Coronary heart disease pathophysiology
|
Coronary heart disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Coronary heart disease pathophysiology On the Web |
|
American Roentgen Ray Society Images of Coronary heart disease pathophysiology |
|
Risk calculators and risk factors for Coronary heart disease pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Atherosclerotic heart disease can be thought of as a wide spectrum of disease of the heart. At one end of the spectrum is the asymptomatic individual with atheromatous streaks within the walls of the coronary arteries. These streaks represent the early stage of atherosclerotic heart disease and do not obstruct the flow of blood. The streaks increase in size and lead to the formation of plaque within the arteries. When the plaque obstruct the passage of blood within the coronary arteries, it causes ischemia, or lack of oxygen, within the heart muscle.
Pathophysiology
Limitation of blood flow to the heart causes ischemia (cell starvation secondary to a lack of oxygen) of the myocardial cells. When myocardial cells die from lack of oxygen, this is called a myocardial infarction (commonly called a heart attack). It leads to heart muscle damage, heart muscle death and later scarring without heart muscle regrowth.
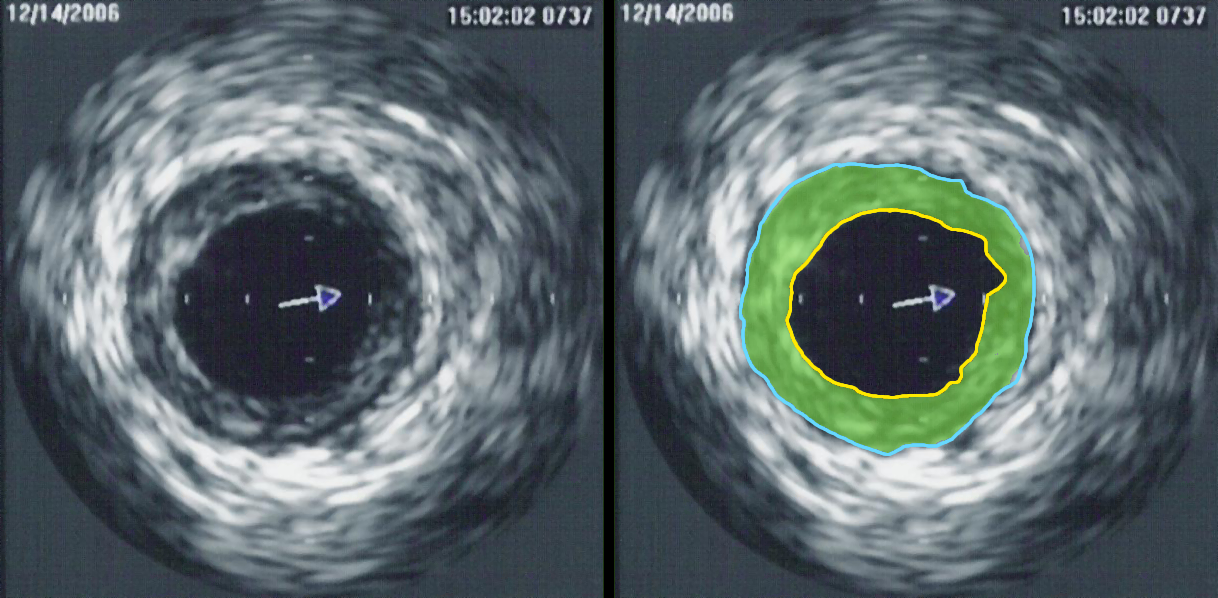
Myocardial infarction usually results from the sudden occlusion of a coronary artery when a plaque ruptures, activating the clotting system and atheroma-clot interaction fills the lumen of the artery to the point of sudden closure. The typical narrowing of the lumen of the coronary artery before sudden closure is typically 20%, according to clinical research completed in the late 1990s and using IVUS examinations within 6 months prior to a heart attack. High grade stenoses as such exceeding 75% blockage, such as detected by stress testing, were found to be responsible for only 14% of acute heart attacks the rest being due to plaque rupture/ spasm. The events leading up to plaque rupture are only partially understood. Myocardial infarction is also caused, far less commonly, by spasm of the artery wall occluding the lumen, a condition also associated with atheromatous plaque and CHD.
CHD is associated with smoking, obesity, hypertension and a chronic sub-clinical lack of vitamin C. A family history of CHD is one of the strongest predictors of CHD. Screening for CHD includes evaluating homocysteine levels, high-density and low-density lipoprotein (cholesterol) levels and triglyceride levels.
Pathophysiology of Atherosclerosis
Atherosclerotic heart disease can be thought of as a wide spectrum of disease of the heart. At one end of the spectrum is the asymptomatic individual with atheromatous streaks within the walls of the coronary arteries (the arteries of the heart). These streaks represent the early stage of atherosclerotic heart disease and do not obstruct the flow of blood. A coronary angiogram performed during this stage of disease may not show any evidence of coronary artery disease, because the lumen of the coronary artery has not decreased in caliber.
Over a period of many years, these streaks increase in thickness. While the atheromatous plaques initially expand into the walls of the arteries, eventually they will expand into the lumen of the vessel, affecting the flow of blood through the arteries. While it was originally believed that the growth of atheromatous plaques was a slow, gradual process, recent evidence suggests that the gradual buildup may be complemented by small plaque ruptures which cause the sudden increase in the plaque burden due to accumulation of thrombus material.
Atheromatous plaques that cause obstruction of less than 70 percent of the diameter of the vessel rarely cause symptoms of obstructive coronary artery disease. As the plaques grow in thickness and obstruct more than 70 percent of the diameter of the vessel, the individual develops symptoms of obstructive coronary artery disease. At this stage of the disease process, the patient can be said to have ischemic heart disease. The symptoms of ischemic heart disease are often first noted during times of increased workload of the heart. For instance, the first symptoms include exertional angina or decreased exercise tolerance.
As the degree of coronary artery disease progresses, there may be near-complete obstruction of the lumen of the coronary artery, severely restricting the flow of oxygen-carrying blood to the myocardium. Individuals with this degree of coronary heart disease typically have suffered from one or more myocardial infarctions (heart attacks), and may have signs and symptoms of chronic coronary ischemia, including symptoms of angina at rest and flash pulmonary edema.
A distinction should be made between myocardial ischemia and myocardial infarction. Ischemia means that the amount of oxygen supplied to the tissue is inadequate to supply the needs of the tissue. When the myocardium becomes ischemic, it does not function optimally. When large areas of the myocardium becomes ischemic, there can be impairment in the relaxation and contraction of the myocardium. If the blood flow to the tissue is improved, myocardial ischemia can be reversed. Infarction means that the tissue has undergone irreversible death due to lack of sufficient oxygen-rich blood.
A 2006 study by the Cleveland Clinic found a region on Chromosome 17 was confined to families with multiple cases of myocardial infarction.[1]
Periodontal disease may contribute to this inflammation.[2][3] Poor oral hygiene is associated with elevated C-reactive protein and fibrinogen.[3]
A more controversial link is that between Chlamydophila pneumoniae infection and atherosclerosis.[4] While this intracellular organism has been demonstrated in atherosclerotic plaques, evidence is inconclusive as to whether it can be considered a causative factor. Treatment with antibiotics in patients with proven atherosclerosis has not demonstrated a decreased risk of heart attacks or other coronary vascular diseases.[5]
Syndrome X
Cardiac syndrome X is the presence of typical angina, abnormal exercise-test results, and normal coronary arteries (including no vasospasm).[6] Syndrome X may be caused by subendocardial hypoperfusion that can be demonstrated by cardiovascular magnetic resonance imaging during the administration of adenosine.[6]
Myocardial infarction
An individual may develop a rupture of an atheromatous plaque at any stage of the spectrum of coronary heart disease. The acute rupture of a plaque may lead to an acute myocardial infarction (heart attack). Surprisingly, more fatal ruptures occur on plaques that are not severely stenosed[7][8][9]
Approximately 15% of NSTEMI and 2% of STEMI patients have no obstruction of coronary arteries and in about half of these patients, spasm of a coronary artery can be induced.[10]
References
- ↑ Farrall M, Green FR, Peden JF, Olsson PG, Clarke R, Hellenius ML, Rust S, Lagercrantz J, Franzosi MG, Schulte H, Carey A, Olsson G, Assmann G, Tognoni G, Collins R, Hamsten A, Watkins H, on behalf of the PROCARDIS Consortium (2006). "Genome-Wide Mapping of Susceptibility to Coronary Artery Disease Identifies a Novel Replicated Locus on Chromosome 17". PLoS Genetics. 2 (5): e72. PMID 16710446.
- ↑ Humphrey LL, Fu R, Buckley DI, Freeman M, Helfand M (2008). "Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis". J Gen Intern Med. 23 (12): 2079–86. doi:10.1007/s11606-008-0787-6. PMID 18807098. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 de Oliveira C, Watt R, Hamer M (2010). "Toothbrushing, inflammation, and risk of cardiovascular disease: results from Scottish Health Survey". BMJ. 340: c2451. doi:10.1136/bmj.c2451. PMID 20508025.
- ↑ Saikku P, Leinonen M, Tenkanen L, Linnanmaki E, Ekman MR, Manninen V, Manttari M, Frick MH, Huttunen JK. (1992). "Chronic Chlamydia pneumoniae infection as a risk factor for coronary heart disease in the Helsinki Heart Study". Ann Intern Med. 116 (4): 273–8. PMID 1733381.
- ↑ Andraws R, Berger JS, Brown DL. (2005). "Effects of antibiotic therapy on outcomes of patients with coronary artery disease: a meta-analysis of randomized controlled trials". JAMA. 293 (21): 2641–7. PMID 15928286.
- ↑ 6.0 6.1 Panting JR, Gatehouse PD, Yang GZ; et al. (2002). "Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging". N. Engl. J. Med. 346 (25): 1948–53. doi:10.1056/NEJMoa012369. PMID 12075055. Unknown parameter
|month=ignored (help) - ↑ Mann JM, Davies MJ (1996). "Vulnerable plaque. Relation of characteristics to degree of stenosis in human coronary arteries". Circulation. 94 (5): 928–31. PMID 8790027.
- ↑ Kolodgie FD, Virmani R, Burke AP, Farb A, Weber DK, Kutys R; et al. (2004). "Pathologic assessment of the vulnerable human coronary plaque". Heart. 90 (12): 1385–91. doi:10.1136/hrt.2004.041798. PMC 1768577. PMID 15547008.
- ↑ Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM (2000). "Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions". Arterioscler Thromb Vasc Biol. 20 (5): 1262–75. PMID 10807742.
- ↑ Ong P, Athanasiadis A, Hill S, Vogelsberg H, Voehringer M, Sechtem U (2008). "Coronary artery spasm as a frequent cause of acute coronary syndrome: The CASPAR (Coronary Artery Spasm in Patients With Acute Coronary Syndrome) Study". J. Am. Coll. Cardiol. 52 (7): 523–7. doi:10.1016/j.jacc.2008.04.050. PMID 18687244. Unknown parameter
|month=ignored (help)