Cardiorenal syndrome
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate-Editor(s)-in-Chief: Yazan Daaboul; Rim Halaby; Dina Elantably, MD, MSc[2]
Overview
Cardiorenal syndrome (CRS) comprises a group of disease states that involve simultaneous kidney and heart failure. Because the kidney and the heart lead a “symbiotic” bi-directional relationship; the vitality of one organ ultimately and inevitably depends on the vitality of the other. In cardiorenal syndrome, an acute or chronic dysfunction in the heart or the kidneys causes an acute or chronic dysfunction of the other organ. Cardiorenal syndromes have recently earned major clinical significance because of their complex management challenges and their profound prognostic indication of mortality in patients suffering from concomitant heart and kidney diseases. The greatest challenge a clinician faces with cardiorenal syndromes is the therapeutic approach and pharmacological intervention required in favor of a CRS patient with known poor prognosis. Today’s management approaches, despite proven efficacy, remain notorious for their injurious effects on the target organs of CRS. Individualized treatment remains up till now an optimal modality of approach pending the understanding of CRS, pathophysiology, and effective prevention.
Classification
Five subgroups have been identified and further approved by the Acute Dialysis Quality Initiative (ADQI) in 2010 on the basis of the following:
- Pathophysiology
- Acute vs. chronic
- Concomitance of cardiac and renal dysfunction
For descriptive purposes, the five cardiorenal syndromes have also been named differently [1] as shown in the table below:
| Type | Name | Description |
| Type 1 | Acute cardiorenal syndrome | Acute heart failure leads to acute kidney injury (AKI) |
| Type 2 | Chronic cardiorenal syndrome | Chronic cardiac dysfunction leads to chronic kidney disease (CKD) |
| Type 3 | Acute renocardiac syndrome | Acute kidney injury leads to acute cardiac dysfunction |
| Type 4 | Chronic renocardiac syndrome | Chronic kidney injury leads to chronic cardiac dysfunction(eg; coronary disease, heart failure or arryhthmia) |
| Type 5 | Secondary cardiorenal syndrome | Acute or chronic systemic disorder (eg; diabetes mellitus, sepsis) leads to heart and kidney failure |
Pathophysiology
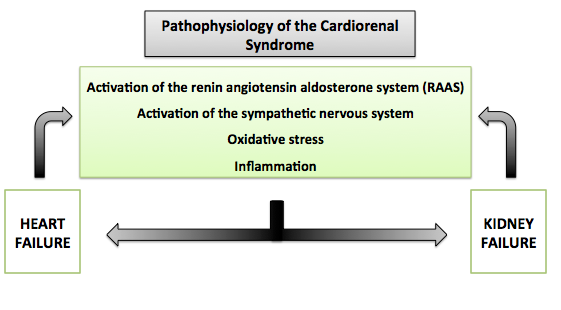
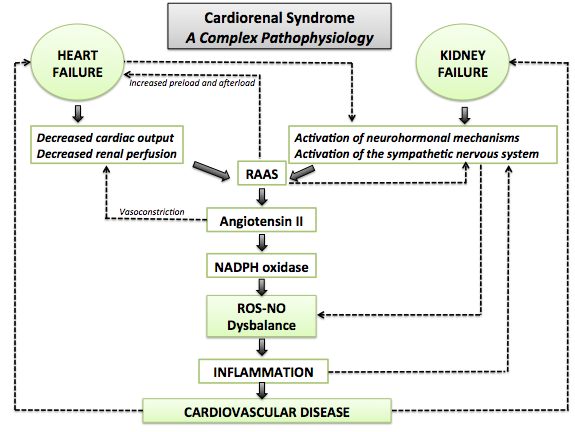
The cardiorenal syndrome is the result of compensatory mechanisms of the body in order to maintain a good blood volume and organ perfusion in the face of heart failure or kidney failure. Regardless of the type of the cardiorenal syndrome, the following events are part of the underlying pathophysiology:
- Activation of the renin angiotensin aldosterone system (RAAS)
- Activation of baroreceptors
- Activation of the sympathetic nervous system
- Oxidative stress.[2]
- Shown below is an image summarizing the bidirectional relationship between the heart and the kidneys in the pathophysiology of the cardiorenal syndrome.
- Shown below is an image showing the complex pathophysiological mechanisms involved in the cardiorenal syndrome.
Cardiorenal Syndrome Type 1
- Acute heart failure leading to acute kidney injury
- Decreased cardiac output, increased venous pressure, kidney congestion, hyperkalemia [1] possibly preventing the use of ACE-I, ARB, and Spironolactone.
Cardiorenal Syndrome Type 2
- Chronic heart dysfunction causing chronic kidney disease
- Erythropoetin deficiency and anemia
- Electrolyte imbalances[3][4]
- Neurohormonal abnormalities with over production of vasoconstrictors
- Altered sensitivity to endogenous vasodilators[1].
