WBR1101: Difference between revisions
(Created page with "{{WBRQuestion |QuestionAuthor=William J Gibson |ExamType=USMLE Step 1 |MainCategory=Pathophysiology |SubCategory=Musculoskeletal/Rheumatology, Pulmonology |MainCategory=Pathop...") |
No edit summary |
||
| Line 23: | Line 23: | ||
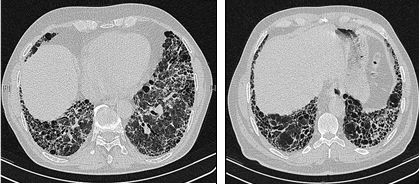
A chest CT is shown below. | A chest CT is shown below. | ||
[[File:WBR1101.jpg]] | |||
Laboratory analysis reveals the following: | Laboratory analysis reveals the following: | ||
Rheumatoid factor: Negative | Rheumatoid factor: Negative | ||
Serum Angiotensin-Converting-Enzyme: Normal | Serum Angiotensin-Converting-Enzyme: Normal | ||
Anti-nuclear antibody: Negative | Anti-nuclear antibody: Negative | ||
Erythrocyte sedimentation rate: Elevated | Erythrocyte sedimentation rate: Elevated | ||
Which of the following is the most likely diagnosis? | Which of the following is the most likely diagnosis? | ||
|Explanation=The patient in this vignette most likely has idiopathic pulmonary fibrosis (IPF). IPF is a chronic and ultimately fatal disease characterized by a progressive decline in lung function. IPF belongs to a large group of more than 200 lung diseases known as interstitial lung diseases (ILD), characterized by the involvement of lung interstitium. The interstitium, the tissue between the air sacs in the lung, is the primary site of injury in interstitial lung diseases. However, these disorders frequently affect not only the interstitium, but also the airspaces, peripheral airways, and vessels. | |Explanation=The patient in this vignette most likely has idiopathic pulmonary fibrosis (IPF). IPF is a chronic and ultimately fatal disease characterized by a progressive decline in lung function. IPF belongs to a large group of more than 200 lung diseases known as interstitial lung diseases (ILD), characterized by the involvement of lung interstitium. The interstitium, the tissue between the air sacs in the lung, is the primary site of injury in interstitial lung diseases. However, these disorders frequently affect not only the interstitium, but also the airspaces, peripheral airways, and vessels. | ||
| Line 42: | Line 47: | ||
'''References:''' | '''References:''' | ||
First Aid 2014 page 605. | First Aid 2014 page 605. | ||
|AnswerA=Sarcoidosis | |AnswerA=Sarcoidosis | ||
|AnswerAExp=Incorrect: While sarcoidosis can cause interstitial lung disease, serum ACE is typically elevated and chest CT will classically show hilar lymphadenopathy. | |AnswerAExp='''Incorrect:''' While sarcoidosis can cause interstitial lung disease, serum ACE is typically elevated and chest CT will classically show hilar lymphadenopathy. | ||
|AnswerB=Idiopathic pulmonary fibrosis | |AnswerB=Idiopathic pulmonary fibrosis | ||
|AnswerBExp=Correct: The patient in this vignette has interstitial lung disease, as evidenced by classic honeycombing pattern of the lung on chest CT. | |AnswerBExp='''Correct:''' The patient in this vignette has interstitial lung disease, as evidenced by classic honeycombing pattern of the lung on chest CT. | ||
|AnswerC=Mixed connective tissue disease | |AnswerC=Mixed connective tissue disease | ||
|AnswerCExp=Incorrect: Mixed connective tissue disease combines features of scleroderma, myositis, systemic lupus erythematosus, and rheumatoid arthritis. It is one cause of interstitial lung disease but would typically be accompanied by a positive anti-nuclear antibody. In particular, MCTD is characterized by a positive, speckled anti-nuclear antibody and an anti-U1-RNP antibody. | |AnswerCExp='''Incorrect:''' Mixed connective tissue disease combines features of scleroderma, myositis, systemic lupus erythematosus, and rheumatoid arthritis. It is one cause of interstitial lung disease but would typically be accompanied by a positive anti-nuclear antibody. In particular, MCTD is characterized by a positive, speckled anti-nuclear antibody and an anti-U1-RNP antibody. | ||
|AnswerD=Tuberculosis | |AnswerD=Tuberculosis | ||
|AnswerDExp=Incorrect: Chronic infection with mycobacterium tuberculosis can cause interstitial lung disease, but reactivation TB is most likely to be concentrated in the apices of the lung rather than the bases depicted here. | |AnswerDExp='''Incorrect:''' Chronic infection with mycobacterium tuberculosis can cause interstitial lung disease, but reactivation TB is most likely to be concentrated in the apices of the lung rather than the bases depicted here. | ||
|AnswerE=Polymyositis | |AnswerE=Polymyositis | ||
|AnswerEExp=Incorrect: Polymyositis is an autoimmune inflammatory disorder that is characterized by progressive proximal muscle weakness. Patients tend to have positive anti-nuclear antibody tests. More than 65% of patients are positive for anti-Jo antibodies. | |AnswerEExp='''Incorrect:''' Polymyositis is an autoimmune inflammatory disorder that is characterized by progressive proximal muscle weakness. Patients tend to have positive anti-nuclear antibody tests. More than 65% of patients are positive for anti-Jo antibodies. | ||
|RightAnswer=B | |RightAnswer=B | ||
|WBRKeyword=Idiopathic, Lung, Pulmonary fibrosis, Idiopathic pulmonary fibrosis, CT, | |WBRKeyword=Idiopathic, Lung, Pulmonary fibrosis, Idiopathic pulmonary fibrosis, CT, | ||
|Approved= | |Approved=Yes | ||
}} | }} | ||
Revision as of 14:46, 8 February 2014
| Author | PageAuthor::William J Gibson |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Pathophysiology |
| Sub Category | SubCategory::Musculoskeletal/Rheumatology, SubCategory::Pulmonology |
| Prompt | [[Prompt::A 55-year-old man presents to his primary care physician for progressive shortness of breath over the past year. He initially experienced difficulty on his morning runs, but now becomes dyspneic after walking as little as 10 meters (30 feet). The patient denies orthopnea and reports no history of occupational exposure to suspicious agents and he does not take any medications. Physical exam reveals diffuse crackles on lung auscultation. Pulmonary function testing demonstrates an FEV1/FVC of 90%.
A chest CT is shown below. Laboratory analysis reveals the following: Rheumatoid factor: Negative Serum Angiotensin-Converting-Enzyme: Normal Anti-nuclear antibody: Negative Erythrocyte sedimentation rate: Elevated Which of the following is the most likely diagnosis?]] |
| Answer A | AnswerA::Sarcoidosis |
| Answer A Explanation | AnswerAExp::'''Incorrect:''' While sarcoidosis can cause interstitial lung disease, serum ACE is typically elevated and chest CT will classically show hilar lymphadenopathy. |
| Answer B | AnswerB::Idiopathic pulmonary fibrosis |
| Answer B Explanation | AnswerBExp::'''Correct:''' The patient in this vignette has interstitial lung disease, as evidenced by classic honeycombing pattern of the lung on chest CT. |
| Answer C | AnswerC::Mixed connective tissue disease |
| Answer C Explanation | [[AnswerCExp::Incorrect: Mixed connective tissue disease combines features of scleroderma, myositis, systemic lupus erythematosus, and rheumatoid arthritis. It is one cause of interstitial lung disease but would typically be accompanied by a positive anti-nuclear antibody. In particular, MCTD is characterized by a positive, speckled anti-nuclear antibody and an anti-U1-RNP antibody.]] |
| Answer D | AnswerD::Tuberculosis |
| Answer D Explanation | AnswerDExp::'''Incorrect:''' Chronic infection with mycobacterium tuberculosis can cause interstitial lung disease, but reactivation TB is most likely to be concentrated in the apices of the lung rather than the bases depicted here. |
| Answer E | AnswerE::Polymyositis |
| Answer E Explanation | [[AnswerEExp::Incorrect: Polymyositis is an autoimmune inflammatory disorder that is characterized by progressive proximal muscle weakness. Patients tend to have positive anti-nuclear antibody tests. More than 65% of patients are positive for anti-Jo antibodies.]] |
| Right Answer | RightAnswer::B |
| Explanation | [[Explanation::The patient in this vignette most likely has idiopathic pulmonary fibrosis (IPF). IPF is a chronic and ultimately fatal disease characterized by a progressive decline in lung function. IPF belongs to a large group of more than 200 lung diseases known as interstitial lung diseases (ILD), characterized by the involvement of lung interstitium. The interstitium, the tissue between the air sacs in the lung, is the primary site of injury in interstitial lung diseases. However, these disorders frequently affect not only the interstitium, but also the airspaces, peripheral airways, and vessels.
Lung tissue from people with IPF shows a characteristic histopathologic pattern known as usual interstitial pneumonia (UIP). UIP is classically characterized by a “honeycombing” pattern on chest CT. Honeycombing is a lung condition defined by the presence of small cystic spaces with irregularly thickened walls composed of fibrous tissue. Interstitial lung disease and IPF in particular is characterized by honeycombing of the lower lobes of the lung. The patient in this vignette displays a progressive course of decreasing lung function consistent with pulmonary dysfunction. Normally, FEV1/FVC is approximately 80%; higher values can indicate restrictive lung disease. Because this patient has an FEV1/FVC of 90%, he likely has restrictive lung disease. The patient’s chest CT shows classic honeycombing pattern of fibrosis in the lower lobes, which is classic for interstitial lung disease. There are many causes of interstitial lung disease, but the other options are ruled out by the lnegative aboratory findings. Educational Objective: Idiopathic pulmonary fibrosis is a form of interstitial lung disease that is characterized by progressive pulmonary dysfunction and "honeycombing" appearance of the lung on CT. References:
First Aid 2014 page 605. |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Idiopathic, WBRKeyword::Lung, WBRKeyword::Pulmonary fibrosis, WBRKeyword::Idiopathic pulmonary fibrosis, WBRKeyword::CT |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |