Cefuroxime clinical studies
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Abdurahman Khalil, M.D. [2]
Ceftin Tablets
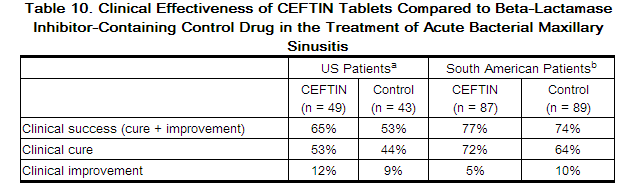
Acute Bacterial Maxillary Sinusitis
One adequate and well-controlled study was performed in patients with acute bacterial maxillary sinusitis. In this study each patient had a maxillary sinus aspirate collected by sinus puncture before treatment was initiated for presumptive acute bacterial sinusitis. All patients had to have radiographic and clinical evidence of acute maxillary sinusitis. As shown in the following summary of the study, the general clinical effectiveness of CEFTIN Tablets was comparable to an oral antimicrobial agent that contained a specific beta-lactamase inhibitor in treating acute maxillary sinusitis. However, sufficient microbiology data were obtained to demonstrate the effectiveness of CEFTIN Tablets in treating acute bacterial maxillary sinusitis due only to Streptococcus pneumoniae or non−beta-lactamase−producing Haemophilusinfluenzae. An insufficient number of beta-lactamase−producing Haemophilusinfluenzae andMoraxellacatarrhalis isolates were obtained in this trial to adequately evaluate the effectiveness of CEFTIN Tablets in the treatment of acute bacterial maxillary sinusitis due to these 2 organisms.
This study enrolled 317 adult patients, 132 patients in the United States and 185 patients in South America. Patients were randomized in a 1:1 ratio to cefuroxime axetil 250 mg twice daily or an oral antimicrobial agent that contained a specific beta-lactamase inhibitor. An intent-to-treat analysis of the submitted clinical data yielded the following results:
a 95% Confidence interval around the success difference [-0.08, +0.32].
b 95% Confidence interval around the success difference [-0.10, +0.16].
In this trial and in a supporting maxillary puncture trial, 15 evaluable patients had non-beta-lactamase−producing Haemophilusinfluenzae as the identified pathogen. Ten (10) of these 15 patients (67%) had their pathogen (non-beta-lactamase−producing Haemophilusinfluenzae) eradicated. Eighteen (18) evaluable patients had Streptococcus pneumoniae as the identified pathogen. Fifteen (15) of these 18 patients (83%) had their pathogen (Streptococcus pneumoniae) eradicated.
Safety
The incidence of drug-related gastrointestinal adverse events was statistically significantly higher in the control arm (an oral antimicrobial agent that contained a specific beta-lactamase inhibitor) versus the cefuroxime axetil arm (12% versus 1%, respectively; P<.001), particularly drug-related diarrhea (8% versus 1%, respectively; P = .001).
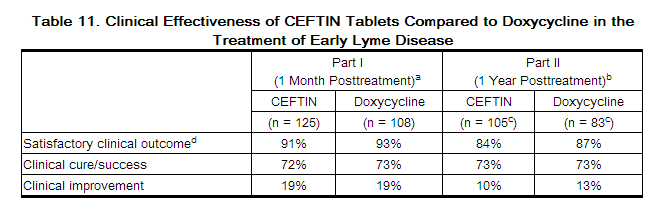
Early Lyme Disease
Two adequate and well-controlled studies were performed in patients with early Lyme disease. In these studies all patients had to present with physician-documented erythema migrans, with or without systemic manifestations of infection. Patients were randomized in a 1:1 ratio to a 20-day course of treatment with cefuroxime axetil 500 mg twice daily or doxycycline 100 mg 3 times daily. Patients were assessed at 1 month posttreatment for success in treating early Lyme disease (Part I) and at 1 year posttreatment for success in preventing the progression to the sequelae of late Lyme disease (Part II).
A total of 355 adult patients (181 treated with cefuroxime axetil and 174 treated with doxycycline) were enrolled in the 2 studies. In order to objectively validate the clinical diagnosis of early Lyme disease in these patients, 2 approaches were used: 1) blinded expert reading of photographs, when available, of the pretreatment erythema migrans skin lesion; and 2) serologic confirmation (using enzyme-linked immunosorbent assay [ELISA] and immunoblot assay [“Western” blot]) of the presence of antibodies specific to Borreliaburgdorferi, the etiologic agent of Lyme disease. By these procedures, it was possible to confirm the physician diagnosis of early Lyme disease in 281 (79%) of the 355 study patients. The efficacy data summarized below are specific to this “validated” patient subset, while the safety data summarized below reflect the entire patient population for the 2 studies.
Analysis of the submitted clinical data for evaluable patients in the “validated” patient subset yielded the following results:
a 95% confidence interval around the satisfactory difference for Part I (-0.08, +0.05).
b95% confidence interval around the satisfactory difference for Part II (-0.13, +0.07).
cn’s include patients assessed as unsatisfactory clinical outcomes (failure + recurrence) in Part I (CEFTIN - 11 [5 failure, 6 recurrence]; doxycycline - 8 [6 failure, 2 recurrence]).
d Satisfactory clinical outcome includes cure + improvement (Part I) and success + improvement (Part II).
CEFTIN and doxycycline were effective in prevention of the development of sequelae of late Lyme disease.
Safety
Drug-related adverse events affecting the skin were reported significantly more frequently by patients treated with doxycycline than by patients treated with cefuroxime axetil (12% versus 3%, respectively; P = .002), primarily reflecting the statistically significantly higher incidence of drug-related photosensitivity reactions in the doxycycline arm versus the cefuroxime axetil arm (9% versus 0%, respectively; P<.001). While the incidence of drug-related gastrointestinal adverse events was similar in the 2 treatment groups (cefuroxime axetil - 13%; doxycycline - 11%), the incidence of drug-related diarrhea was statistically significantly higher in the cefuroxime axetil arm versus the doxycycline arm (11% versus 3%, respectively; P = .005).
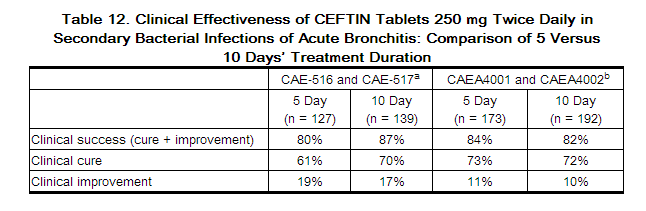
Secondary Bacterial Infections of Acute Bronchitis
Four randomized, controlled clinical studies were performed comparing 5 days versus 10 days of CEFTIN for the treatment of patients with secondary bacterial infections of acute bronchitis. These studies enrolled a total of 1,253 patients (CAE-516 n = 360; CAE-517 n = 177; CAEA4001 n = 362; CAEA4002 n = 354). The protocols for CAE-516 and CAE-517 were identical and compared CEFTIN 250 mg twice daily for 5 days, CEFTIN 250 mg twice daily for 10 days, and AUGMENTIN® 500 mg 3 times daily for 10 days. These 2 studies were conducted simultaneously. CAEA4001 and CAEA4002 compared CEFTIN 250 mg twice daily for 5 days, CEFTIN 250 mg twice daily for 10 days, and CECLOR® 250 mg 3 times daily for 10 days. They were otherwise identical to CAE-516 and CAE-517 and were conducted over the following 2 years. Patients were required to have polymorphonuclear cells present on the Gram stain of their screening sputum specimen, but isolation of a bacterial pathogen from the sputum culture was not required for inclusion. The following table demonstrates the results of the clinical outcome analysis of the pooled studies CAE-516/CAE-517 and CAEA4001/CAEA4002, respectively:
a 95% Confidence interval around the success difference [-0.164, +0.029].
b95% Confidence interval around the success difference [-0.061, +0.103].
The response rates for patients who were both clinically and bacteriologically evaluable were consistent with those reported for the clinically evaluable patients.
Safety
In these clinical trials, 399 patients were treated with CEFTIN for 5 days and 402 patients with CEFTIN for 10 days. No difference in the occurrence of adverse events was observed between the 2 regimens.
References
http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/050605s042lbl.pdf