Deucravacitinib
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kosar Doraghi, M.D.[2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Warning: Hypersensitivity Reaction
See full prescribing information for complete Boxed Warning.
Hypersensitivity: such as angioedema
Discontinue if a clinically significant hypersensitivity reaction occurs.
SOTYKTU is not approved for use in RA.
|
Overview
Deucravacitinib is a tyrosine kinase 2 (TYK2) inhibitor that is FDA approved for the treatment of adults with moderate-to-severe plaque psoriasis who are candidates for systemic therapy or phototherapy. There is a Black Box Warning for this drug as shown here. Common adverse reactions include hypersensitivity reaction, upper respiratory infections, blood creatine phosphokinase increased, herpes simplex, mouth ulcers,folliculitis, and acne.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Recommended Evaluations and Immunizations Prior to Treatment Initiation.
- The suggested dose for SOTYKTU is 6 mg to be taken orally once daily, with or without food. Avoid crushing, cutting, or chewing the tablets.
- SOTYKTU is not recommended in patients with severe hepatic impairment,no dosage adjustment is needed for patients with mild to moderate hepatic impairment.
Off-Label Use and Dosage (Adult)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and efficacy of SOTYKTU have not been established in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Contraindications
History of hypersensitivity reaction.
Warnings
|
Warning: Hypersensitivity Reaction
See full prescribing information for complete Boxed Warning.
Hypersensitivity: such as angioedema
Discontinue if a clinically significant hypersensitivity reaction occurs.
SOTYKTU is not approved for use in RA.
|
- Hypersensitivity
If a clinically significant hypersensitivity reaction occurs, institute appropriate therapy and discontinue SOTYKTU.
- Infections
Deucravacitinib may increase the risk of infections. The most common serious infections reported with SOTYKTU included pneumonia and COVID-19. Closely monitor patients for the development of signs and symptoms of infection during and after treatment with SOTYKTU.
- Viral Reactivation
Herpes virus reactivation, the impact of SOTYKTU on chronic viral hepatitis reactivation is unknown. Consider viral hepatitis screening and monitoring for reactivation in accordance with clinical guidelines before starting therapy and during therapy with SOTYKTU. If signs of reactivation occur, consult a hepatitis specialist. SOTYKTU is not recommended for use in patients with active hepatitis B or hepatitis C.
- Tuberculosis
Assess patients for both latent and active tuberculosis (TB) infection before starting SOTYKTU treatment. Do not prescribe SOTYKTU to individuals with active TB. Commence treatment for latent TB before initiating SOTYKTU administration. Consider anti-TB therapy prior to initiation of SOTYKTU in patients with a past history of latent or active TB in whom an adequate course of treatment cannot be confirmed. Monitor patients receiving SOTYKTU for signs and symptoms of active TB during treatment.
- Malignancy including Lymphomas
Malignancies, including lymphomas, were observed in clinical trials with SOTYKTU. Consider the benefits and risks for the individual patient prior to initiating or continuing therapy with SOTYKTU.
- Rhabdomyolysis and Elevated CPK
The use of SOTYKTU was linked to a higher occurrence of asymptomatic elevation in creatine phosphokinase (CPK) and rhabdomyolysis compared to a placebo. If significantly elevated CPK levels are observed or if myopathy is diagnosed or suspected, discontinue SOTYKTU. Advise patients to promptly report any unexplained muscle pain, tenderness, or weakness, especially if accompanied by malaise or fever.
- Laboratory Abnormalities: Triglyceride Elevations and Liver Enzyme Elevations
Regularly assess serum triglyceride levels in accordance with clinical guidelines for hyperlipidemia during the course of SOTYKTU treatment. Manage patients based on the clinical guidelines for the control of hyperlipidemia. Treatment with SOTYKTU was associated with an increase in the incidence of liver enzyme elevation compared to treatment with placebo. Liver serum transaminase elevations ≥ 3 times the ULN were reported in subjects treated with SOTYKTU. Evaluate liver enzymes at baseline and thereafter in patients with known or suspected liver disease according to routine patient management.
- Immunizations
Before starting SOTYKTU therapy, contemplate administering all age-appropriate immunizations in alignment with current immunization guidelines, including prophylactic herpes zoster vaccination. Refrain from administering live vaccines to individuals undergoing SOTYKTU treatment. The impact of SOTYKTU on the response to both live and non-live vaccines has not been assessed.
