Wheeze: Difference between revisions
No edit summary |
No edit summary |
||
| Line 42: | Line 42: | ||
**[[rhinovirus]] | **[[rhinovirus]] | ||
**[[respiratory syncytial virus]] | **[[respiratory syncytial virus]] | ||
**[[ | **human metapneumovirus | ||
**Other: | |||
***[[Mycoplasma pneumoniae]] | |||
***[[Chlamydophila pneumoniae]] | |||
***[[Pertussis]] | |||
*[[Bronchopulmonary dysplasia]] | *[[Bronchopulmonary dysplasia]] | ||
*[[Carcinoid syndrome]] | *[[Carcinoid syndrome]] | ||
Revision as of 19:26, 17 February 2009
| Wheeze | |
| ICD-10 | R06.2 |
|---|---|
| ICD-9 | 786.07 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: John Fani Srour, M.D.
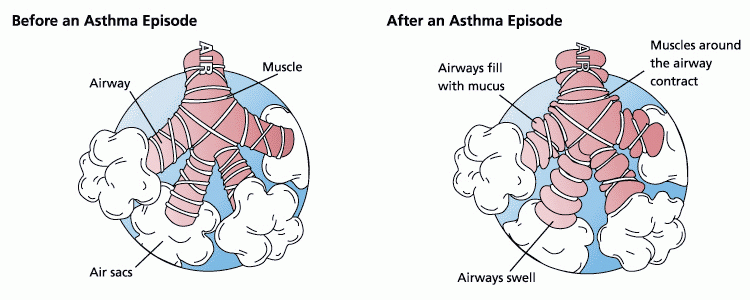
A wheeze is a continuous, coarse, whistling sound produced in the respiratory airways during breathing. For wheezes to occur, some part of the respiratory tree must be narrowed or obstructed, or airflow velocity within the respiratory tree must be heightened. Wheezing is commonly experienced by persons with a lung disease; the most common cause of recurrent wheezing is asthma, a form of reactive airway disease.
Characteristics
Wheezes occupy different portions of the respiratory cycle depending on the site of airway obstruction and its nature. The proportion of the respiratory cycle occupied by the wheeze roughly corresponds to the degree of airway obstruction.Template:Rf,Template:Rf Bronchiolar disease usually causes wheezing that occurs in the expiratory phase of respiration. The presence of expiratory phase wheezing signifies that the patient's peak expiratory flow rate is less than 50% of normal.Template:Rf Wheezing heard in the inspiratory phase on the other hand is often a sign of a stiff stenosis, usually caused by tumors, foreign bodies or scarring. This is especially true if the wheeze is monotonal, occurs throughout the inspiratory phase (ie. is "holoinspiratory"), and is heard more distally, in the trachea. Inspiratory wheezing also occurs in hypersensitivity pneumonitis.Template:Rf Wheezes heard at the end of both expiratory and inspiratory phases usually signify the periodic opening of deflated alveoli, as occurs in some diseases that lead to collapse of parts of the lungs.
The location of the wheeze can also be an important clue to the diagnosis. Diffuse processes that affect most parts of the lungs are more likely to produce wheezing that may be heard throughout the chest via a stethoscope. Localized processes, such as the occlusion of a portion of the respiratory tree, are more likely to produce wheezing at that location, whence the sound will be loudest and radiate outwardly. The pitch of a wheeze does not reliably predict the degree of narrowing in the affected airway.Template:Rf
Wheezing can also occur in people who are not in shape. Wheezing is not a severe problem. The more often you run, the easier breathing gets.
A special type of wheeze is stridor. Stridor — the word is from the Latin, strīdorTemplate:Rf — is a harsh, high-pitched, vibrating sound that is heard in respiratory tract obstruction. Stridor heard solely in the expiratory phase of respiration usually indicates a lower respiratory tract obstruction, "as with aspiration of a foreign body (such as the fabled pediatric peanut)."Template:Rf Stridor in the inspiratory phase is usually heard with obstruction in the upper airways, such as the trachea, epiglottis, or larynx; because a block here means that no air may reach either lung, this condition is a medical emergency.
The differential diagnosis of wheezing is wide, and the cause of wheezing in a given patient is determined by considering the characteristics of the wheezes and the historical and clinical findings made by the examining physician.
