Ethambutol
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Deepika Beereddy, MBBS [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Ethambutol is an anti- infective agent, antibacterial agent that is FDA approved for the treatment of pulmonary tuberculosis as an adjunct. Common adverse reactions include hyperuricemia, nausea, vomiting, mania.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Pulmonary tuberculosis; Adjunct
- Dosing Information
- MYAMBUTOL should not be used alone, in initial treatment or in retreatment. MYAMBUTOL should be administered on a once every 24-hour basis only. Absorption is not significantly altered by administration with food. Therapy, in general, should be continued until bacteriological conversion has become permanent and maximal clinical improvement has occured.
- MYAMBUTOL is not recommended for use in pediatric patients under thirteen years of age since safe conditions for use have not been established.
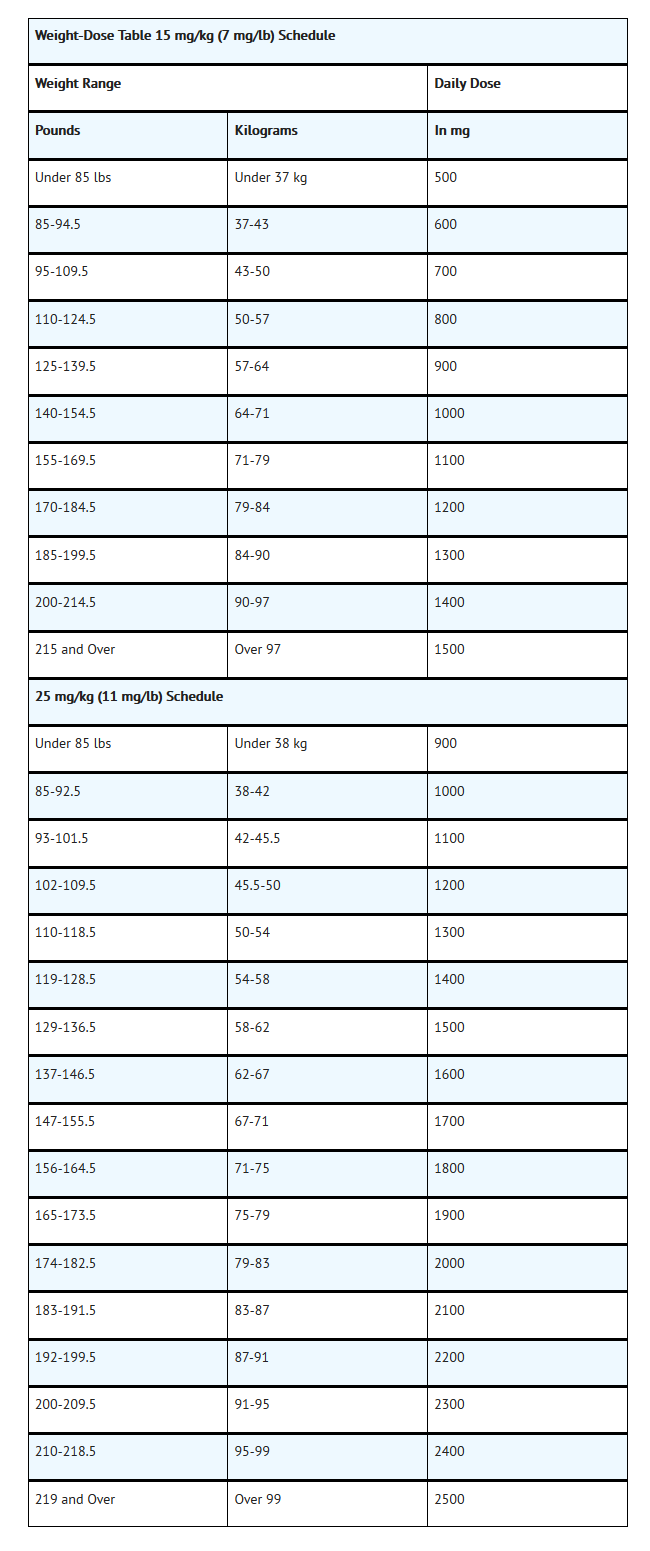
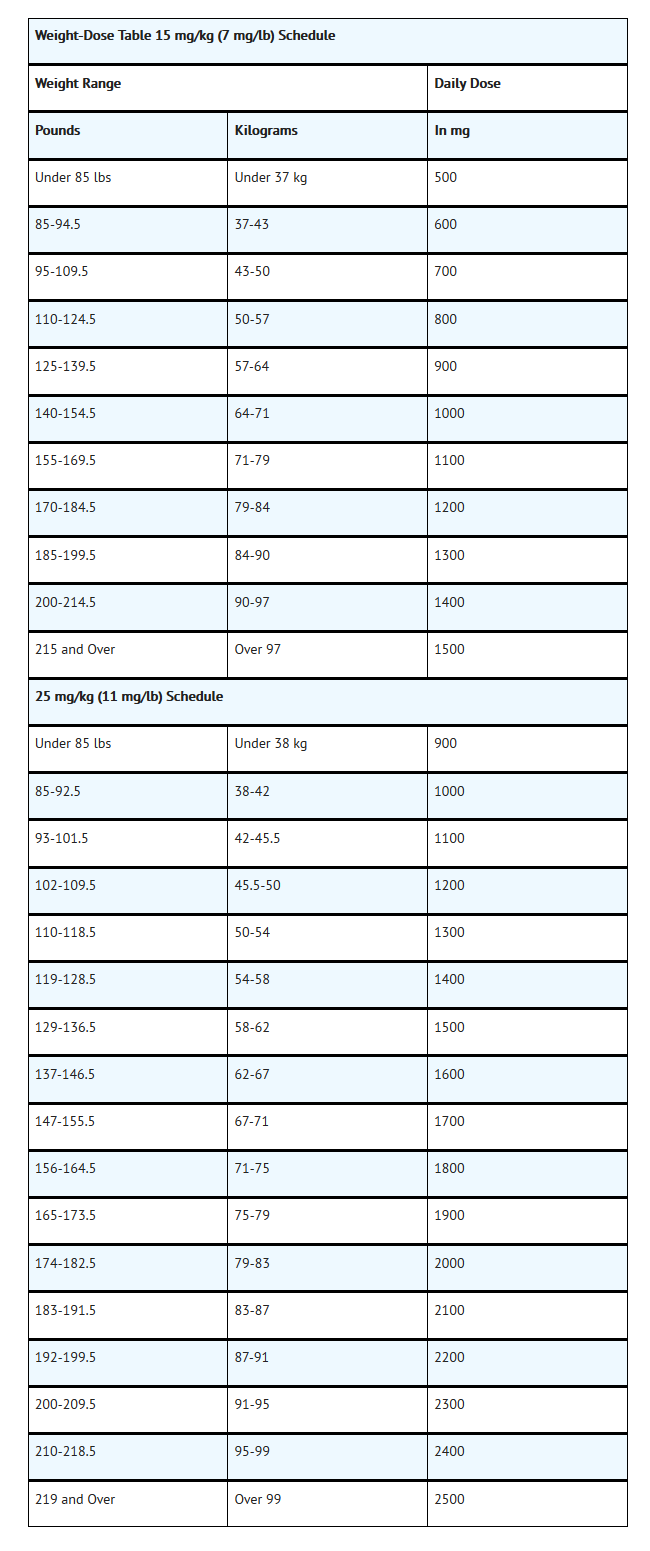
- Initial Treatment: In patients who have not received previous antituberculous therapy, administer MYAMBUTOL 15 mg/kg (7 mg/lb) of body weight, as a single oral dose once every 24 hours. In the more recent studies, isoniazid has been administered concurrently in a single, daily, oral dose.
- Retreatment: In patients who have received previous antituberculous therapyadminister MYAMBUTOL 25 mg/kg (11mg/lb) of body weight, as a single oral dose once every 24 hours. Concurrently administer at least one other antituberculous drug to which the organisms have been demonstrated to be susceptible by appropriate in vitro tests. Suitable drugs usually consist of those not previously used in the treatment of the patient. After 60 days of MYAMBUTOL administration, decrease the dose to 15 mg/kg (7 mg/lb) of body weight, and administer as a single oral dose once every 24 hours.
- During the period when patient is on a daily dose of 25 mg/kg, monthly eye examinations are advised.
- See Table for easy selection of proper weight-dose tablet(s).
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Disseminated infection due to Mycobacterium avium-intracellulare group; Prophylaxis - HIV infection
- Dosing information:
- Guideline Recommendations:
- Secondary Prevention:
- The recommended dose of ethambutol for the prevention of recurrence (secondary prophylaxis) of disseminated Mycobacterium avium complex disease in HIV-infected patients is 15 mg/kg orally daily in combination with clarithromycin 500 mg orally twice daily (or azithromycin 500 to 600 mg orally daily as an alternative), with or without rifabutin 300 mg orally daily.
- Secondary prophylaxis is indicated as lifelong therapy for individuals with documented disseminated disease. However, discontinuation of secondary prophylaxis may be considered in individuals who have completed at least 12 months of therapy, remained asymptomatic with respect to mycobacterial infection signs and symptoms, and have responded to HAART with a sustained CD4 count greater than 100/mcL for at least 6 months. Secondary prophylaxis should include a combination of clarithromycin (or azithromycin as an alternative choice) plus ethambutol with the possible addition of rifabutin.