- Potential Risks Related to JAK Inhibition
The association between TYK2 inhibition and potential adverse reactions observed in Janus Kinase (JAK) inhibition is not known. A large, randomized postmarketing safety trial involving a JAK inhibitor for rheumatoid arthritis (RA), focusing on patients aged 50 and above with at least one cardiovascular risk factor, revealed higher rates of all-cause mortality, sudden cardiovascular death, major adverse cardiovascular events, overall thrombosis, deep venous thrombosis, pulmonary embolism, and malignancies (excluding non-melanoma skin cancer) in those treated with the JAK inhibitor compared to TNF blockers. It's important to note that SOTYKTU is not approved for use in RA.
Adverse Reactions
Clinical Trials Experience
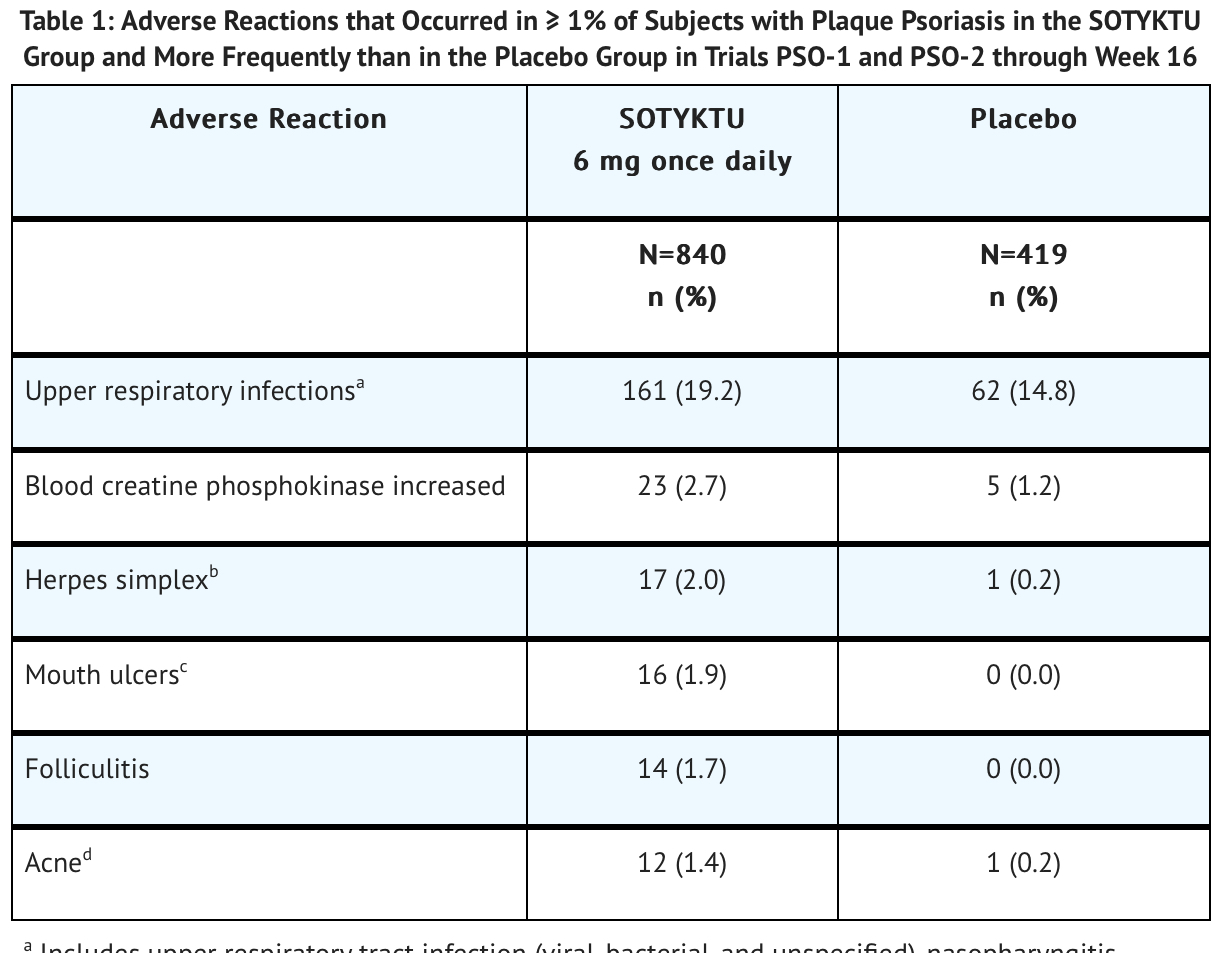
Most common adverse reactions (≥ 1%) are [upper respiratory infections], blood creatine phosphokinase increased, herpes simplex, mouth ulcers, folliculitis, and acne.
