/kg/day) during the period of organogenesis (on GD 6 to 17 and GD 7 to 20, respectively). There were no test article-related embryofetal effects (malformations or fetal toxicity) at any dose level in either species. The highest systemic exposure of dasabuvir was 24-times higher (rats) and 6-times higher (rabbits) than the exposures in humans at the recommended clinical dose.
- In a pre- and postnatal developmental study in rats, dasabuvir was administered orally at 0, 50, 200, or 800 mg/kg/day from GD 7 to lactation day 21. There were no treatment-related effects at maternal exposures 44-times higher than exposures in humans at the recommended clinical dose.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ombitasvir / paritaprevir / ritonavir / dasabuvir in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Ombitasvir / paritaprevir / ritonavir / dasabuvir during labor and delivery.
Nursing Mothers
Risk Summary
- It is not known whether ombitasvir / paritaprevir / ritonavir / dasabuvir and its metabolites are present in human breast milk, affect human milk production or have effects on the breastfed infant. Unchanged ombitasvir, paritaprevir and its hydrolysis product M13, and dasabuvir were the predominant components observed in the milk of lactating rats, without effect on nursing pups.
- The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for ombitasvir / paritaprevir / ritonavir / dasabuvir and any potential adverse effects on the breastfed child from ombitasvir / paritaprevir / ritonavir / dasabuvir or from the underlying maternal condition.
- If ombitasvir / paritaprevir / ritonavir / dasabuvir is administered with ribavirin, the nursing mother’s information for ribavirin also applies to this combination regimen. Refer to the ribavirin prescribing information for more information on use during lactation.
Data (Animal)
Ombitasvir
- No effects of ombitasvir on growth and postnatal development were observed in nursing pups at the highest dose tested (200 mg/kg/day) in mice. Maternal systemic exposure (AUC) to ombitasvir was approximately 25 times the exposure in humans at the recommended clinical dose. Although not measured directly, ombitasvir was likely present in the milk of lactating mice in this study, since systemic exposure was observed in nursing pups on post-natal day 21 (approximately 16% of maternal exposure).
- When ombitasvir was administered to lactating rats (5 mg/kg on post-partum day 10 to 11), milk exposure (AUC) was 4 times higher than that in plasma, with unchanged parent drug (91%) accounting for the majority of drug-related material in milk.
Paritaprevir/ritonavir
- No effects of paritaprevir/ritonavir on growth and postnatal development were observed in nursing pups at the highest dose tested (300/30 mg/kg/day) in rats. Maternal systemic exposure (AUC) to paritaprevir was approximately 17 times the exposure in humans at the recommended clinical dose. Although not measured directly, paritaprevir was likely present in the milk of lactating rats at the high dose in this study, since systemic exposure was observed in nursing pups on post-natal day 15 (approximately 0.3 % of maternal exposure).
- When paritaprevir/ritonavir was administered to lactating rats (30/15 mg/kg on post-partum day 10 to 11), milk exposure (AUC) was half that in plasma, with the hydrolysis product M13 (84%) and unchanged parent drug (16%) accounting for all paritaprevir-related material in milk.
Dasabuvir
- No effects of dasabuvir on growth and postnatal development were observed in nursing pups at the highest dose tested (800 mg/kg/day) in rats. Maternal systemic exposure (AUC) to dasabuvir was approximately 44 times the exposure in humans at the recommended clinical dose. Although not measured directly, dasabuvir was likely present in the milk of lactating rats in this study, since systemic exposure was observed in nursing pups on post-natal day 14 (approximately 14% of maternal exposure).
- When dasabuvir was administered to lactating rats (5 mg/kg on post-partum day 10 to 11), milk exposure (AUC) was 2 times higher than that in plasma, with unchanged parent drug (78%) accounting for the majority of drug-related material in milk.
Pediatric Use
- Safety and effectiveness of ombitasvir / paritaprevir / ritonavir / dasabuvir in pediatric patients less than 18 years of age have not been established.
Geriatic Use
- No dosage adjustment of ombitasvir / paritaprevir / ritonavir / dasabuvir is warranted in geriatric patients. Of the total number of subjects in clinical studies of ombitasvir / paritaprevir / ritonavir / dasabuvir, 8.5% (174/2053) were 65 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger subjects, but greater sensitivity of some older individuals cannot be ruled out.
Gender
There is no FDA guidance on the use of Ombitasvir / paritaprevir / ritonavir / dasabuvir with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ombitasvir / paritaprevir / ritonavir / dasabuvir with respect to specific racial populations.
Renal Impairment
- No dosage adjustment of ombitasvir / paritaprevir / ritonavir / dasabuvir is required in patients with mild, moderate or severe renal impairment, including those on dialysis. For patients that require ribavirin, refer to the ribavirin prescribing information for information regarding use in patients with renal impairment.
Hepatic Impairment
- No dosage adjustment of ombitasvir / paritaprevir / ritonavir / dasabuvir is required in patients with mild hepatic impairment (Child-Pugh A). Ombitasvir / paritaprevir / ritonavir / dasabuvir is contraindicated in patients with moderate to severe (Child-Pugh B and C) hepatic impairment.
Females of Reproductive Potential and Males
- If ombitasvir / paritaprevir / ritonavir / dasabuvir is administered with ribavirin, the information for ribavirin with regard to pregnancy testing, contraception, and infertility also applies to this combination regimen. Refer to ribavirin prescribing information for additional information.
Immunocompromised Patients
There is no FDA guidance one the use of Ombitasvir / paritaprevir / ritonavir / dasabuvir in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
- Hepatitis C genotype: Prior to initiation of therapy.
- Reduction from baseline in hepatitis C virus-RNA viral load may indicate efficacy.
- Hepatitis B virus (HBV) current or prior infection: Prior to use.
- Hepatic labs; prior to treatment, first 4 weeks of treatment, and as clinically indicated thereafter.
- Clinical and laboratory signs of hepatitis flare or HBV reactivation, in patients with evidence of current or priot HBV infection: During treatment and post-treatment follow-up.
- Signs or symptoms of hepatic decompensation, in patients with cirrhosis.
- Signs and symptoms of hypotension and worsening renal function: During concomitant therapy with angiotensin receptor blockers (eg, valsartan, losartan, candesartan).
- Signs and symptoms of hypotension and edema: During concomitant therapy with calcium channel blockers (eg, amlodipine, nifedipine, diltiazem, verapamil).
IV Compatibility
There is limited information regarding the compatibility of Ombitasvir / paritaprevir / ritonavir / dasabuvir and IV administrations.
Overdosage
- In case of overdose, it is recommended that the patient be monitored for any signs or symptoms of adverse reactions and appropriate symptomatic treatment instituted immediately.
Pharmacology
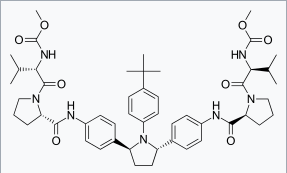
Ombitasvir
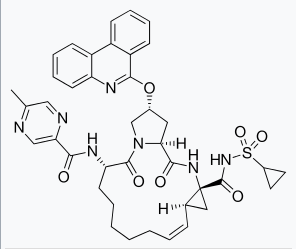
Paritaprevir
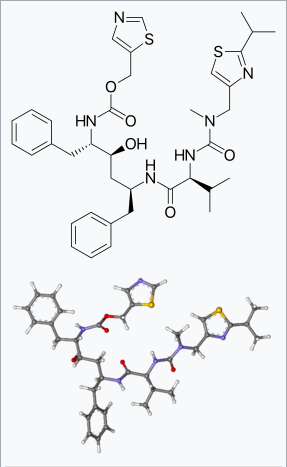
Dasabuvir
| |
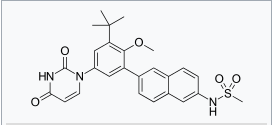
Ombitasvir / paritaprevir / ritonavir / dasabuvir
| |
| Systematic (IUPAC) name | |
| N-{6-[5-(2,4-Dioxo-3,4-dihydro-1(2H)-pyrimidinyl)-2-methoxy-3-(2-methyl-2-propanyl)phenyl]-2-naphthyl}methanesulfonamide | |
| Identifiers | |
| CAS number | |
| ATC code | J05 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 493.58 g/mol |
| SMILES | & |
| Synonyms | ABT-333 |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. |
B(US) |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | ? |
=
Mechanism of Action
- Ombitasvir / paritaprevir / ritonavir / dasabuvir combines three direct-acting hepatitis C virus antiviral agents with distinct mechanisms of action.
- Ritonavir is not active against HCV. Ritonavir is a potent CYP3A inhibitor that increases peak and trough plasma drug concentrations of paritaprevir and overall drug exposure (i.e., area under the curve).
Structure
Ombitasvir

Paritaprevir


Dasabuvir

Pharmacodynamics
Cardiac Electrophysiology
- The effect of a combination of ombitasvir, paritaprevir, ritonavir, and dasabuvir on QTc interval was evaluated in a randomized, double blind, placebo and active-controlled (moxifloxacin 400 mg) 4-way crossover thorough QT study in 60 healthy subjects. At concentrations approximately 6, 1.8 and 2 times the therapeutic concentrations of paritaprevir, ombitasvir, and dasabuvir, the combination did not prolong QTc to any clinically relevant extent.
Pharmacokinetics
- The pharmacokinetic properties of the components of ombitasvir / paritaprevir / ritonavir / dasabuvir are provided in TABLE 6. Based on the population pharmacokinetic analysis, the median steady-state pharmacokinetic parameters of ombitasvir, paritaprevir, ritonavir and dasabuvir in HCV‑infected subjects are provided in TABLE 7.


Specific Populations
Hepatic Impairment
- The single dose pharmacokinetics of ombitasvir, paritaprevir, ritonavir and dasabuvir were evaluated in non-HCV infected subjects with mild hepatic impairment (Child-Pugh Category A; score of 5-6), moderate hepatic impairment (Child-Pugh Category B, score of 7-9) and severe hepatic impairment (Child-Pugh Category C, score of 10-15).
- Relative to subjects with normal hepatic function, ombitasvir, paritaprevir and ritonavir AUC values decreased by 8%, 29% and 34%, respectively, and dasabuvir AUC values increased by 17% in subjects with mild hepatic impairment.