Disseminated infection due to Mycobacterium avium-intracellulare group - HIV infection
- Dosing information:
- Guideline Recommendations:
- The recommended dose of ethambutol for the treatment of disseminated Mycobacterium avium complex disease in HIV-infected patients is 15 mg/kg orally daily in combination with clarithromycin 500 mg orally twice daily (or azithromycin 500 to 600 mg orally daily as an alternative), with or without rifabutin 300 mg orally daily.
HIV infection - Tuberculosis
- Dosing information:
- The Centers for Disease Control and Prevention (CDC), in association with the American Thoracic Society and the Infectious Diseases Society of America, recommends a 6-month treatment regimen for tuberculosis in HIV-infected patients on antiretroviral therapy. The treatment regimen consists of a 2-month initial phase of isoniazid, rifampin, pyrazinamide, and ethambutol, followed by a continuation phase of 4 to 7 months. For patients on directly observed therapy (DOT), 5 day-a-week dosing may be used to replace 7 day-a-week dosing (AIII). Rifabutin, which has fewer problematic drug interactions, may be used interchangeably with rifampin; dose adjustments to rifabutin and antiretroviral agents may be necessary. Ethambutol may be excluded if drug susceptibility results indicate that the organisms are fully susceptible to isoniazid and rifampin. If pyrazinamide cannot be included in the initial phase due to conditions such as severe liver disease, gout, or pregnancy, the initial phase should consist of isoniazid, rifampin, and ethambutol given once daily for 2 months. If isoniazid cannot be used, a 6-month regimen of rifampin, pyrazinamide, and ethambutol may be substituted (BI). If rifampin cannot be used, treatment with isoniazid and ethambutol for 12 to 18 months, with pyrazinamide during at least the initial phase is recommended. Completion of treatment should be determined by the total number of doses taken, and not solely on duration of therapy. The following is a list of 4 different regimens of initial and continuation phases that may be used for the treatment of tuberculosis in HIV-infected patients. Strength of recommendation and quality of evidence ratings are included at the end of this protocol.
- Regimen 1
- Initial Phase:
- Isoniazid, rifampin, pyrazinamide, and ethambutol administered once daily for 56 doses/8 weeks (AII), OR
- Isoniazid, rifampin, pyrazinamide, and ethambutol administered once daily for 5 days/week for 40 doses/8 weeks (AIII)
- Continuation Phase:
- Isoniazid and rifampin administered once daily for 126 doses/18 weeks (AII), OR
- Isoniazid and rifampin administered once daily for 5 days/week for 90 doses/18 weeks (AIII), OR
- Isoniazid and rifampin administered twice weekly for 36 doses/18 weeks (AII) (not recommended in HIV-infected patients with CD4+ counts less than 100 cells/milliliter)
- Regimen 2 (not recommended in HIV-infected patients with CD4+ counts less than 100 cells/milliliter)
- Initial Phase:
- Isoniazid, rifampin, pyrazinamide, and ethambutol administered once daily for at least the first 14 doses/2 weeks, followed by twice weekly dosing for 12 doses/6 weeks (BII), OR
- Isoniazid, rifampin, pyrazinamide, and ethambutol administered once daily for 5 days/week for 10 doses/2 weeks (AIII), followed by twice weekly dosing for 12 doses/6 weeks (BII)
- Continuation Phase:
- Isoniazid and rifampin administered twice weekly for 36 doses/18 weeks (BII)
- Regimen 3
- Initial Phase:
- Isoniazid, rifampin, pyrazinamide, and ethambutol administered 3 times weekly for 24 doses/8 weeks (BII)
- Continuation Phase:
- Isoniazid and rifampin administered 3 times weekly for 54 doses/18 weeks (BII)
- Regimen 4Initial Phase:
- Isoniazid, rifampin, and ethambutol administered once daily for 56 doses/8 weeks (CII), OR
- Isoniazid, rifampin, and ethambutol administered once daily for 5 days/week for 40 doses/8 weeks (AIII)
- Continuation Phase:Isoniazid and rifampin administered once daily for 217 doses/31 weeks (CII), OR
- Isoniazid and rifampin administered once daily for 5 days/week for 155 doses/31 weeks (AIII), OR
- Isoniazid and rifampin administered twice weekly for 62 doses/31 weeks (CII)
Mycobacterium avium complex infection, Lung disease
- Dosing information:
- Guideline Recommendations:
- Nodular/Bronchiectatic Disease:
- An intermittent regimen including ethambutol (25 mg/kg orally), rifampin (600 mg orally), and a macrolide (azithromycin 500 to 600 mg orally OR clarithromycin 1000 mg orally), administered 3 times a week, is recommended as initial therapy for patients with nodular/bronchiectatic disease, patients with a goal of disease suppression only, or fibrocavitary patients unable to tolerate daily therapy. The 3 times a week dosing regimen is not recommended for patients with severe or previously treated disease.
- Cavitary Disease:
- A daily regimen including ethambutol (15 mg/kg orally), rifampin (10 mg/kg orally; maximum, 600 mg/day), and a macrolide (azithromycin 250 mg orally OR clarithromycin 1000 mg orally (or 500 mg orally twice daily)), with or without an injectable aminoglycoside (streptomycin OR amikacin), is recommended as initial therapy for patients with fibrocavitary disease or severe nodular/bronchiectatic disease. For patients weighing less than 50 kg or older than 70 years, the clarithromycin dose may be reduced to 500 mg daily (or 250 mg twice daily) if gastrointestinal intolerance occurs.
- Advanced (Severe) or Previously Treated Disease:
- An aggressive daily regimen including ethambutol (15 mg/kg orally), rifampin 10 mg/kg orally (maximum, 600 mg/day) OR rifabutin 150 to 300 mg orally, a macrolide (azithromycin 250 mg orally OR clarithromycin 1000 mg orally [or 500 mg orally twice daily]), and an injectable aminoglycoside (streptomycin OR amikacin) is recommended as initial therapy for patients with fibrocavitary disease or severe nodular/bronchiectatic disease. For patients weighing less than 50 kg or older than 70 years, the clarithromycin dose may be reduced to 500 mg daily (or 250 mg twice daily) if gastrointestinal intolerance occurs.
Active tuberculosis - HIV infection
Pulmonary tuberculosis
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Ethambutol in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Pulmonary tuberculosis; Adjunct(13 years or older)
- Dosing Information
- 15 to 20 mg/kg ORALLY daily, OR 50 mg/kg ORALLY twice weekly; MAX 2500 mg/dose (guideline dosing) (younger than 15 years and 40 kg or less ideal body weight) .
- Initial, 15 mg/kg ORALLY once daily as combination therapy with at least one other antitubercular agent (eg, isoniazid, with or without streptomycin); patients weighing over 97 kg, dose is 1500 mg(13 years or older).
- Retreatment, 25 mg/kg ORALLY once daily for 60 days, then 15 mg/kg ORALLY once daily as combination therapy with at least one of the second line antitubercular agents not previously used (eg, cycloserine, ethionamide, pyrazinamide, or viomycin; additionally, isoniazid, aminosalicylic acid, streptomycin, or other alternating drug regimens have been used); patients weighing over 99 kg, dose is 2500 mg (13 years or older).
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Tuberculosis
Disseminated infection due to Mycobacterium avium-intracellulare group; Prophylaxis - HIV infection
- Dosing Information
- 15 to 25 mg/kg ORALLY daily (MAX 2.5 g/day) in combination with clarithromycin 7.5 mg/kg ORALLY twice daily (MAX 500 mg twice daily), with or without rifabutin 5 mg/kg ORALLY daily (MAX 300 mg/day).
Disseminated infection due to Mycobacterium avium-intracellulare group - HIV infection
- Dosing Information
- 15 to 25 mg/kg ORALLY once daily (MAX 2.5 g/day) in combination with either clarithromycin 7.5 to 15 mg/kg ORALLY twice daily (MAX 500 mg twice daily) (preferred) or azithromycin 10 to 12 mg/kg (MAX 500 mg/day) ORALLY once daily (alternative); for severe disease, add rifabutin 10 to 20 mg/kg ORALLY once daily (MAX, 300 mg/day) .
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Ethambutol in pediatric patients.
Contraindications
- MYAMBUTOL is contraindicated in patients who are known to be hypersensitive to this drug. It is also contraindicated in patients with known optic neuritis unless clinical judgement determines that it may be used. MYAMBUTOL is contraindicated in patients who are unable to appreciate and report visual side effects or changes in vision (e.g., young children, unconscious patients).
Warnings
- MYAMBUTOL may produce decreases in visual acuity which appear to be due to optic neuritis. This effect may be related to dose and duration of treatment. This effect is generally reversible when administration of the drug is discontinued promptly. However, irreversible blindness has been reported. (See PRECAUTIONS and ADVERSE REACTIONS).
- Liver toxicities including fatalities have been reported (see ADVERSE REACTIONS). Baseline and periodic assessment of hepatic function should be performed.
Precautions
- MYAMBUTOL ethambutol hydrochloride is not recommended for use in pediatric patients under thirteen years of age since safe conditions for use have not been established.
- Patients with decreased renal function need the dosage reduced as determined by serum levels of MYAMBUTOL, since the main path of excretion of this drug is by the kidneys.
- Because this drug may have adverse effects on vision, physical examination should include ophthalmoscopy, finger perimetry and testing of color discrimination. In patients with visual defects such as cataracts, recurrent inflammatory conditions of the eye, optic neuritis, and diabetic retinopathy, the evaluation of changes in visual acuity is more difficult, and care should be taken to be sure the variations in vision are not due to the underlying disease conditions. In such patients, consideration should be given to relationship between benefits expected and possible visual deterioration since evaluation of visual changes is difficult.
- As with any potent drug, baseline and periodic assessment of organ system functions, including renal, hepatic, and hematopoietic, should be performed.
Adverse Reactions
Clinical Trials Experience
- MYAMBUTOL may produce decreases in visual acuity, including irreversable blindness, which appear o be due to optic neuritis. Optic neuropathy including optic neuritis or retrobulbar neuritis occuring in association with ethambutol therapy may be characterized by one or more of the following events: decreased visual acuity, scotoma, color blindness, and/or visual defect. These events have also been reported in the absence of a diagnosis of optic or retrobulbar neuritis.
- Patients should be advised to report promptly to their physician any change of visual acuity
- The change in visual acuity may be unilateral or bilateral and hence each eye must be tested separately and both eyes tested together. Testing of visual acuity should be performed before beginning MYAMBUTOL therapy and periodically during drug administration, except that it should be done monthly when a patient is on a dosage of more than 15 mg per kilogram per day. Snellen eye charts are recommeneded for testing of visual acuity. Studies have shown that there are definite fluctuations of one or two lines of the Snellen chart in the visual acuity of many tuberculous patients not receiving MYAMBUTOL.
- The following table may be useful in interpreting possible changes in visual acuity attributable to MYAMBUTOL.
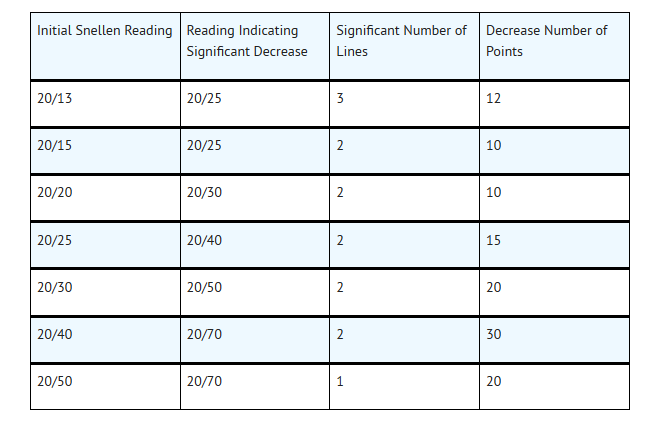
- In general, changes in visual acuity less than those indicated under "Significant Number of Lines" and "Decrease Number of Points" may be due to chance variation, limitations of the testing method, or physiologic variability. Conversely, changes in visual acuity equaling or exceeding those under "Significant Number of LInes" and "Decrease Number of Points" indicate need for retesting and careful evaluation of the patient's visual status. If careful evaluation confirms the magnitude of visual change and fails to reveal another cause, MYAMBUTOL should be discontinued and the patient reevaluated at frequent intervals. Progressive decreases in visual acuity during therapy must be considered to be due to MYAMBUTOL.
- If corrective glasses are used prior to treatment, these must be worn during visual acuity testing. During 1 to 2 years of therapy, a refractive error may develop which must be corrected in order to obtain accurate test results. Testing the visual acuity through a pinhole eliminates refractive error. Patients developing visual abnormality during MYAMBUTOL treatment may show subjective visual symptoms before, or simultaneously with, the demonstration of decreases in visual acuity, and all patients receiving MYAMBUTOL should be questioned periodically about blurred vision and other subjective eye symptoms.
- Recovery of visual acuity generally occurs over a period of weeks to months after the drug has been discontinued. Some patients have received MYAMBUTOL ethambutol hydrochloride again after such recovery without recurrence of loss of visual acuity.
- Other adverse reactions reported include: hypersensitivity, anaphylactic/anaphylactoid reaction, dermatitis, erythmea multiforme, pruritus, and joint pain; anorexia, nausea, vomiting, gastrointestinal upset, and abdominal pain; fever, malaise, headache, and dizziness; mental confusion, disorientation, and possible hallucinations; thrombocytopenia, leukopenia and neutropenia. Numbness and tingling of the extremities due to peripheral neuritis have been reported.