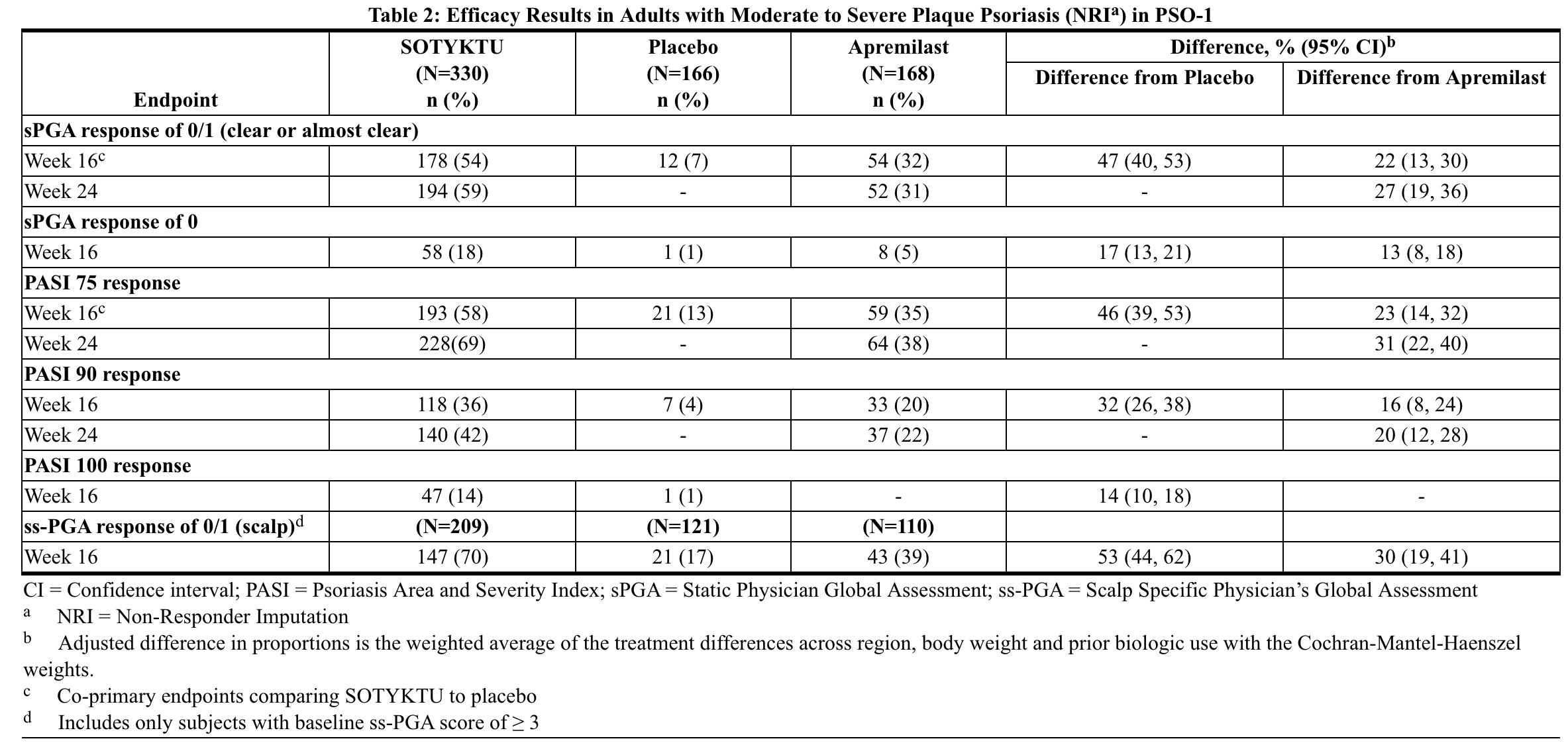
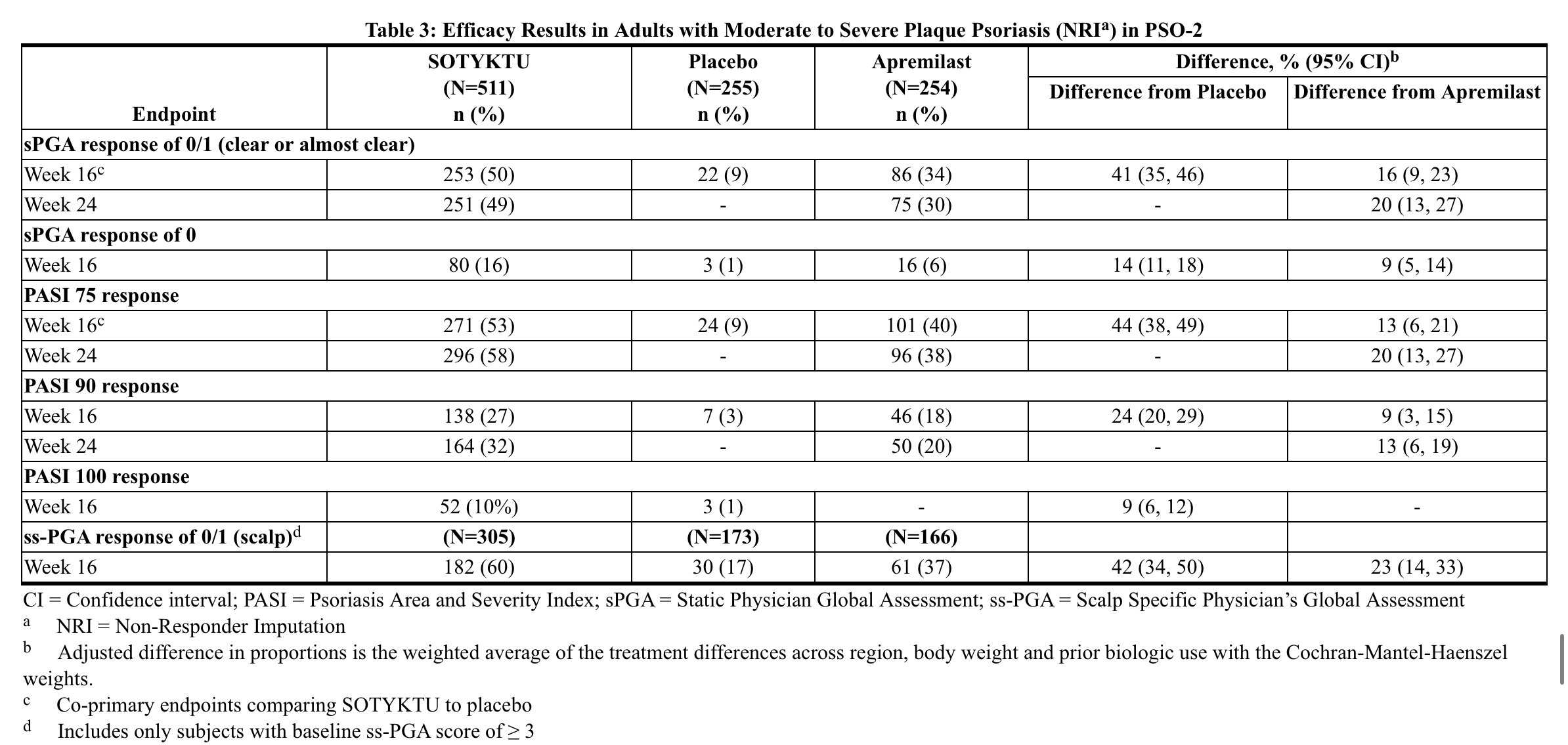
- SOTYKTU's safety was evaluated in two placebo- and active-controlled trials (PSO-1 and PSO-2) and an open-label extension trial involving 1,519 individuals with moderate-to-severe plaque psoriasis. The 6 mg daily oral dose was administered, with 1,141 subjects exposed for at least a year. In the placebo-controlled period (PSO-1 and PSO-2), SOTYKTU had a 2.4% discontinuation rate due to adverse reactions, compared to 3.8% for placebo. The trials included subjects randomized to SOTYKTU, placebo, or apremilast. Table 1 details adverse reactions during the 16-week controlled period. The majority of participants were White (87%), male (67%), and had a mean age of 47 years.
- Includes upper respiratory tract infection (viral, bacterial, and unspecified), nasopharyngitis, pharyngitis (including viral, streptococcal, and unspecified), sinusitis (includes acute, viral, bacterial), rhinitis, rhinotracheitis, tracheitis, laryngitis, and tonsillitis (including bacterial, streptococcal)
- oral herpes, genital herpes, herpes simplex, and herpes virus infection
- mouth ulceration, aphthous ulcer, tongue ulceration, and stomatitis
- acne, acne cystic, and dermatitis acneiform.
Adverse reactions that occurred in < 1% of subjects in the SOTYKTU group were herpes zoster.
- Specific Adverse Reactions:
- Infections
During the 16-week placebo-controlled phase, infections were observed in 29% of the SOTYKTU group (equivalent to 116 events per 100 person-years), compared to 22% in the placebo group (equivalent to 83.7 events per 100 person-years). The majority of these infections were non-serious, mild to moderate in severity, and did not result in the discontinuation of SOTYKTU. In the same 16-week period, serious infections were documented in 5 subjects treated with SOTYKTU (2.0 per 100 patient-years) and 2 subjects treated with placebo (1.6 per 100 patient-years). Notably, the most frequently reported serious infections during the 52-week treatment period were pneumonia and COVID-19.