- Relative to subjects with normal hepatic function, ombitasvir, ritonavir and dasabuvir AUC values decreased by 30%, 30% and 16%, respectively, and paritaprevir AUC values increased by 62% in subjects with moderate hepatic impairment.
- Relative to subjects with normal hepatic function, paritaprevir, ritonavir and dasabuvir AUC values increased by 945%, 13%, and 325% respectively, and ombitasvir AUC values decreased by 54% in subjects with severe hepatic impairment.
Renal Impairment
- The single dose pharmacokinetics of ombitasvir, paritaprevir, ritonavir and dasabuvir were evaluated in non-HCV infected subjects with mild (CLcr: 60 to 89 mL/min), moderate (CLcr: 30 to 59 mL/min), and severe (CLcr: 15 to 29 mL/min) renal impairment.
- Overall, changes in exposure of ombitasvir, paritaprevir, ritonavir and dasabuvir in non-HCV infected subjects with mild-, moderate- and severe renal impairment are not expected to be clinically relevant. Pharmacokinetic data are not available on the use of ombitasvir / paritaprevir / ritonavir / dasabuvir in non-HCV infected subjects with End Stage Renal Disease (ESRD).
- Relative to subjects with normal renal function, paritaprevir, ritonavir and dasabuvir AUC values increased by 19%, 42% and 21%, respectively, while ombitasvir AUC values were unchanged in subjects with mild renal impairment.
- Relative to subjects with normal renal function, paritaprevir, ritonavir and dasabuvir AUC values increased by 33%, 80% and 37%, respectively, while ombitasvir AUC values were unchanged in subjects with moderate renal impairment.
- Relative to subjects with normal renal function, paritaprevir, ritonavir and dasabuvir AUC values increased by 45%, 114% and 50%, respectively, while ombitasvir AUC values were unchanged in subjects with severe renal impairment.
Pediatric Population
- The pharmacokinetics of ombitasvir / paritaprevir / ritonavir / dasabuvir in pediatric patients less than 18 years of age has not been established.
Sex
- No dose adjustment is recommended based on sex or body weight.
Race/Ethnicity
- No dose adjustment is recommended based on race or ethnicity.
Age
- No dose adjustment is recommended in geriatric patients.
Drug Interaction Studies
- The effects of drugs discussed in TABLE 5 on the exposures of the individual components of ombitasvir / paritaprevir / ritonavir / dasabuvir are shown in TABLE 8. For information regarding clinical recommendations.

- TABLE 9 summarizes the effects of ombitasvir / paritaprevir / ritonavir / dasabuvir on the pharmacokinetics of co-administered drugs which showed clinically relevant changes. For information regarding clinical recommendations.

Microbiology
Mechanism of Action
- Ombitasvir / paritaprevir / ritonavir / dasabuvir combines three direct-acting antiviral agents with distinct mechanisms of action and non-overlapping resistance profiles to target HCV at multiple steps in the viral lifecycle.
Ombitasvir
- Ombitasvir is an inhibitor of HCV NS5A, which is essential for viral RNA replication and virion assembly. The mechanism of action of ombitasvir has been characterized based on cell culture antiviral activity and drug resistance mapping studies.
Paritaprevir
- Paritaprevir is an inhibitor of the HCV NS3/4A protease which is necessary for the proteolytic cleavage of the HCV encoded polyprotein (into mature forms of the NS3, NS4A, NS4B, NS5A, and NS5B proteins) and is essential for viral replication. In a biochemical assay, paritaprevir inhibited the proteolytic activity of recombinant HCV genotype 1a and 1b NS3/4A protease enzymes with IC50 values of 0.18 nM and 0.43 nM, respectively.
Dasabuvir
- Dasabuvir is a non-nucleoside inhibitor of the HCV RNA-dependent RNA polymerase encoded by the NS5B gene, which is essential for replication of the viral genome. In a biochemical assay, dasabuvir inhibited a panel of genotype 1a and 1b NS5B polymerases with median IC50 values of 2.8 nM (range 2.4 nM to 4.2 nM; n = 3) and 3.7 nM (range 2.2 nM to 10.7 nM; n = 4), respectively. Based on drug resistance mapping studies of HCV genotypes 1a and 1b, dasabuvir targets the palm domain of the NS5B polymerase, and is therefore referred to as a non-nucleoside NS5B-palm polymerase inhibitor.
Antiviral Activity
Ombitasvir
- The EC50 values of ombitasvir against genotype 1a-H77 and 1b-Con1 strains in HCV replicon cell culture assays were 14.1 pM and 5 pM, respectively. The median EC50 values of ombitasvir against HCV replicons containing NS5A genes from a panel of genotype 1a and 1b isolates from treatment-naïve subjects were 0.68 pM (range 0.35 to 0.88 pM; n = 11) and 0.94 pM (range 0.74 to 1.5 pM; n = 11), respectively.
