WBR0970: Difference between revisions
Rim Halaby (talk | contribs) No edit summary |
YazanDaaboul (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor={{Rim}} | |QuestionAuthor={{Rim}} (Reviewed by {{YD}}) | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory=Biochemistry | |MainCategory=Biochemistry | ||
| Line 8: | Line 8: | ||
|MainCategory=Biochemistry | |MainCategory=Biochemistry | ||
|SubCategory=General Principles | |SubCategory=General Principles | ||
|MainCategory=Biochemistry | |||
|MainCategory=Biochemistry | |MainCategory=Biochemistry | ||
|MainCategory=Biochemistry | |MainCategory=Biochemistry | ||
| Line 20: | Line 21: | ||
|MainCategory=Biochemistry | |MainCategory=Biochemistry | ||
|SubCategory=General Principles | |SubCategory=General Principles | ||
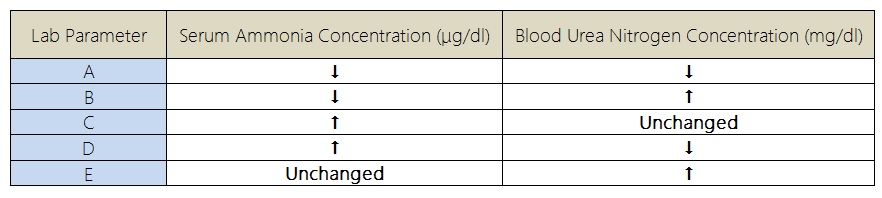
|Prompt=A | |Prompt=A 59-year-old man, with a history of chronic hepatitis C infection, presents to the physician's office with complaints of progressively worsening fatigue, loss of appetite, and bleeding tendency. Physical examination is remarkable for jaundiced skin, increase in abdominal girth, gynecomastia, and palmar erythema. The patient is asked to push his hands down on the midline of the abdomen while the examiner taps one flank, and the tap is then felt on the other flank. A set of laboratory tests is ordered. Which set of BUN and ammonia changes is associated with the patient's condition?<br> | ||
|Explanation= | |||
[[Image:WBR0970table.jpg|700px]] | |||
|Explanation=Hepatic cirrhosis should be suspected among patients with chronic hepatitis infection who present with worsening [[fatigue]], loss of appetite, and bleeding tendency (acquired coagulopathy due to reduced synthesis of coagulation factors in the liver). In this vignette, the findings on physical examination (jaundiced skin, ascites, gynecomastia, and palmar erythema) further raise the suspicion of hepatic cirrhosis. Ascites is evaluated using the fluid wave test, whereby the patient is asked to push his hands down on the midline of the abdomen while the examiner taps one flank and feels the tap at the other flank. | |||
High concentration of ammonia is toxic, and the blood concentration of ammonia is normally maintained very low. Urea is synthesized from ammonia within the periportal hepatocytes, and ammonia is further transformed into glutamine within the perivenous hepatocytes. Both processes help in the elimination of ammonia build-up in a normal liver. In [[cirrhosis]], increased hepatocyte loss and extrahepatic portosystemic shunts result in hyperammonemia caused by reduced hepatic urea synthesis. Ammonia is not converted to urea, resulting in an elevated concentration of ammonia and a reduced concentration of urea (and blood urea nitrogen). | |||
|AnswerA=A | |||
|AnswerA= | |AnswerAExp=In [[cirrhosis]], serum [[ammonia]] concentration is elevated and blood [[urea]] nitrogen concentration is reduced. | ||
|AnswerAExp= | |AnswerB=B | ||
|AnswerB= | |AnswerBExp=In [[cirrhosis]], serum [[ammonia]] concentration is elevated and blood [[urea]] nitrogen concentration is reduced. | ||
|AnswerBExp=In [[cirrhosis]], [[ | |AnswerC=C | ||
|AnswerC= | |AnswerCExp=In [[cirrhosis]], serum [[ammonia]] concentration is elevated and blood [[urea]] nitrogen concentration is reduced. | ||
|AnswerCExp= | |AnswerD=D | ||
|AnswerD= | |AnswerDExp=In [[cirrhosis]], increased hepatocyte loss and extrahepatic portosystemic shunts result in hyperammonemia caused by reduced hepatic urea synthesis. Ammonia is not converted to urea, resulting in an elevated concentration of ammonia and a reduced concentration of urea (and blood urea nitrogen). | ||
|AnswerDExp= | |AnswerE=E | ||
|AnswerE= | |AnswerEExp=In [[cirrhosis]], serum [[ammonia]] concentration is elevated and blood [[urea]] nitrogen concentration is reduced. | ||
|AnswerEExp= | |EducationalObjectives=In [[cirrhosis]], increased hepatocyte loss and extrahepatic portosystemic shunts result in hyperammonemia caused by reduced hepatic urea synthesis. Ammonia is not converted to urea, resulting in an elevated concentration of ammonia and a reduced concentration of urea (and blood urea nitrogen). | ||