- Malignancies
During the 0-to-52-week treatment period of the two clinical trials, PSO-1 and PSO-2 (total exposure of 986 patient-years with SOTYKTU), malignancies (excluding non-melanoma skin cancer) were reported in three subjects treated with SOTYKTU (0.3 per 100 patient-years). These included isolated cases of breast cancer, hepatocellular carcinoma, and lymphoma occurring after 24, 32, and 25 weeks of treatment, respectively. Throughout PSO-1, PSO-2, and the subsequent open-label extension trial where subjects from the controlled trials could enroll, a total of three subjects (0.1 per 100 patient-years) developed lymphoma while receiving SOTYKTU, with occurrences after 25, 77, and 98 weeks of treatment.
- Laboratory Abnormalities
During the 16-week placebo-controlled period, the following adverse events were observed in subjects treated with SOTYKTU compared to placebo: Creatine Phosphokinase (CPK) elevations were reported in 23 subjects (9.3 per 100 patient-years) with SOTYKTU and 5 subjects (4.1 per 100 patient-years) with placebo. Liver enzyme elevations (ALT and AST) ≥3 times the upper limit of normal (ULN) were observed in SOTYKTU-treated subjects: 9 subjects (3.6 per 100 patient-years) for ALT and 13 subjects (5.2 per 100 patient-years) for AST, compared to 2 subjects (1.6 per 100 patient-years) for both enzymes with placebo. Decreased Glomerular Filtration Rate (GFR) occurred in 4 subjects (1.6 per 100 patient-years) with SOTYKTU and 1 subject (0.8 per 100 patient-years) with placebo among those with moderate renal impairment (eGFR 30-59 mL/min) at baseline. Two SOTYKTU-treated subjects experienced worsening proteinuria from baseline. Mean triglyceride levels increased by 10.3 mg/dL during the 16-week treatment period and by 9.1 mg/dL during the 52-week treatment period with SOTYKTU.
Postmarketing Experience
- Safety Through Week 52
In PSO-1 and PSO-2, the exposure adjusted incidence rate of adverse reactions in subjects treated with SOTYKTU from Week 0 through Week 52 without switching treatment did not increase compared to the rate observed during the first 16 weeks of treatment.
Drug Interactions
There is limited information regarding Deucravacitinib Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
The existing data from case reports regarding the utilization of SOTYKTU during pregnancy are inadequate.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Deucravacitinib in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Deucravacitinib during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Deucravacitinib in women who are nursing.
Pediatric Use
There is no FDA guidance on the use of Deucravacitinib in pediatric settings.
Geriatic Use
Out of 1,519 subjects treated with SOTYKTU for plaque psoriasis, 10% were aged 65 or older, with 1.4% aged 75 or older. During the initial 16-week period, older subjects, particularly those 65 and over (including 75 and over), experienced a higher incidence of serious adverse reactions, including infections, and more discontinuations due to adverse reactions compared to younger adults. However, there were no significant differences in the effectiveness of SOTYKTU between patients aged 65 and older and younger adults.
Gender
There is no FDA guidance on the use of Deucravacitinib with respect to specific gender populations.
Race
There is no FDA guidance on the use of Deucravacitinib with respect to specific racial populations.
Renal Impairment
No dose adjustment of SOTYKTU is recommended in patients with mild, moderate, or severe renal impairment.
Hepatic Impairment
There is no recommended need to adjust the dose of SOTYKTU for patients with mild or moderate hepatic impairment. However, the use of SOTYKTU is not advised for patients with severe hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Deucravacitinib in women of reproductive potentials and males.
Immunocompromised Patients
Not recommended for use in combination with other potent immunosuppressants.
Administration and Monitoring
Administration
- Recommended Evaluations and Immunizations Prior to Treatment Initiation
- The suggested dose for SOTYKTU is 6 mg to be taken orally once daily, with or without food. Avoid crushing, cutting, or chewing the tablets.
- SOTYKTU is not recommended in patients with severe hepatic impairment,no dosage adjustment is needed for patients with mild to moderate hepatic impairment.
Monitoring
There is limited information regarding Deucravacitinib Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Deucravacitinib and IV administrations.
Overdosage
There is no experience regarding human overdosage with SOTYKTU. The extent of deucravacitinib elimination by hemodialysis was small (5.4% of dose per dialysis treatment), and thus hemodialysis for treatment of overdose with SOTYKTU is limited.
Pharmacology
There is limited information regarding Deucravacitinib Pharmacology in the drug label.