Paritaprevir
- The EC50 values of paritaprevir against genotype 1a-H77 and 1b-Con1 strains in the HCV replicon cell culture assay were 1.0 nM and 0.21 nM, respectively. The median EC50 values of paritaprevir against HCV replicons containing NS3 genes from a panel of genotype 1a and 1b isolates from treatment-naïve subjects were 0.68 nM (range 0.43 nM to 1.87 nM; n = 11) and 0.06 nM (range 0.03 nM to 0.09 nM; n = 9), respectively.
Ritonavir
- In HCV replicon cell culture assays, ritonavir did not exhibit a direct antiviral effect and the presence of ritonavir did not affect the antiviral activity of paritaprevir.
Dasabuvir
- The EC50 values of dasabuvir against genotype 1a-H77 and 1b-Con1 strains in HCV replicon cell culture assays were 7.7 nM and 1.8 nM, respectively. The median EC50 values of dasabuvir against HCV replicons containing NS5B genes from a panel of genotype 1a and 1b isolates from treatment-naïve subjects were 0.6 nM (range 0.4 nM to 2.1 nM; n = 11) and 0.3 nM (range 0.2 nM to 2 nM; n = 10), respectively.
Combination Antiviral Activity
- Evaluation of pairwise combinations of ombitasvir, paritaprevir, dasabuvir and ribavirin in HCV genotype 1 replicon cell culture assays showed no evidence of antagonism in antiviral activity.
Resistance
In Cell Culture
- Exposure of HCV genotype 1a and 1b replicons to ombitasvir, paritaprevir or dasabuvir resulted in the emergence of drug resistant replicons carrying amino acid substitutions in NS5A, NS3, or NS5B, respectively. Amino acid substitutions in NS5A, NS3, or NS5B selected in cell culture or identified in Phase 2b and 3 clinical trials were phenotypically characterized in genotype 1a or 1b replicons.
- For ombitasvir, in HCV genotype 1a replicons single NS5A substitutions M28T/V, Q30E/R, L31V, H58D, and Y93C/H/L/N reduced ombitasvir antiviral activity by 58- to 67,000-fold. In genotype 1b replicons, single NS5A substitutions L28T, L31F/V, and Y93H reduced ombitasvir antiviral activity by 8- to 661-fold. In general, combinations of ombitasvir resistance-associated substitutions in HCV genotype 1a or 1b replicons further reduced ombitasvir antiviral activity.
- For paritaprevir, in HCV genotype 1a replicons single NS3 substitutions F43L, R155G/K/S, A156T, and D168A/E/F/H/N/V/Y reduced paritaprevir antiviral activity by 7- to 219-fold. An NS3 Q80K substitution in a genotype 1a replicon reduced paritaprevir antiviral activity by 3-fold. Combinations of V36M, Y56H, or E357K with R155K or D168 substitutions reduced the activity of paritaprevir by an additional 2- to 7-fold relative to the single R155K or D168 substitutions in genotype 1a replicons. In genotype 1b replicons single NS3 substitutions A156T and D168A/H/V reduced paritaprevir antiviral activity by 7- to 159-fold. The combination of Y56H with D168 substitutions reduced the activity of paritaprevir by an additional 16- to 26-fold relative to the single D168 substitutions in genotype 1b replicons.
- For dasabuvir, in HCV genotype 1a replicons single NS5B substitutions C316Y, M414I/T, E446K/Q, Y448C/H, A553T, G554S, S556G/R, and Y561H reduced dasabuvir antiviral activity by 8- to 1,472-fold. In genotype 1b replicons, single NS5B substitutions C316H/N/Y, S368T, N411S, M414I/T, Y448C/H, A553V, S556G and D559G reduced dasabuvir antiviral activity by 5- to 1,569-fold.
In Clinical Studies
- In a pooled analysis of subjects treated with regimens containing ombitasvir, paritaprevir, and dasabuvir with or without ribavirin (for 12 or 24 weeks) in Phase 2b and Phase 3 clinical trials, resistance analyses were conducted for 64 subjects who experienced virologic failure (20 with on-treatment virologic failure, 44 with post-treatment relapse). Treatment-emergent substitutions observed in the viral populations of these subjects are shown in TABLE 10. Treatment-emergent substitutions were detected in all 3 HCV drug targets in 30/57 (53%) HCV genotype 1a infected subjects, and 1/6 (17%) HCV genotype 1b infected subjects.

Persistence of Resistance-Associated Substitutions
- The persistence of ombitasvir, paritaprevir, and dasabuvir treatment-emergent amino acid substitutions in NS5A, NS3, and NS5B, respectively, was assessed in HCV genotype 1a-infected subjects in Phase 2 trials whose virus had at least 1 treatment-emergent resistance-associated substitution in the drug target, and with available data through at least 24 weeks post-treatment. Population and clonal nucleotide sequence analyses (assay sensitivity approximately 5-10%) were conducted to detect the persistence of viral populations with treatment-emergent substitutions.
- For ombitasvir, viral populations with 1 or more resistance-associated treatment-emergent substitutions in NS5A persisted at detectable levels through at least Post-Treatment Week 24 in 24/24 (100%) subjects, and through Post-Treatment Week 48 in 18/18 (100%) subjects with available data.