Cardiorenal Syndrome Type 3
- Acute kidney injury leading to acute cardiac dysfunction, typically due to bilateral renal artery stenosis[1]
- Fluid overload, neurohormonal activation, pericarditis, acidemia, hyperkalemia.[5][1][6]
Cardiorenal Syndrome Type 4
- Primary chronic kidney disease leading to gradual decreased cardiac function
- Electrolyte imbalances with chronic kidney disease
- Fluid overload.
Cardiorenal Syndrome Type 5
- Combined cardiac and renal dysfunction due to acute or chronic systemic disorders (Sepsis, diabetes, amyloidosis, lupus, sarcoidosis)
- Primary trigger causes simultaneous or sequential damage to both organs
- Injury to heart and kidneys cause of vicious cycle of further injury to each other. [1]
Risk Factors
Risk factors of worsening renal function in patients with heart failure includes[7]:
- Unconrolled hypertension (systolic BP>160 mmHg)
- Diabetes Mellitus
- Previous history of heart failure
- Baseline serum creatinine 1.5 mg/dl or higher.
Epidemiology and Demographics
- The prevalence of moderate to severe kidney impairement in patients with heart failure ranges from 30 to 60%.[8][9]
- Among patients with acute decompensated heart failure , only 9% have normal renal function, whereas approximately 91 % have estimated GFR lower than 89 ml x min x 1.73 m2.[10]
- Among patients with chronic kidney disease on hemodialysis or peritoneal dialysis, 40% have heart failure. In fact, patients with kidney failure are more likely to die from cardiac causes rather than from the kidney failure itself.[11]
Natural History, Complications and Prognosis
- Renal failure is one of the most significant poor prognostic independent risk factors in patients with heart failure.[12]
- Renal failure in the context of ambulatory patients with heart failure carries a poor prognostic sign and high mortality risks even at a creatinine level of 1.3 mg/dL.[13]
- Worsening renal failure, evidenced by an increase in creatinine as low as 0.3 mg/dL, is a poor prognostic factor in hospitalized patients with heart failure. In fact, the increase in the creatinine level rather than the baseline creatinine in these patients correlated with frequent hospitalizations and higher mortality.[14]
Diagnosis
Cardiorenal Syndrome Type 1
- Blood and Urine Neutrophil gelatinase-associated lipocalin (NGAL) [15]
- Cystatin C is a good early predictor of GFR[16][17]
- Serum Creatinine elevates 48-72 h later[18]
Cardiorenal Syndrome Type 2
- Serum creatinine to measure renal function
- Classical makers of heart failure (eg. BNP) and measurement by ultrasound of systolic and diastolic ventricular dysfunction and ejection fraction [19]
Cardiorenal Syndrome Type 3
Cardiorenal Syndrome Type 4
- Classical diagnosis of chronic kidney disease and heart failure[1]
Cardiorenal Syndrome Type 5
- Diagnosis of primary disease
Biomarkers of Cardiorenal Syndromes
- Despite the efficient use of cardiac biomarkers that detect early injury, the detection of acute kidney injury before the consequential fall of GFR has not been possible with the current utilization of serum creatinine. It has become therefore imperative to search for new biomarkers that can readily identify renal damage and thus cardiorenal syndromes rapidly for prompt and efficient management.
- Several novel biomarkers have been introduced to the literature. Nonetheless, none has yet effectively replaced the use of serum creatinine in clinical settings.
Catalytic Iron
- Catalytic iron is based on the use of bleomycin detectable assay to detect catalytic iron in CRS at the level of generation of reactive oxygen species.
- It is a potential diagnostic and therapeutic target for CRS[22].
Neutrophil Gelatinase-Associated Lipocalin (NGAL) or Siderocalin
- It scavenges cellular and pericellular labile iron.
- It has been studied extensively in animal and human models; it increases significantly in plasma and urine [23].
Cystatin C
- It is a cysteine protease inhibitor.
- At the level of the kidney, it is freely filtered, and completely reabsorbed.
- Cystatin C is better than creatinine in estimating GFR and chronic kidney disease status[24].
Other Biomarkers
- Other previous and emerging biomarkers for CRS include Kidney Injury Molecule 1 (KIM-1) [25], N-Acetyl-B-(D) Glucosaminidase (NAG)[26], Interleukin-18 (IL-18)[27], Liver Fatty Acid-Binding Protein (L-FABP) [28], and Tubular Enzymuria such as gamma glutamyl transpeptidase (GGT), alkaline phosphatase, lactate dehydrogenase, and α and π glutathione S-transferase (GST) [29][30].
Treatment
Cardiorenal Syndrome Type 1
- Due to venous congestion; low dose of loop diuretics is most effective.
- High dose diuretic use aggravates acute kidney injury [31].
- Extracorporeal ultrafiltration if resistance to diuretics under optimal conditions[32].
Cardiorenal Syndrome Type 2
- ACE-I, ARB, B-blockers, statins.
- High dose loop diuretics is still debatable whether it is a contributing factor or independent of aggravated of renal disease [33].
- Other treatment modalities: high dose vasodilators[34].
Cardiorenal Syndrome Type 3
- Diuretics are useful.
- Caution with ACE-I and ARB (required for management of heart failure and hypertension, but might aggravate acute kidney injury since kidney highly dependent on renin angiotensin aldoesterone system) [32]
- Other treatment modalities: renal revascularization [35].
Cardiorenal Syndrome Type 4
- Classical treatment of chronic kidney disease and heart failure (beta-blockers, ACE-I, statins, etc.) [32].
Cardiorenal Syndrome Type 5
- Treatment of primary disease.
- Judicious IV fluids and pressor agents might be helpful.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Ronco, C., Haapio, M., House, A., Anavekar, N., & Bellomo, R. (2008). Cardiorenal Syndrome. Journal of the American College of Cardiology, 52(19):1527-1539.
- ↑ Bongartz LG, Cramer MJ, Doevendans PA, Joles JA, Braam B (2005). "The severe cardiorenal syndrome: 'Guyton revisited'". Eur Heart J. 26 (1): 11–7. doi:10.1093/eurheartj/ehi020. PMID 15615794.
- ↑ Jie, J., Verhaar, M., Cramer, M., & et al. (2006). Erythropoietin and the cardiorenal syndrome: Cellular mechanisms on the cardiorenal connectors. American Journal of Physiology - Renal Physiology, 291:F932-F944.
- ↑ Fu, P., & Arcasoy, M. (2007). Erythropoietin protects cardiac myocytes against anthracycline-induced apoptosis. Biochemical and Biophysical Research Communications, 354:372-378.
- ↑ Blake, P., Hasegawa, Y., Khosla, M., Fouad-Tarazi, F., Sakura, N., & Paganini, E. (1996). Isolation of “myocardial depressant factor(s)” from the ultrafiltrate of heart failure patients with acute renal failure. ASAIO Journal, 42:M911-M915.
- ↑ Meyer, T., & Hostetter, T. (2007). Uremia. The New England Journal of Medicine, 257:1316-1325.
- ↑ Forman, Daniel E.; Butler, Javed; Wang, Yongfei; Abraham, William T.; O'Connor, Christopher M.; Gottlieb, Stephen S.; Loh, Evan; Massie, Barry M.; Rich, Michael W.; Stevenson, Lynne Warner; Young, James B.; Krumholz, Harlan M. (2004). "Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure". Journal of the American College of Cardiology. 43 (1): 61–67. doi:10.1016/j.jacc.2003.07.031. ISSN 0735-1097.
- ↑ Smith GL, Lichtman JH, Bracken MB, Shlipak MG, Phillips CO, DiCapua P; et al. (2006). "Renal impairment and outcomes in heart failure: systematic review and meta-analysis". J Am Coll Cardiol. 47 (10): 1987–96. doi:10.1016/j.jacc.2005.11.084. PMID 16697315.
- ↑ Heywood JT, Fonarow GC, Costanzo MR, Mathur VS, Wigneswaran JR, Wynne J; et al. (2007). "High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: a report from the ADHERE database". J Card Fail. 13 (6): 422–30. doi:10.1016/j.cardfail.2007.03.011. PMID 17675055.
- ↑ Heywood, J. Thomas; Fonarow, Gregg C.; Costanzo, Maria Rosa; Mathur, Vandana S.; Wigneswaran, John R.; Wynne, Janet (2007). "High Prevalence of Renal Dysfunction and Its Impact on Outcome in 118,465 Patients Hospitalized With Acute Decompensated Heart Failure: A Report From the ADHERE Database". Journal of Cardiac Failure. 13 (6): 422–430. doi:10.1016/j.cardfail.2007.03.011. ISSN 1071-9164.
- ↑ Foley RN, Parfrey PS, Sarnak MJ (1998). "Epidemiology of cardiovascular disease in chronic renal disease". J Am Soc Nephrol. 9 (12 Suppl): S16–23. PMID 11443763.
- ↑ Gottlieb SS, Abraham WT, Butler J, Forman DE, Loh E, Massie BM, O'Connor CM, Rich MW, Stevenson LW, Young J, Krumholz HM. The prognostic importance of different definitions of worsening renal function in congestive heart failure. J Card Fail. 2002; 8: 136–141.
- ↑ Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2000; 35: 681–689.