Mechanism of Action
Deucravacitinib is an inhibitor of tyrosine kinase 2 (TYK2). TYK2 is a member of the Janus kinase (JAK) family. Deucravacitinib binds to the regulatory domain of TYK2, stabilizing an inhibitory interaction between the regulatory and the catalytic domains of the enzyme. This results in allosteric inhibition of receptor-mediated activation of TYK2 and its downstream activation of Signal Transducers and Activators of Transcription (STATs) as shown in cell-based assays. JAK kinases, including TYK2, function as pairs of homo- or heterodimers in the JAK-STAT pathways. TYK2 pairs with JAK1 to mediate multiple cytokine pathways and also pairs with JAK2 to transmit signals as shown in cell-based assays. The precise mechanism linking inhibition of TYK2 enzyme to therapeutic effectiveness in the treatment of adults with moderate-to-severe plaque psoriasis is not currently known.
Structure
Deucravacitinib is a tyrosine kinase 2 (TYK2) inhibitor and is described chemically as:
- 6-(cyclopropanecarbonylamido)-4-[2-methoxy-3-(1-methyl-1,2,4-triazol-3-yl)anilino]-N-(trideuteriomethyl)pyridazine-3-carboxamide.
The molecular formula is C20H19D3N8O3 and the molecular weight of the free base is 425.47. Deucravacitinib has the structural formula:
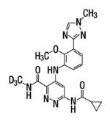
Deucravacitinib is a white to yellow powder. The solubility of deucravacitinib is pH dependent. Solubility decreases with increasing pH.
- SOTYKTU (deucravacitinib) tablets are supplied in 6 mg strength for oral administration. Each tablet contains deucravacitinib as the active ingredient and the following inactive ingredients: anhydrous lactose, croscarmellose sodium, hypromellose acetate succinate, magnesium stearate, microcrystalline cellulose, and silicon dioxide. In addition, the film coating Opadry® II Pink contains the following inactive ingredients: iron oxide red, iron oxide yellow, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide.
Pharmacodynamics
In patients with psoriasis, deucravacitinib reduced psoriasis-associated gene expression in psoriatic skin in a dose dependent manner, including genes regulated by the IL-23 pathway and type I IFN pathway. After 16 weeks of once-daily treatment, deucravacitinib reduced IL-17A, IL-19, and beta-defensin levels by approximately 47% to 50%, 72%, and 81% to 84%, respectively. However, the specific connection between these changes in gene expression and how deucravacitinib works to produce clinical benefits remains unclear.
Pharmacokinetics
After oral intake, deucravacitinib exhibited proportional increases in plasma Cmax and AUC across a dosage range of 3 mg to 36 mg (0.5 to 6 times the approved recommended dose) in healthy individuals. The accumulation of deucravacitinib following once-daily dosing in healthy subjects was minimal, being less than 1.4-fold. Pharmacokinetics (PK) profiles of both deucravacitinib and its active metabolite, BMT-153261, were similar between healthy individuals and those with psoriasis. Steady-state Cmax and AUC24 of deucravacitinib after a 6 mg once-daily dose were 45 ng/mL and 473 ng·hr/mL, respectively. Corresponding values for the active metabolite BMT-153261 were 5 ng/mL and 95 ng·hr/mL.
- Absorption:
Deucravacitinib demonstrated an oral bioavailability of 99%, with a median Tmax ranging from 2 to 3 hours in healthy subjects.
- Food Effect:
Administration of a high-fat, high-calorie meal did not significantly alter the pharmacokinetics of deucravacitinib. However, concurrent food intake decreased Cmax and AUC of deucravacitinib by approximately 24% and 11%, respectively, and prolonged Tmax by 1 hour. Similarly, food intake reduced Cmax and AUC of BMT-153261 by approximately 23% and 10%, respectively, and prolonged Tmax by 2 hours.
- Distribution:
At steady state, the volume of distribution of deucravacitinib was 140 L. Deucravacitinib exhibited a protein binding of 82 to 90%, with a blood-to-plasma concentration ratio of 1.26.
- Elimination:
The volume of distribution of deucravacitinib at steady state is 140 L. Protein binding of deucravacitinib was 82 to 90% and the blood-to-plasma concentration ratio was 1.26.
- metabolism:
Deucravacitinib is metabolized primarily by cytochrome P-450 (CYP) 1A2 to form the major metabolite BMT-153261. Additionally, it undergoes metabolism by CYP2B6, CYP2D6, carboxylesterase (CES) 2, and uridine glucuronyl transferase (UGT) 1A9. The active metabolite, BMT-153261, exhibits comparable potency to the parent drug, but its circulating exposure accounts for approximately 20% of the total drug-related components.
- Excretion:
After a single dose of radiolabeled deucravacitinib, approximately 13% and 26% of the dose was recovered unchanged in urine and feces, respectively. BMT-153261 accounted for approximately 6% and 12% of the dose in urine and feces, respectively.
- Specific Populations:
In patients with renal impairment, deucravacitinib exposure varied based on the severity of impairment. In patients with mild renal impairment, Cmax was slightly lower, while AUCinf remained unchanged. However, in patients with moderate, severe, or end-stage renal disease (ESRD) on dialysis, both Cmax and AUCinf were elevated compared to those with normal renal function. Similar trends were observed for BMT-153261. In patients with hepatic impairment, deucravacitinib exposure increased with the severity of impairment, whereas exposure to BMT-153261 decreased.
- Drug Interaction Studies:
No clinically significant interactions were observed between deucravacitinib and various drugs, including cyclosporine, fluvoxamine, ritonavir, diflunisal, pyrimethamine, famotidine, or rabeprazole. Likewise, co-administration of deucravacitinib did not affect the pharmacokinetics of rosuvastatin, methotrexate, mycophenolate mofetil (MMF), or oral contraceptives.
- In Vitro Studies:
Deucravacitinib did not significantly inhibit or induce cytochrome P450 (CYP) enzymes or carboxylesterase (CES) enzymes. It also did not act as an inhibitor of uridine diphosphate (UDP)-glucuronosyl transferase (UGT) enzymes. Deucravacitinib acted as a substrate for Pgp, BCRP, and OCT1, but not for other transporter systems. It inhibited BCRP and OATP1B3 but not other transporters.
Nonclinical Toxicology
- Carcinogenesis, Mutagenesis, Impairment of Fertility:
The carcinogenic potential of deucravacitinib was assessed in 2-year rat and 6-month rasH2 transgenic mouse studies. No evidence of tumorigenicity was observed in male or female rats that received deucravacitinib at oral doses up to 15 mg/kg/day (51 times the MRHD based on AUC comparison). No evidence of tumorigenicity was observed in male or female Tg.rasH2 mice that received deucravacitinib at oral doses up to 60 mg/kg/day. Deucravacitinib was not mutagenic in a bacterial mutagenicity assay (Ames test) or clastogenic in an in vitro chromosomal aberration assay (cultured Chinese hamster ovary cells) or in an in vivo rat peripheral blood micronucleus assay. In male rats, deucravacitinib had no effects on reproductive parameters (mating, fertility, and sperm morphology) or early embryonic development of their offspring at oral doses up to 50 mg/kg/day (224 times the MRHD based on AUC comparison). In female rats, deucravacitinib had no effects on mating, fertility, or early embryonic parameters at oral doses up to 50 mg/kg/day (171 times the MRHD based on AUC comparison).
Clinical Studies
- Plaque Psoriasis
The effectiveness and safety of administering SOTYKTU at a dosage of 6 mg per day were evaluated in two multicenter, randomized, double-blind, placebo- and active-controlled clinical trials, PSO-1 (NCT03624127) and PSO-2 (NCT03611751) which enrolled subjects 18 years of age and older with moderate-to-severe plaque psoriasis who were eligible for systemic therapy or phototherapy. Subjects had a body surface area (BSA) involvement of ≥ 10%, a Psoriasis Area and Severity Index (PASI) score ≥ 12, and a static Physician’s Global Assessment (sPGA) ≥ 3 (moderate or severe). In PSO-1 and PSO-2, efficacy was assessed in 1,684 subjects randomized to either SOTYKTU (6 mg orally once daily), placebo, or apremilast (30 mg orally twice daily).
- Endpoints:
Both trials evaluated the responses at Week 16 in comparison to a placebo for the two co-primary endpoints:
- proportion of subjects who achieved a sPGA score of 0 (clear) or 1 (almost clear) with at least a 2-grade improvement from baseline;
- the proportion of subjects who achieved at least a 75% improvement in PASI scores from baseline (PASI 75).
Other comparisons between SOTYKTU and placebo that were secondary endpoints at Week 16:
- the proportion of subjects who achieved PASI 90, PASI 100, sPGA 0, scalp severity PGA (ss-PGA) score of 0 (clear) or 1 (almost clear) with at least 2-grade improvement, and Psoriasis Symptoms and Signs Diary (PSSD) Symptom Score of 0 (symptom-free).
Comparisons between SOTYKTU and apremilast were made for the following secondary endpoints at these time points:
- at Week 16 and Week 24 (PSO-1 and PSO-2), the proportion of subjects who achieved PASI 75, PASI 90, and sPGA 0/1 with at least a 2-grade improvement from baseline
- at Week 16 (PSO-1 and PSO-2), the proportion of subjects who achieved sPGA 0 and ss-PGA 0/1 with at least a 2-grade improvement from baseline (scalp).
- Result:
In both trials, the subjects had a mean age of 47 years, a mean weight of 91 kg, with 67% being male, 13% Hispanic or Latino, 87% White, 2% Black, and 10% Asian. At the start, subjects had a median affected body surface area (BSA) of 20% and a median Psoriasis Area and Severity Index (PASI) score of 19. About 80% had a moderate severity score (sPGA 3), and 20% had severe (sPGA 4) psoriasis. Approximately 18% had a history of psoriatic arthritis. Across both trials, 40% of subjects had previously received phototherapy, 42% were new to any systemic therapy, 41% had received prior non-biologic systemic treatment, and 35% had received prior biologic therapy. Efficacy results comparing SOTYKTU to apremilast and placebo in PSO-1 are presented in Table 2, while Table 3 displays the efficacy results in PSO-2.
- Examination of age, gender, race, body weight, baseline disease severity, and prior systemic therapy did not identify differences in response to SOTYKTU at Week 16 among these subgroups.
- Maintenance and Durability of Response:
In PSO-1, subjects who received SOTYKTU showed sustained responses at Week 52, with 78% maintaining sPGA 0/1 response, 82% maintaining PASI 75 response, and 74% maintaining PASI 90 response from Week 24. In PSO-2, subjects originally randomized to SOTYKTU and responding at Week 24 were either continued on treatment or withdrawn to receive placebo. Among those continuing treatment, 70% maintained sPGA 0/1 response and 80% maintained PASI 75 response at Week 52. Conversely, among those withdrawn to placebo, only 24% maintained sPGA 0/1 response and 31% maintained PASI 75 response at Week 52. The median time to loss of response was approximately 8 weeks for sPGA 0/1 responders and 12 weeks for PASI 75 responders who were withdrawn to placebo.
- Patient Reported Outcomes:
A greater proportion of subjects treated with SOTYKTU compared to placebo achieved Psoriasis Symptoms and Signs Diary (PSSD) symptom score of 0 (absence of itch, pain, burning, stinging, and skin tightness) at Week 16 (8% in SOTYKTU vs. 1% in placebo) in both trials.
How Supplied
SOTYKTU™ (deucravacitinib) tablets are offered in the following specifications:
- Tablet Strength: 6 mg
- Tablet Color/Shape: Pink, round, biconvex, film-coated tablet
- Tablet Markings: Laser printed with “BMS 895” and “6 mg” on one side
- Package Size: Bottles of 30 with child-resistant closure
- NDC Code: 0003-0895-11
Storage
Store SOTYKTU tablets at 20° to 25°C (68° to 77°F); excursions permitted between 15° and 30°C (59° and 86°F)
Images
Drug Images
{{#ask: Page Name::Deucravacitinib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Deucravacitinib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Before starting SOTYKTU therapy and with each prescription renewal, patients are advised to carefully review the FDA-approved patient labeling (Medication Guide) as there may be updated information they should be aware of. Patients should be informed about both the potential benefits and risks associated with SOTYKTU.
- Hypersensitivity Reactions:
Patients should discontinue SOTYKTU and seek immediate medical attention if they experience any symptoms of serious hypersensitivity reactions.
- Infections:
Patients should be informed that SOTYKTU may reduce their immune system's ability to fight infections. They should contact their healthcare provider promptly if they develop any signs or symptoms of infection. Additionally, patients should be aware that herpes infections, including serious cases, may occur with the use of SOTYKTU.
- Malignancies including Lymphomas:
Patients should be informed that SOTYKTU may increase their risk of developing malignancies, including lymphomas. They should be instructed to inform their healthcare provider if they have a history of any type of cancer [see Warnings and Precautions.
- Rhabdomyolysis:
Patients should be informed that SOTYKTU may increase their risk of developing rhabdomyolysis. They should be instructed to promptly inform their healthcare provider if they experience unexplained muscle pain, tenderness, or weakness, especially if accompanied by malaise or fever.
- Laboratory Abnormalities:
Patients should be aware that SOTYKTU may affect certain laboratory tests, and blood tests may be necessary before and during treatment with SOTYKTU [see *Warnings and Precautions.
- Immunizations:
Patients should be advised that vaccination with live vaccines is not recommended during treatment with SOTYKTU. Medications that interact with the immune system may increase the risk of infection following administration of live vaccines. Patients should inform their healthcare provider that they are taking SOTYKTU before receiving any potential vaccinations.
- Pregnancy:
Patients should report their pregnancy to Bristol-Myers Squibb Company by calling 1-800-721-5072
Precautions with Alcohol
Alcohol-Deucravacitinib interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Deucravacitinib Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Deucravacitinib Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Deucravacitinib
|Pill Name=30 Tablets SOTYKTUTM (deucravacitinib)
|Drug Name=Deucravacitinib
|Pill Ingred=Rx only|+sep=;
|Pill Imprint=
|Pill Dosage=6 mg {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=SOTYKTU Bristol Myers Squibb
|NDC=NDC 0003-0895-11
}}