- For paritaprevir, viral populations with 1 or more treatment-emergent substitutions in NS3 persisted at detectable levels through at least Post-Treatment Week 24 in 17/29 (59%) subjects, and through Post-Treatment Week 48 in 5/22 (23%) subjects with available data. Resistance-associated variant R155K remained detectable in 5/8 (63%) subjects through Post-Treatment Week 24, and in 1/5 (20%) subjects through Post-Treatment Week 48. Resistance-associated D168 substitutions remained detectable in 6/22 (27%) subjects through Post-Treatment Week 24, and were no longer detectable through Post-Treatment Week 48.
- For dasabuvir, viral populations with 1 or more treatment-emergent substitutions in NS5B persisted at detectable levels through at least Post-Treatment Week 24 in 11/16 (69%) subjects, and through Post-Treatment Week 48 in 8/15 (53%) subjects with available data. Treatment-emergent S556G persisted through Post-Treatment Week 48 in 6/9 (67%) subjects.
- Among HCV genotype 1b infected subjects who experienced virologic failure with a regimen including ombitasvir and paritaprevir, a treatment-emergent NS5A Y93H substitution persisted through at least Post-Treatment Week 48 in 2/2 subjects, and a NS3 D168V treatment-emergent substitution persisted through Post-Treatment Week 24 in 2/4 subjects, but was no longer detectable through Post-Treatment Week 48 (0/4 subjects).
- The lack of detection of virus containing a resistance-associated substitution does not indicate that the resistant virus is no longer present at clinically significant levels. The long-term clinical impact of the emergence or persistence of virus containing ombitasvir / paritaprevir / ritonavir / dasabuvir-resistance-associated substitutions is unknown.
Effect of Baseline HCV Polymorphisms on Treatment Response
- A pooled analysis of subjects in the Phase 3 clinical trials of ombitasvir, paritaprevir, and dasabuvir with or without ribavirin was conducted to explore the association between baseline HCV NS5A, NS3, or NS5B resistance-associated polymorphisms and treatment outcome. Baseline samples from HCV genotype 1a infected subjects who experienced virologic failure (n=47), as well as samples from a subset of demographically matched subjects who achieved SVR (n=94), were analyzed to compare the frequencies of resistance-associated polymorphisms in these two populations. The NS3 Q80K polymorphism was detected in approximately 38% of subjects in this analysis and was enriched approximately 2-fold in virologic failure subjects compared to SVR-achieving subjects. Ombitasvir resistance-associated polymorphisms in NS5A (pooling data from all resistance-associated amino acid positions) were detected in approximately 22% of subjects in this analysis and similarly were enriched approximately 2-fold in virologic failure subjects. Dasabuvir resistance-associated polymorphisms in NS5B were detected in approximately 5% of subjects in this analysis and were not enriched in virologic failure subjects.
- In contrast to the Phase 3 subset analysis, no association of NS3 or NS5A polymorphisms and treatment outcome was seen in an analysis of noncirrhotic HCV genotype 1a-infected subjects (n=174 for NS3 and n=183 for NS5A) who received ombitasvir, paritaprevir, and dasabuvir with or without ribavirin (for 12 or 24 weeks) in a Phase 2b trial.
- Baseline HCV polymorphisms are not expected to have a substantial impact on the likelihood of achieving SVR when ombitasvir / paritaprevir / ritonavir / dasabuvir is used as recommended for HCV genotype 1a and 1b infected patients, based on the low virologic failure rates observed in clinical trials.
Cross-resistance
- Cross-resistance is expected among NS5A inhibitors, NS3/4A protease inhibitors, and non-nucleoside NS5B-palm inhibitors by class. Dasabuvir retained full activity against HCV replicons containing a single NS5B L159F, S282T, or V321A substitution, which are associated with resistance or prior exposure to nucleos(t)ide analogue NS5B polymerase inhibitors. In clinical trials of ombitasvir / paritaprevir / ritonavir / dasabuvir, no subjects who experienced virologic failure had treatment-emergent substitutions potentially associated with resistance to nucleos(t)ide analogue NS5B polymerase inhibitors.
- The impact of prior ombitasvir, paritaprevir, or dasabuvir treatment experience on the efficacy of other NS5A inhibitors, NS3/4A protease inhibitors, or NS5B inhibitors has not been studied. Similarly, the efficacy of ombitasvir / paritaprevir / ritonavir / dasabuvir has not been studied in subjects who have failed prior treatment with another NS5A inhibitor, NS3/4A protease inhibitor, or NS5B inhibitor.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis
Ombitasvir
- Ombitasvir was not carcinogenic in a 6-month transgenic mouse study up to the highest dose tested (150 mg per kg per day). Similarly, ombitasvir was not carcinogenic in a 2-year rat study up to the highest dose tested (30 mg per kg per day), resulting in ombitasvir exposures approximately 16-fold higher than those in humans at 25 mg.
- Ombitasvir and its major inactive human metabolites (M29, M36) were not genotoxic in a battery of in vitro or in vivo assays, including bacterial mutagenicity, chromosome aberration using human peripheral blood lymphocytes and in vivo mouse micronucleus assays.
Paritaprevir, ritonavir
- Paritaprevir, ritonavir was not carcinogenic in a 6-month transgenic mouse study up to the highest dose tested (300/30 mg per kg per day). Similarly, paritaprevir, ritonavir was not carcinogenic in a 2-year rat study up to the highest dose tested (300/30 mg per kg per day), resulting in paritaprevir exposures approximately 9-fold higher than those in humans at 150 mg.
- Paritaprevir was positive in an in vitro chromosome aberration test using human lymphocytes. Paritaprevir was negative in a bacterial mutation assay, and in two in vivo genetic toxicology assays (rat bone marrow micronucleus and rat liver Comet tests).
Dasabuvir
- Dasabuvir was not carcinogenic in a 6-month transgenic mouse study up to the highest dose tested (2000 mg per kg per day). Similarly, dasabuvir was not carcinogenic in a 2-year rat study up to the highest dose tested (800 mg per kg per day), resulting in dasabuvir exposures approximately 19-fold higher than those in humans at 500 mg.
- Dasabuvir was not genotoxic in a battery of in vitro or in vivo assays, including bacterial mutagenicity, chromosome aberration using human peripheral blood lymphocytes and in vivo rat micronucleus assays.
- If ombitasvir / paritaprevir / ritonavir / dasabuvir is administered with ribavirin, refer to the prescribing information for ribavirin for information on carcinogenesis, and mutagenesis.
Impairment of Fertility
Ombitasvir
- Ombitasvir had no effects on embryo-fetal viability or on fertility when evaluated in mice up to the highest dose of 200 mg per kg per day. Ombitasvir exposures at this dose were approximately 25-fold the exposure in humans at the recommended clinical dose.
Paritaprevir, ritonavir
- Paritaprevir, ritonavir had no effects on embryo-fetal viability or on fertility when evaluated in rats up to the highest dose of 300/30 mg per kg per day. Paritaprevir exposures at this dose were approximately 2- to 5-fold the exposure in humans at the recommended clinical dose.
Dasabuvir
- Dasabuvir had no effects on embryo-fetal viability or on fertility when evaluated in rats up to the highest dose of 800 mg per kg per day. Dasabuvir exposures at this dose were approximately 16-fold the exposure in humans at the recommended clinical dose.
- If ombitasvir / paritaprevir / ritonavir / dasabuvir is administered with ribavirin, refer to the prescribing information for ribavirin for information on Impairment of Fertility.
Clinical Studies
Description of Clinical Trials
- TABLE 11 presents the clinical trial design including different treatment arms that were conducted with ombitasvir / paritaprevir / ritonavir / dasabuvir with or without ribavirin in subjects with chronic hepatitis C (HCV) genotype 1 (GT1) infection. For detailed description of trial design and recommended regimen and duration.

- Ombitasvir / paritaprevir / ritonavir / dasabuvir with RBV was also evaluated in the following two studies:
- HCV GT1-infected liver transplant recipients (CORAL-I).
- Subjects with HCV GT1 co-infected with HIV-1 (TURQUOISE-I).
- In all clinical trials, the ombitasvir, paritaprevir, ritonavir dose was 25/150/100 mg once daily and the dasabuvir dose was 250 mg twice daily. Doses of drugs in ombitasvir / paritaprevir / ritonavir / dasabuvir were not adjusted. For subjects who received RBV, the RBV dose was 1000 mg per day for subjects weighing less than 75 kg or 1200 mg per day for subjects weighing greater than or equal to 75 kg. RBV dose adjustments were performed according to the RBV labeling.
- In all clinical trials, sustained virologic response was defined as HCV RNA below the lower limit of quantification (<LLOQ) 12 weeks after the end of treatment (SVR12). Plasma HCV RNA levels were measured using the COBAS TaqMan HCV test (version 2.0), for use with the High Pure System, which has an LLOQ of 25 IU per mL. Outcomes for subjects not achieving an SVR12 were recorded as on-treatment virologic failure (VF), post-treatment virologic relapse through post-treatment Week 12 or failure due to other non-virologic reasons (e.g., premature discontinuation, adverse event, lost to follow-up, consent withdrawn).
Clinical Trial Results in Adults with Chronic HCV Genotype 1a and 1b Infection without Cirrhosis
Subjects with Chronic HCV GT1a Infection without Cirrhosis
- Subjects with HCV GT1a infection without cirrhosis treated with ombitasvir / paritaprevir / ritonavir / dasabuvir with RBV for 12 weeks in SAPPHIRE-I and -II and in PEARL-IV had a median age of 53 years (range: 18 to 70); 63% of the subjects were male; 90% were White; 7% were Black/African American; 8% were Hispanic or Latino; 19% had a body mass index of at least 30 kg per m2; 55% of patients were enrolled in US sites; 72% had IL28B (rs12979860) non-CC genotype; 85% had baseline HCV RNA levels of at least 800,000 IU per mL.
- TABLE 12 presents treatment outcomes for HCV GT1a treatment-naïve and treatment-experienced subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir with RBV for 12 weeks in SAPPHIRE-I, PEARL-IV and SAPPHIRE-II.