|RightAnswer= | |References=Lockwood AH, McDonald JM, Reiman RE, et al. The dynamics of ammonia metabolism in man. Effects of liver disease and hyperammonemia. J Clin Invest. 1979;63(3):449-60.<br> | ||
|WBRKeyword=Urea, | First Aid 2014 page 109, 361 | ||
|Approved= | |RightAnswer=D | ||
|WBRKeyword=Urea, Ammonia, Cirrhosis, Fluid wave test, Urea cycle, Urea synthesis, Blood urea nitrogen, BUN, Hyperammonemia | |||
|Approved=Yes | |||
}} | }} | ||
Revision as of 13:30, 10 March 2015
| Author | [[PageAuthor::Rim Halaby, M.D. [1] (Reviewed by Yazan Daaboul, M.D.)]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Biochemistry |
| Sub Category | SubCategory::General Principles |
| Prompt | [[Prompt::A 59-year-old man, with a history of chronic hepatitis C infection, presents to the physician's office with complaints of progressively worsening fatigue, loss of appetite, and bleeding tendency. Physical examination is remarkable for jaundiced skin, increase in abdominal girth, gynecomastia, and palmar erythema. The patient is asked to push his hands down on the midline of the abdomen while the examiner taps one flank, and the tap is then felt on the other flank. A set of laboratory tests is ordered. Which set of BUN and ammonia changes is associated with the patient's condition? |
| Answer A | AnswerA::A |
| Answer A Explanation | [[AnswerAExp::In cirrhosis, serum ammonia concentration is elevated and blood urea nitrogen concentration is reduced.]] |
| Answer B | AnswerB::B |
| Answer B Explanation | [[AnswerBExp::In cirrhosis, serum ammonia concentration is elevated and blood urea nitrogen concentration is reduced.]] |
| Answer C | AnswerC::C |
| Answer C Explanation | [[AnswerCExp::In cirrhosis, serum ammonia concentration is elevated and blood urea nitrogen concentration is reduced.]] |
| Answer D | AnswerD::D |
| Answer D Explanation | [[AnswerDExp::In cirrhosis, increased hepatocyte loss and extrahepatic portosystemic shunts result in hyperammonemia caused by reduced hepatic urea synthesis. Ammonia is not converted to urea, resulting in an elevated concentration of ammonia and a reduced concentration of urea (and blood urea nitrogen).]] |
| Answer E | AnswerE::E |
| Answer E Explanation | [[AnswerEExp::In cirrhosis, serum ammonia concentration is elevated and blood urea nitrogen concentration is reduced.]] |
| Right Answer | RightAnswer::D |
| Explanation | [[Explanation::Hepatic cirrhosis should be suspected among patients with chronic hepatitis infection who present with worsening fatigue, loss of appetite, and bleeding tendency (acquired coagulopathy due to reduced synthesis of coagulation factors in the liver). In this vignette, the findings on physical examination (jaundiced skin, ascites, gynecomastia, and palmar erythema) further raise the suspicion of hepatic cirrhosis. Ascites is evaluated using the fluid wave test, whereby the patient is asked to push his hands down on the midline of the abdomen while the examiner taps one flank and feels the tap at the other flank.
High concentration of ammonia is toxic, and the blood concentration of ammonia is normally maintained very low. Urea is synthesized from ammonia within the periportal hepatocytes, and ammonia is further transformed into glutamine within the perivenous hepatocytes. Both processes help in the elimination of ammonia build-up in a normal liver. In cirrhosis, increased hepatocyte loss and extrahepatic portosystemic shunts result in hyperammonemia caused by reduced hepatic urea synthesis. Ammonia is not converted to urea, resulting in an elevated concentration of ammonia and a reduced concentration of urea (and blood urea nitrogen). |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Urea, WBRKeyword::Ammonia, WBRKeyword::Cirrhosis, WBRKeyword::Fluid wave test, WBRKeyword::Urea cycle, WBRKeyword::Urea synthesis, WBRKeyword::Blood urea nitrogen, WBRKeyword::BUN, WBRKeyword::Hyperammonemia |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |