Whipple's disease
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
| Whipple's disease | |
 | |
|---|---|
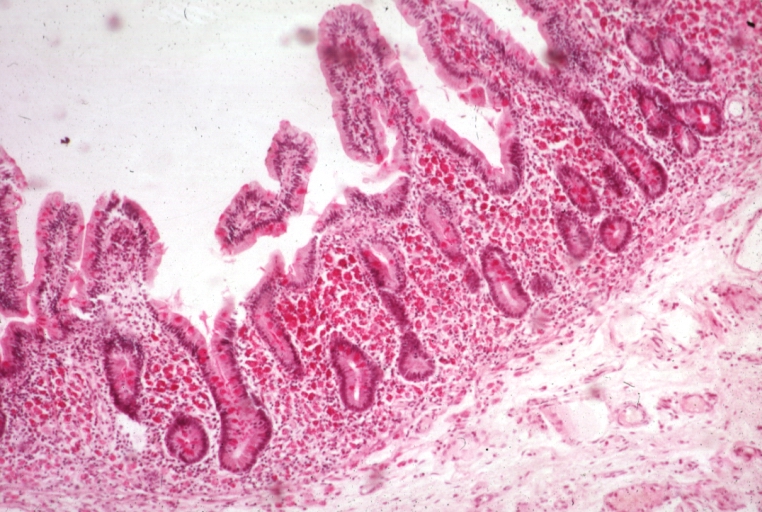
| light microscopy of small intestine;Whipples Disease: enlarged villus with abundant macrophages | |
| ICD-10 | K90.8 |
| ICD-9 | 040.2 |
| DiseasesDB | 14124 |
| MedlinePlus | 000209 |
| eMedicine | med/2409 neuro/397 |
| MeSH | D008061 |
Template:Search infobox Whipple's disease is a rare, systemic infectious disease caused by the bacterium Tropheryma whipplei.[1] First described by George Hoyt Whipple in 1907[2][3] and commonly considered a gastrointestinal disorder, Whipple's disease primarily causes malabsorption but may affect any part of the body including the heart, lungs, brain, joints, and eyes. Weight loss, diarrhea, joint pain, and arthritis are common presenting symptoms, but the presentation can be highly variable and approximately 15% of patients do not have these classic signs and symptoms.[4]. Whipple's disease is significantly more common in men, with a striking 87% of patients being male.[5]. When recognized and treated, Whipple's disease can usually be cured with long-term antibiotic therapy; untreated the disease is ultimately fatal.
Mnemonics
W H I P P L E S
- Weight Loss
- Hyperpigmentation of the skin
- Infection with Tropheryma whipplei
- PAS positive granules in macrophage
- Polyarthritis
- Lymphadenopathy
- Enteric Involvement
- Steatorrhea
Symptoms
- arthritis upto 75% or arthralgia. Usually oligo- or polyarticular, symmetyric, transient and can be chronic.
- malabsorption
- intestinal lipodystrophy (accumulation of fatty deposits in lymph nodes of the intestine)
- lymphadenopathy
- abdominal pain
- diarrhea
- fever
- melanoderma
- neurological symptoms
- cognitive changes
- nystagmus
Diagnosis
Common clinical signs and symptoms of Whipple's disease include weight loss, diarrhea, joint pain or arthritis, fever, and adenopathy. Diagnosis is made by intestinal biopsy, which reveals presence of the organism as PAS-positive macrophage inclusions. Immunohistochemical staining for antibodies against T. whipplei has been used to detect the organism in a variety if tissues, and a confirmatory PCR-based assay is also available.
Endoscopy of the duodenum and jejunum can reveal pale yellow shaggy mucosa with erythematous eroded patches in patients with classic intestinal Whipple's disease, and small bowel X-rays may show some thickened folds.
Treatment
Treatment is with penicillin, ampicillin, tetracycline or co-trimoxazole for 1 -2 years.[4] Any treatment lasting less than a year has an approximate relapse rate of 40%. In the January 4, 2007 issue of the New England Journal of Medicine, Fenollar et al suggest the use of doxycycline with hydroxychloroquine for 12 to 18 months. Sulfonamides (Sulfadiazine or Sulfamethoxazole) should be added for treatment of neurological symptoms.[5]
References
- ↑ Puéchal X (2002). "Whipple's disease". Joint Bone Spine. 69 (2): 133–40. PMID 12027303.
- ↑ Template:WhoNamedIt
- ↑ Whipple GH (1907). "A hitherto undescribed disease characterized anatomically by deposits of fat and fatty acid in the intestinal and mesenteric lymphatic tissues". Bull Johns Hopkins Hosp. 18: 382&ndash, 93.
- ↑ 4.0 4.1 Bai J, Mazure R, Vazquez H, Niveloni S, Smecuol E, Pedreira S, Mauriño E (2004). "Whipple's disease". Clin Gastroenterol Hepatol. 2 (10): 849–60. PMID 15476147.
- ↑ 5.0 5.1 Fenollar F, Puéchal X, Raoult D (2007). "Whipple's disease". N Engl J Med. 356 (1): 55–66. PMID 17202456.
External links
Template:SIB Template:Gastroenterology
de:Morbus Whipple it:Morbo di Whipple nl:Ziekte van Whipple sv:Whipples sjukdom