- Treatment-naïve, HCV GT1a-infected subjects without cirrhosis treated with ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with RBV for 12 weeks in PEARL-IV had a significantly higher SVR12 rate than subjects treated with ombitasvir / paritaprevir / ritonavir / dasabuvir alone (97% and 90% respectively; difference +7% with 95% confidence interval, +1% to +12%). Ombitasvir / paritaprevir / ritonavir / dasabuvir alone was not studied in treatment-experienced subjects with GT1a infection.
- In SAPPHIRE-I and SAPPHIRE-II, no placebo subject achieved a HCV RNA <25 IU/mL during treatment.

Subjects with Chronic HCV GT1b Infection without Cirrhosis
- Subjects with HCV GT1b infection without cirrhosis were treated with ombitasvir / paritaprevir / ritonavir / dasabuvir with or without RBV for 12 weeks in PEARL-II and -III. Subjects had a median age of 52 years (range: 22 to 70); 47% of the subjects were male; 93% were White; 5% were Black/African American; 2% were Hispanic or Latino; 21% had a body mass index of at least 30 kg per m2; 21% of patients were enrolled in US sites; 83% had IL28B (rs12979860) non-CC genotype; 77% had baseline HCV RNA levels of at least 800,000 IU per mL.
- The SVR rate for HCV GT1b-infected subjects without cirrhosis treated with ombitasvir / paritaprevir / ritonavir / dasabuvir without RBV for 12 weeks in PEARL-II (treatment-experienced: null responder, n=32; partial responder, n=26; relapser, n=33) and PEARL-III (treatment-naïve, n=209) was 100%.
Clinical Trial Results in Adults with Chronic HCV Genotype 1a and 1b Infection and Compensated Cirrhosis
- Ombitasvir / paritaprevir / ritonavir / dasabuvir with and without ribavirin was evaluated in two clinical trials in patients with compensated cirrhosis.
- TURQUOISE-II was an open-label trial that enrolled 380 HCV GT1-infected subjects with cirrhosis and mild hepatic impairment (Child-Pugh A) who were either treatment-naïve or did not achieve SVR with prior treatment with pegIFN/RBV. Subjects were randomized to receive ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with RBV for either 12 or 24 weeks of treatment. Treated subjects had a median age of 58 years (range: 21 to 71); 70% of the subjects were male; 95% were White; 3% were Black/African American; 12% were Hispanic or Latino; 28% had a body mass index of at least 30 kg per m2; 43% of patients were enrolled in US sites; 82% had IL28B (rs12979860) non‑CC genotype; 86% had baseline HCV RNA levels of at least 800,000 IU per mL; 69% had HCV GT1a infection, 31% had HCV GT1b infection; 42% were treatment-naïve, 36% were prior pegIFN/RBV null responders; 8% were prior pegIFN/RBV partial responders, 14% were prior pegIFN/RBV relapsers; 15% had platelet counts of less than 90 x 109 per L; 50% had albumin less than 4.0 mg per dL.
- TURQUOISE-III was an open-label trial that enrolled 60 HCV GT1b-infected subjects with cirrhosis and mild hepatic impairment (Child-Pugh A) who were either treatment-naïve or did not achieve SVR with prior treatment with pegIFN/RBV. Subjects received ombitasvir / paritaprevir / ritonavir / dasabuvir without RBV for 12 weeks. Treated subjects had a median age of 61 years (range: 26 to 78); including 45% treatment-naïve and 55% pegIFN/RBV treatment-experienced; 25% were ≥65 years; 62% were male; 12% were Black; 5% were Hispanic or Latino; 28% had a body mass index of at least 30 kg per m2; 40% of patients were enrolled in US sites; 22% had platelet counts of less than 90 x 109 per L; 17% had albumin less than 35 g/L; 92% had baseline HCV RNA levels of at least 800,000 IU per mL; 83% had IL28B (rs12979860) non‑CC genotype.
- TABLE 13 presents treatment outcomes for GT1a- and GT1b-infected treatment-naïve and treatment-experienced subjects. In GT1a infected subjects, the overall SVR12 rate difference between 24 and 12 weeks of treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir with RBV was +6% with 95% confidence interval, -0.1% to +13% with differences varying by pretreatment history.

Effect of Ribavirin Dose Reductions on SVR12
- Seven percent of subjects (101/1551) treated with ombitasvir / paritaprevir / ritonavir / dasabuvir with RBV had a RBV dose adjustment due to a decrease in hemoglobin level; of these, 98% (98/100) achieved an SVR12.
Clinical Trial of Selected Liver Transplant Recipients (CORAL-I)
- Ombitasvir / paritaprevir / ritonavir / dasabuvir with RBV was administered for 24 weeks to 34 HCV GT1-infected liver transplant recipients who were at least 12 months post transplantation at enrollment with normal hepatic function and mild fibrosis (Metavir fibrosis score F2 or lower). The initial dose of RBV was left to the discretion of the investigator with 600 to 800 mg per day being the most frequently selected dose range at initiation of ombitasvir / paritaprevir / ritonavir / dasabuvir and at the end of treatment.
- Of the 34 subjects (29 with HCV GT1a infection and 5 with HCV GT1b infection) enrolled, (97%) achieved SVR12 (97% in subjects with GT1a infection and 100% of subjects with GT1b infection). One subject with HCV GT1a infection relapsed post-treatment.
Clinical Trial in Subjects with HCV/HIV-1 Co-infection (TURQUOISE-I)
- In an open-label clinical trial 63 subjects with HCV GT1 infection co-infected with HIV-1 were treated for 12 or 24 weeks with ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with RBV. Subjects were on a stable HIV-1 antiretroviral therapy (ART) regimen that included tenofovir disoproxil fumarate plus emtricitabine or lamivudine, administered with ritonavir boosted atazanavir or raltegravir. Subjects on atazanavir stopped the ritonavir component of their HIV-1 ART regimen upon initiating treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir in combination with RBV. Atazanavir was taken with the morning dose of ombitasvir / paritaprevir / ritonavir / dasabuvir. The ritonavir component of the HIV-1 ART regimen was restarted after completion of treatment with ombitasvir / paritaprevir / ritonavir / dasabuvir and RBV.
- Treated subjects had a median age of 51 years (range: 31 to 69); 24% of subjects were black; 81% of subjects had IL28B (rs12979860) non-CC genotype; 19% of subjects had compensated cirrhosis; 67% of subjects were HCV treatment-naïve; 33% of subjects had failed prior treatment with pegIFN/RBV; 89% of subjects had HCV genotype 1a infection.
- The SVR12 rates were 91% (51/56) for subjects with HCV GT1a infection and 100% (7/7) for those with HCV GT1b infection. Of the 5 subjects who were non-responders, 1 experienced virologic breakthrough, 1 discontinued treatment, 1 experienced relapse and 2 subjects had evidence of HCV re-infection post-treatment.
- One subject had confirmed HIV-1 RNA >400 copies/mL during the post-treatment period. This subject had no evidence of resistance to the ART regimen. No subjects switched their ART regimen due to loss of plasma HIV-1 RNA suppression.
Durability of Response
- In an open-label clinical trial, 92% of subjects (526/571) who received various combinations of the direct acting antivirals included in ombitasvir / paritaprevir / ritonavir / dasabuvir with or without RBV achieved SVR12, and 99% of those who achieved SVR12 maintained their response through 48 weeks post-treatment (SVR48).
How Supplied
- Ombitasvir / paritaprevir / ritonavir / dasabuvir is dispensed in a monthly carton for a total of 28 days of therapy. Each monthly carton contains four weekly cartons. Each weekly carton contains seven daily dose packs.
- Each child resistant daily dose pack contains four tablets: two 12.5/75/50 mg ombitasvir, paritaprevir, ritonavir tablets and two 250 mg dasabuvir tablets, and indicates which tablets need to be taken in the morning and evening. The NDC number is 0074-3093-28.
- Ombitasvir, paritaprevir, ritonavir 12.5/75/50 mg tablets are pink-colored, film-coated, oblong biconvex shaped, debossed with “AV1” on one side. Dasabuvir 250 mg tablets are beige-colored, film-coated, oval-shaped, debossed with “AV2” on one side.
Storage
- Store at or below 30°C (86°F).
Images
Drug Images
{{#ask: Page Name::Ombitasvir / paritaprevir / ritonavir / dasabuvir |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel


{{#ask: Label Page::Ombitasvir / paritaprevir / ritonavir / dasabuvir |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling.
- Inform patients to review the Medication Guide for ribavirin.
Risk of Hepatitis B Virus Reactivation in Patients Coinfected with HCV and HBV
- Inform patients that HBV reactivation can occur in patients coinfected with HBV during or after treatment of HCV infection. Advise patients to tell their healthcare provider if they have a history of hepatitis B virus infection.
Risk of ALT Elevations or Hepatic Decompensation and Failure
- Inform patients to watch for early warning signs of liver inflammation or failure, such as fatigue, weakness, lack of appetite, nausea and vomiting, as well as later signs such as jaundice, onset of confusion, abdominal swelling, and discolored feces, and to consult their health care professional without delay if such symptoms occur.
Pregnancy
- Advise patients taking ombitasvir / paritaprevir / ritonavir / dasabuvir with ribavirin to avoid pregnancy during treatment and within 6 months of stopping ribavirin. Inform patients to notify their health care provider immediately in the event of a pregnancy.
Drug Interactions
- Inform patients that ombitasvir / paritaprevir / ritonavir / dasabuvir may interact with some drugs; therefore, patients should be advised to report to their healthcare provider the use of any prescription, non-prescription medication or herbal products.
- Inform patients that contraceptives containing ethinyl estradiol are contraindicated with ombitasvir / paritaprevir / ritonavir / dasabuvir.
Administration
- Advise patients to take ombitasvir / paritaprevir / ritonavir / dasabuvir every day at the regularly scheduled time with a meal without regard to fat or calorie content.
- Inform patients that it is important not to miss or skip doses and to take ombitasvir / paritaprevir / ritonavir / dasabuvir for the duration that is recommended by the healthcare provider.

Precautions with Alcohol
Alcohol-Ombitasvir / paritaprevir / ritonavir / dasabuvir interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Viekira Pak
Look-Alike Drug Names
There is limited information regarding Ombitasvir / paritaprevir / ritonavir / dasabuvir Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.