- ↑ Hillege HL, Girbes AR, de Kam PJ, Boomsma F, de Zeeuw D, Charlesworth A, Hampton JR, van Veldhuisen DJ. Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation. 2000; 102: 203–210.
- ↑ Mishra, J., Ma, Q., Prada, A., & et al. (2003). Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. Journal of American Society of Nephrology, 14: 2534-2543.
- ↑ Dharnidharka, V., Kwon, C., & Stevens, G. (2002). Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis. American Journal of Kidney Diseases, 40:221-226.
- ↑ Vandevoorde, R., Katlman, T., Ma, Q., & et al. (2006). Serum NGAL and cystatin C as predictive biomarkers for acute kidney injury. Journal of American Society of Nephrology, 17:404A.
- ↑ Wagener, G., Jan, M., Kim, M., & et al. (2006). Association between increases in urinary neutrophil gelatinase-associated lipocalin and acute renal dysfunction after adult cardiac surgery. Anesthesiology, 105:485-491.
- ↑ Palazzuoli, A., Silverberg, D., Iovine, F., & et al. (2007). Effects of beta-erythropoietin treatment on left ventricular remodeling, systolic function, and B-type natriuretic peptide levels in patients with the cardiorenal anemia syndrome. American Heart Journal, 154:645e9-15.
- ↑ Cameron, S., Sokoll, L., Laterza, O., Shah, S., & Green, G. (2007). A multi-marker approach for the prediction of adverse events in patients with acute coronary syndromes. Clinica Chimica Acta, 376:168-173.
- ↑ Forfia, P., Lee, M., Tunin, R., Mahmud, M., Champion, H., & Kass, D. (2007). Acute phosphodiesterase 5 inhibition mimics hemodynamic effects of B-type natriuretic peptide and potentiates B-type natriuretic peptide effects in failing but not normal canine heart. Journal of American College of Cardiology, 49:1079-1088.
- ↑ Lele, S., Shah, S., McCullough, P., & Rajapurkar, M. (2009). Serum catalytic iron as a novel biomarker of vascular injury in acute coronary syndromes. EuroIntervention, 5(3):336-342.
- ↑ Mori, K., & Nakao, K. (2007). Neutrophil gelatinase-associated lipocalin as the real-time indicator of active kidney damage. Kidney International, 71:967-970.
- ↑ McMurray, M., Trivax, J., & McCullough, P. (2009). Serum cystatin C, renal filtration function, and left ventricular remodeling. Circulation. Heart Failure, 2(2):86-89.
- ↑ Kobayashi, M., Hirawa, N., & Morita, S. (2010). Silent brain infarction and rapid decline of kidney function in patients with CKD: a prospective cohort study. American Journal of Kidney Diseases, 56(3):468-476.
- ↑ Wellwood, J., Ellis, B., Price, R., Hammond, K., Thompson, A., & Jones, N. (1975). Urinary N-acetyl- beta-D-glucosaminidase activities in patients with renal disease. British Medical Journal, 3(5980):408-411.
- ↑ Parikh, C., Abraham, E., Ancukiewicz, M., & Edelstein, C. (2005). Urine IL-18 is an early diagnostic marker for acute kidney injury and predicts mortality in the intensive care unit. Journal of the American Society of Nephrology, 16(10):3046-3052.
- ↑ Noiri, E., Doi, K., Negishi, K., & et al. (2009). Urinary fatty acid-binding protein 1: an early predictive biomarker of kidney injury. American Journal of Physiology—Renal Physiology, 296(4):F669-F-679.
- ↑ Liang, X., Liu, S., Chen, Y., & et al. (2010). Combination of urinary kidney injury molecule-1 and interleukin-18 as early biomarker for the diagnosis and progressive assessment of acute kidney injury following cardiopulmonary bypass surgery: a prospective nested casecontrol study. Biomarkers, 15(4):332-339.
- ↑ Endre, Z., & Westhuyzen, J. (2008). Early detection of acute kidney injury: emerging new biomarkers. Nephrology, 13(2):91-98.
- ↑ Howard, P., & Dunn, M. (2001). Aggressive diuresis for severe heart failure in the elderly. Chest, 119:807-810.
- ↑ 32.0 32.1 32.2 Ronco, C. (2008). NGAL: an emerging biomarker of acute kidney injury. International Journal of Artificial Organs, 199:200.
- ↑ Berger, A., Duval, S., & Krumholz, H. (2003). Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. Journal of American College of Cardiology, 42:201-208.
- ↑ Butler, J., Forman, D., Abraham, W., & et al. (2004). Relationship between heart failure treatment and development of worsening renal function among hospitalized patients. American Heart Journal, 147:331-338.
- ↑ Hirsch, A., Haskal, Z., Hertzer, N., & et al. (2006). ACC/AHA guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society . Journal of American College of Cardiology, 47:e1-e192.