Complete Differential Diagnosis of the Causes of Wheeze
(In alphabetical order)
- Abnormal arytenoid movement
- Allergic bronchopulmonary aspergillosis
- Amyloid deposition
- Anaphylaxis
- Angioedema
- Aspiration(foreign particles or foods)
- Asthma including status asthmaticus
- Benign airway tumors
- Bronchiectasis
- Bronchiolitis
- Bronchiolitis obliterans
- Bronchitis (usually viral, bacterial only in patients with tracheostomy or endotracheal intubation)
- influenza A and B
- parainfluenza
- coronavirus (types 1-3)
- rhinovirus
- respiratory syncytial virus
- human metapneumovirus
- Other:
- Bronchopulmonary dysplasia
- Carcinoid syndrome
- Cardiac asthma ( pulmonary edema)
- Cardiomegaly
- Chondromalacia
- Chronic obstructive pulmonary disease: Chronic bronchitis and Emphysema
- Cold induced wheezing
- Congenital abnormalities
- Cricoarytenoid arthritis
- Cystic fibrosis
- Descending aortic aneurysm
- Esophageal foreign body
- Gastroesophageal Reflux Disease (with aspiration)
- Hemorrhage, pulmonary
- Hypertrophied tonsils
- Immunodeficiency
- Infection ( pneumonia )
- Interstitial lung disease
- Intrathoracic goiter
- Klebsiella rhinoscleroma
- Laryngeal edema
- Laryngocele
- Laryngostenosis
- Laryngotracheobronchitis
- Lymphadenopathy
- Lymphangitic carcinomatosis
- Malignancy ( bronchogenic tumors)
- Squamous cell carcinoma with variants: papillary, clear cell, small cell, basaloid
- Small cell carcinoma
- Adenocarcinoma
- Acinar
- Papillary
- Bronchioloalveolar carcinoma
- Non-mucinous (Clara cell/type II pneumocyte type)
- Mucinous (Goblet cell type)
- Mixed mucinous and non-mucinous (Clara cell/type II pneumocyte/goblet cell type) or indeterminate
- Solid adenocarcinoma with mucin formation
- Mixed
- Variants: well-differentiated fetal adenocarcinoma, mucinous ("colloid"), mucinous cystadenocarcinoma, signet ring, clear cell
- Large cell carcinoma with variants: large cell neuroendocrine carcinoma, combined large cell neuroendocrine carcinoma, basaloid carcinoma, lymphoepithelioma-like carcinoma, clear cell carcinoma, large cell carcinoma with rhaboid phenotype
- Adenosquamous carcinoma
- Carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements
- Carcinomas with spindle and/or giant cells
- Pleomorphic carcinoma
- Spindle cell carcinoma
- Giant cell carcinoma
- Carcinosarcoma
- Blastoma (Pulmonary blastoma)
- Carcinoid tumor
- Typical carcinoid
- Atypical carcinoid
- Carcinomas of salivary gland type
- Mucoepidermoid carcinoma
- Adenoid cystic carcinoma
- Unclassified carcinoma
- Medication-induced bronchoconstriction
- Milk allergy
- Mobile supraglottic soft tissue
- Obesity
- Parasitic infections
- Paroxysmal vocal cord motion
- Postextubation granuloma
- Postlobectomy bronchial torsion
- Postnasal drip syndrome
- Postradiation stenosis
- Primary ciliary dyskinesia
- Psychogenic wheezing
- Pulmonary edema
- Pulmonary embolism
- Relapsing polychondritis
- Retained foreign body (trachea or esophagus)
- Retropharyngeal abscess
- Right sided aortic arch
- Supraglottitis
- Tracheal stenosis
- Tracheobronchitis
- Tracheobronchomegaly
- Tracheomalacia
- Vascular compression and rings
- Vocal cord dysfunction
- Vocal cord hematoma
- Vocal cord paralysis (bilateral paralysis)
- Wegener's granulomatosis
Complete Differential Diagnosis of the Causes of Wheeze
(By organ system)
| Cardiovascular | Cardiac asthma ( pulmonary edema), Cardiomegaly, Descending aortic aneurysm, Pulmonary edema
Pulmonary embolism, Right sided aortic arch, Vascular compression/ rings |
| Chemical / poisoning | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | Medication-induced bronchoconstriction |
| Ear Nose Throat | Aspiration(foreign particles or foods), Bilateral vocal cord paralysis, Hypertrophied tonsils, Intrathoracic goiter, Laryngeal edema, Laryngocele, Laryngostenosis, Laryngotracheobronchitis, Mobile supraglottic soft tissue, Paroxysmal vocal cord motion, Postextubation granuloma, Postlobectomy bronchial torsion, Postnasal drip syndrome, Postradiation stenosis, Retropharyngeal abscess, Supraglottitis, Vocal cord dysfunction, Vocal cord hematoma |
| Endocrine | Intrathoracic goiter, Obesity, |
| Environmental | No underlying causes |
| Gastroenterologic | Gastroesophageal Reflux Disease |
| Genetic | Cystic fibrosis, Milk allergy, Obesity, Primary ciliary dyskinesia, Vascular compression/ rings |
| Hematologic | Lymphadenopathy |