- Elevated serum uric acid levels occur and precipiation of acute gout has been reported. Pulmonary infiltrates, with or without eosinophilia, also have been reported during MYAMBUTOL therapy. Liver toxicities, including fatalities, have been reported. (See WARNINGS). Since MYAMBUTOL is recommended for therapy in conjunction with one or more other antituberculous drugs, these changes may be related to the concurent therapy. Hypersensitivity syndrome consisting of cutaneous reaction (such as rash or exofoliative dermatitis), eosinophilia, and one or more of the following: hepatitis, pneumonitis, nephritis, myocarditis, pericarditis. Fever and lymphadenopathy may be present.
Postmarketing Experience
- There is limited information regarding Postmarketing Experience of Ethambutol in the drug label.
Drug Interactions
- The results of a study of coadministration of ethambutol (50 mg/kg) with an aluminum hydroxide containing antacid to 13 patients with tuberculosis showed a reduction of mean serum concentrations and urinary excretion of ethambutol of approximately 20% and 13%, respectively, suggesting that the oral absorption of ethambutol may be reduced by these antacid products. It is recommended to avoid concurrent administration of ethambutol with aluminum hydroxide containing antacids for at least 4 hours following ethambutol administration.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C Teratogenic Effects: Pregnancy Category C
- There are no adequate and well-controlled studies in pregnant women. There are reports of ophthalmic abnormalities occuring in infants born to women on antituberculous therapy that included ethambutol hydrochloride. MYAMBUTOL should be used during pregnancy only if the benefit justifies the potential risk to the fetus.
- MYAMBUTOL has been shown to be teratogenic in pregnant mice and rabbits when given in high doses. When pregnant mice or rabbits were treated with high doses of ethambutol hydrochloride, fettal mortality was slightly but not significantly (P>0.05) increased. Femal rats treated with ethambutol hydrochloride displayed slight but insignificant (P>0.05) decreases in fertility and litter size.
- In fetuses born of mice treated with high doses of MYAMBUTOL during pregnancy, a low incidence of cleft palate, exencephaly and abnormality of the vertebral column were observed. Minor abnormalities of the cervical vertebra were seen in the newborn of rats treated with high doses of ethambutol hydrochloride during pregnancy. Rabbits receiving high doses of MYAMBUTOL during pregnancy gave birth to two fetuses with monophthalmmia, one with a shortened right forearm accompanied by bulateral wrist-joint contracture and one with hare lip and cleft palate.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
- There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ethambutol in women who are pregnant.
Labor and Delivery
- There is no FDA guidance on use of Ethambutol during labor and delivery.
Nursing Mothers
- MYAMBUTOL is excreted into breast milk. The use of MYAMBUTOL should be considered only if the expected benefit to the mother outweighs the potential risk to the infant.
Pediatric Use
- MYAMBUTOL ethambutol hydrochloride is not recommended for use in pediatric patients under thirteen years of age since safe conditions have not been established.
Geriatic Use
- There are limited date on the use of ethambutol in the elderly. One study of 101 patients, 65 years and older, on multiple drug antituberculosis regimens included 94 patients on ethambutol. No differences in safety of tolerability were observed in these patients compared with that reported in adults in general.
- Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Gender
- There is no FDA guidance on the use of Ethambutol with respect to specific gender populations.
Race
- There is no FDA guidance on the use of Ethambutol with respect to specific racial populations.
Renal Impairment
- There is no FDA guidance on the use of Ethambutol in patients with renal impairment.
Hepatic Impairment
- There is no FDA guidance on the use of Ethambutol in patients with hepatic impairment.
Females of Reproductive Potential and Males
- There is no FDA guidance on the use of Ethambutol in women of reproductive potentials and males.
Immunocompromised Patients
- There is no FDA guidance one the use of Ethambutol in patients who are immunocompromised.
Administration and Monitoring
Administration
- MYAMBUTOL should not be used alone, in initial treatment or in retreatment. MYAMBUTOL should be administered on a once every 24-hour basis only. Absorption is not significantly altered by administration with food. Therapy, in general, should be continued until bacteriological conversion has become permanent and maximal clinical improvement has occured.
- MYAMBUTOL is not recommended for use in pediatric patients under thirteen years of age since safe conditions for use have not been established.
- Initial Treatment: In patients who have not received previous antituberculous therapy, administer MYAMBUTOL 15 mg/kg (7 mg/lb) of body weight, as a single oral dose once every 24 hours. In the more recent studies, isoniazid has been administered concurrently in a single, daily, oral dose.
- Retreatment: In patients who have received previous antituberculous therapy, administer MYAMBUTOL 25 mg/kg (11mg/lb) of body weight, as a single oral dose once every 24 hours. Concurrently administer at least one other antituberculous drug to which the organisms have been demonstrated to be susceptible by appropriate in vitro tests. Suitable drugs usually consist of those not previously used in the treatment of the patient. After 60 days of MYAMBUTOL administration, decrease the dose to 15 mg/kg (7 mg/lb) of body weight, and administer as a single oral dose once every 24 hours.
- During the period when patient is on a daily dose of 25 mg/kg, monthly eye examinations are advised.
- See Table for easy selection of proper weight-dose tablet(s).
Monitoring
- There is limited information regarding Monitoring of Ethambutol in the drug label.
IV Compatibility
- There is limited information regarding IV Compatibility of Ethambutol in the drug label.
Overdosage
- There is limited information regarding Chronic Overdose of Ethambutol in the drug label.
Pharmacology
There is limited information regarding Ethambutol Pharmacology in the drug label.
Mechanism of Action
Structure
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Ethambutol in the drug label.
Pharmacokinetics
- MYAMBUTOL® following a single oral dose of 25 mg/kg of body weight, attains a peak of 2 to 5 mcg/mL in serum 2 to 4 hours after administration. When the drug is administered daily for longer periods of time at this dose, serum levels are similar. The serum levels of MYAMBUTOL falls to undetectable levels by 24 hours after the last dose except in some patients with abnormal renal function. The intracellular concentrations of erythrocytes reach peak values approximately twice those of plasma and maintain this ratio throughout the 24 hours.
- During the 24-hour period following oral administration of MYAMBUTOL approximately 50 percent of the initial dose is excreted unchanged in the urine, while an additional 8 to 15 percent appears in the form of metabolites. The main path of metabolism appears to be an initial oxidation of the alcohol to an aldehydic intermediate, followed by conversion to a dicarboxylic acid. From 20 to 22 percent of the initial dose is excreted in the feces as unchanged drug. No drug accumulation has been observed with consecutive single daily doses of 25 mg/kg in patients with normal kidney function, although marked accumulation has been demonstrated in patients with renal insufficiency.
- MYAMBUTOL diffuses into actively growing mycobacterium cells such as tubercle bacilli. MYAMBUTOL appears to inhibit the synthesis of one or more metabolites, thus causing impairment of cell metabolism, arrest of multiplication, and cell death. No cross resistance with other available antimycobacterial agents has been demonstrated.
- MYAMBUTOL has been shown to be effective against strains of Mycobacterium tuberculosis but does not seem to be active against fungi, viruses, or other bacteria. Mycobacterium tuberculosis strains previously unexposed to MYAMBUTOL have been uniformly sensitive to concentrations of 8 or less mcg/mL, depending on the nature of the culture media. When MYAMBUTOL has been used alone for treatment of tuberculosis, tubercle bacilli from these patients have developed resistance of MYAMBUTOL ethambutol hydrochloride by in vitro susceptibility tests; the development of resistance has been unpredictable and appears to occur in a step-like manner. No cross resistance between MYAMBUTOL and other antituberculous drugs has been reported. MYAMBUTOL has reduced the emergence of mycobacterial resistance is isoniazid when both drugs have been used concurrently.
- Any agar diffusion microbiologic assay, based upon inhibition of Mycobacterium smegmatis (ATCC 607) may be used to determine concentrations of MYAMBUTOL in serum and urine.
Nonclinical Toxicology
ANIMAL PHARMACOLOGY
Toxicological studies in dogs on high prolonged doses produced evidence of myocardial damage and failure, and depigmentation of the tapetum lucidum of he eyes, the significance of which is not known. Degenerative changes in the central nervous system, apparently not dose-related, have also been noted in dogs receiving ethambutol hydrochloride over a prolonged period.
In the rhesus monkey, neurological signs appeared after treatment with high doses given daily over a period of several months. These were correlated with specific serum levels of ethambutol hydrochloride and with definite neuroanatomical changes in the central nervous system. Focal interstitial carditis was also noted in monkeys which received ethambutol hydrochloride in high doses for a prolonged period.
Clinical Studies
- There is limited information regarding Clinical Studies of Ethambutol in the drug label.
How Supplied
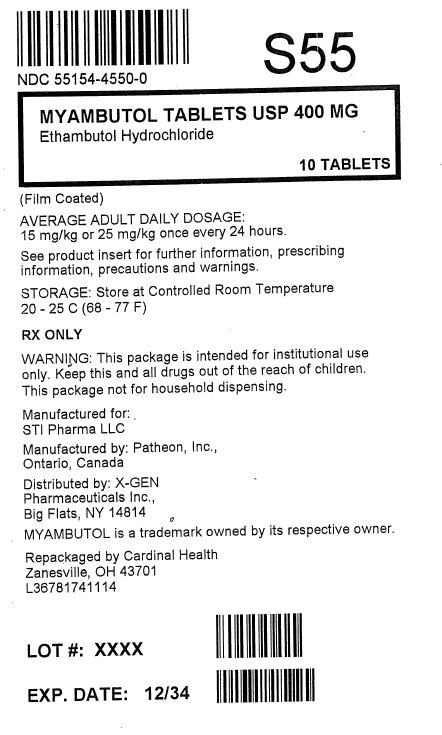
- MYAMBUTOL® Ethambutol Hydrochloride Tablets USP
- 100 mg - round, convex, white, film coated tablets engraved M6 on one side are supplied as follows:
- NDC 68850-010-01 - Bottle of 100
- 400 mg - round, convex, white, scored, film coated tablets engraved with M to the left and 7 to the right of the score on one side are supplied as follows:
- NDC 68850-012-01 - Bottle of 100
- NDC 68850-012-02 - 10 Blister-packs x 10 Tablets
Storage
- Store at controlled room temperature 20° to 25°C (68° to 77°F).
Images
Drug Images
{{#ask: Page Name::Ethambutol |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
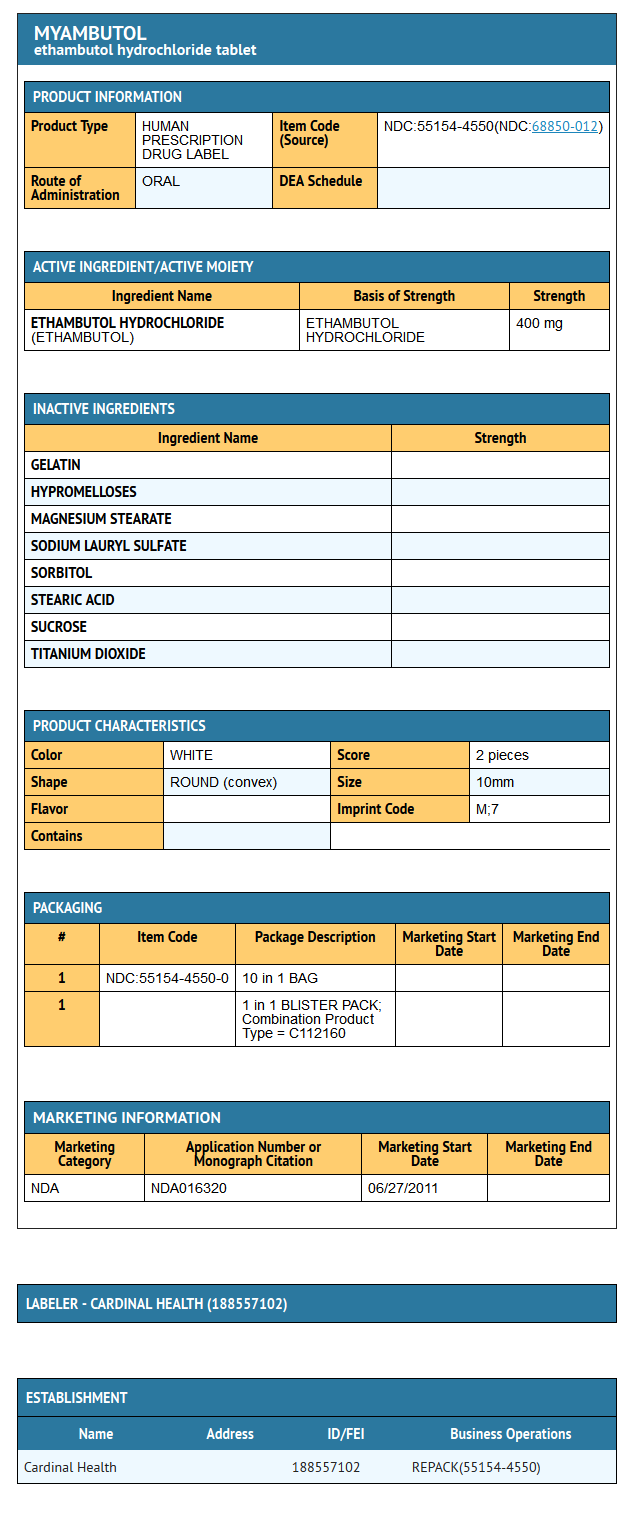
{{#ask: Label Page::Ethambutol |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- There is limited information regarding Patient Counseling Information of Ethambutol in the drug label.
Precautions with Alcohol
- Alcohol-Ethambutol interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Myambutol
Look-Alike Drug Names
- A® — B®[1]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Ethambutol
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Ethambutol |Label Name=Ethambutol11.png
}}
{{#subobject:
|Label Page=Ethambutol |Label Name=Ethambutol11.png
}}