| Iatrogenic | Aspiration(foreign particles or foods), Esophageal foreign body, |
| Infectious Disease | Allergic bronchopulmonary aspergillosis, Cold induced wheezing, Bronchitis, Bronchiolitis, pneumonia, Lymphadenopathy, Retropharyngeal abscess |
| Musculoskeletal / Ortho | Cricoarytenoid arthritis, |
| Neurologic | No underlying causes |
| Nutritional / Metabolic | Obesity |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | Carcinoid syndrome, Lymphadenopathy, Lymphangitic carcinomatosis
Malignancy (bronchogenic tumors), |
| Opthalmologic | No underlying causes |
| Overdose / Toxicity | No underlying causes |
| Psychiatric | Psychogenic wheezing |
| Pulmonary | Bronchiectasis, Bronchiolitis, Bronchiolitis obliterans, Bronchitis, Bronchopulmonary dysplasia, Carcinoid syndrome, Chronic obstructive pulmonary disease: Chronic bronchitis and Emphysema, Cold induced wheezing, Cystic fibrosis, Pulmonary hemorrhage, pneumonia, Interstitial lung disease, Postlobectomy bronchial torsion, Postradiation stenosis, Primary ciliary dyskinesia, Pulmonary edema, Pulmonary embolism, Tracheal stenosis, Tracheobronchitis, Tracheobronchomegaly, Tracheomalacia, Wegener's granulomatosis |
| Renal / Electrolyte | No underlying causes |
| Rheum / Immune / Allergy | Allergic bronchopulmonary aspergillosis, Anaphylaxis, Angioedema, Asthma, Cricoarytenoid arthritis, Immunodeficiency, Interstitial lung disease, Lymphadenopathy, Milk allergy, Relapsing polychondritis, Wegener's granulomatosis |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Miscellaneous | Amyloid deposition |
Treatment of Wheeze
Management of chronic obstructive pulmonary disease (COPD)
All patients with COPD should be on a short-acting bronchodilator to be used on as-needed basis for intermittent increases in dyspnea. The purpose of the short-acting bronchodilator is to reduce symptoms and improve lung function. It is recommended to use a short-acting beta agonist plus a short-acting anticholinergic, rather than either alone, to achieve greater benefit. However, monotherapy with either is acceptable. For patients in whom intermittent short-acting bronchodilators are insufficient to control symptoms, a regularly scheduled long-acting inhaled bronchodilator is recommended. The purpose of the long-acting inhaled bronchodilator is to improve symptoms, improve lung function, and reduce the frequency of exacerbations. The effects of the currently available once daily long acting anticholinergic are superior to the effects of the twice daily long acting beta agonists that are available. Theophylline is the least preferred long-acting bronchodilator option because its effects are modest and toxicity is a concern. For patients who continue to have symptoms or repeated exacerbations despite an optimal long-acting inhaled bronchodilator regimen, adding an inhaled glucocorticoid is recommended.
All patients with COPD should be advised to quit smoking, educated about COPD, and given a yearly influenza vaccination. In addition, the pneumococcal polysaccharide vaccine should be given to patients who are ≥65 years old, or who are younger than 65 years with a forced expiratory volume in one second (FEV1) less than 40 percent.
Management of asthma
See also
References
Additional Resources
Template:Ent Baughman RP, Loudon RG. Quantitation of wheezing in acute asthma. Chest. 1984;86:718–722. PMID 6488909 Template:Ent Pasterkamp H, Asher T, Leahy F, et al. The effect of anticholinergic treatment on postexertional wheezing in asthma studied by phonopneumography and spirometry. Am Rev Respir Dis. 1985;132:16–21. PMID 3160273 Template:Ent Shim CS, Williams MH. Relationship of wheezing to the severity of obstruction in asthma. Arch Intern Med. 1983;143:890–892. PMID 6679232 Template:Ent Earis J, Marsh K, Pearson M, et al. The inspiratory squawk in extrinsic allergic alveolitis and other pulmonary fibrosis. Thorax. 1982;37:923–926. PMID 7170682 Template:Ent Meslier N, Charbonneau G, Racineux JL. Wheezes. Eur Respir J. 1995;8(11):1942-8. PMID 8620967 Template:Ent Simpson JA, Weiner ESC (eds). "stridor, n. 2." Oxford English Dictionary 2nd ed. Oxford: Clarendon Press, 1989. OED Online Oxford University Press. Accessed September 10, 2005. http://dictionary.oed.com. Template:Ent Orient JM. Sapira's Art & Science of Bedside Diagnosis 2nd ed. Philadelphia: Lippincott William Wilkins, 2000. ISBN 0-683-30714-2
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs