WBR0922: Difference between revisions
Jump to navigation
Jump to search
(Created page with "{{WBRQuestion |QuestionAuthor=Vendhan Ramanujam |ExamType=USMLE Step 3 |MainCategory=Inpatient Facilities |SubCategory=Gastrointestinal |MainCategory=Inpatient Facilities |Sub...") |
m (refreshing WBR questions) |
||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor=Vendhan Ramanujam | |QuestionAuthor=Vendhan Ramanujam | ||
|ExamType=USMLE Step 3 | |ExamType=USMLE Step 3 | ||
Latest revision as of 02:05, 28 October 2020
| Author | PageAuthor::Vendhan Ramanujam |
|---|---|
| Exam Type | ExamType::USMLE Step 3 |
| Main Category | MainCategory::Inpatient Facilities |
| Sub Category | SubCategory::Gastrointestinal |
| Prompt | [[Prompt::A 35 year old male is admitted following a complaint of progressive dysphagia for the past three weeks. He has dysphagia for both solids and liquids. There is no history of fever or odynophagia. He denies any history of vomiting and weight loss. He has a past history of severe upper abdominal pain that lasted for 2 days following a binge of alcohol 2 months back and it relieved with symptomatic treatment. Physical examination is unremarkable and vitals are stable. His lab tests are normal except for elevated serum amylase and lipase levels. An endoscopy showed stasis at the lower end of esophagus with an extrinsic compression of the lower esophagus and an ultrasound abdomen showed a cystic lesion of 10 cm diameter in the upper abdomen in close relation to the tail region of the pancreas. A following abdominal CT showed the same cystic lesion with internal septae at the same location with similar size.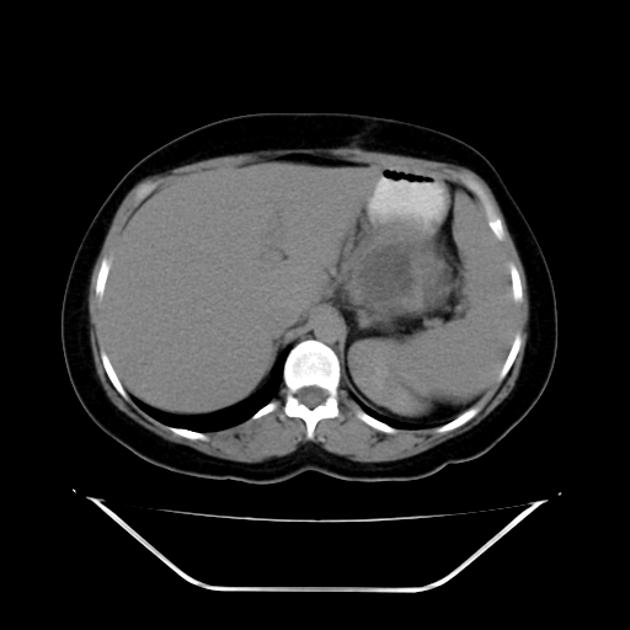 What will be the next best step in the line of management of this patient?]] |
| Answer A | AnswerA::Endoscopic ultrasonography or CT guided aspiration of the cyst |
| Answer A Explanation | [[AnswerAExp::Correct-In the absence of a history or signs of acute or chronic pancreatitis or pancreatic trauma, in the absence of associated inflammatory changes on CT scan and in the presence of internal septae within the cyst cavity, pancreatic cystic neoplasms should be considered as a differential diagnosis to pancreatic pseudocyst and should be followed with either endoscopic ultrasonography or CT guided aspiration of cyst for differentiating the both and to plan the management accordingly.]] |
| Answer B | AnswerB::Observation for the next 3 weeks |
| Answer B Explanation | AnswerBExp::'''Incorrect'''-After confirming a pseudocyst, uncomplicated pseudocysts smaller than 5 cm should be observed for 6 weeks before further therapeutic intervention. |
| Answer C | AnswerC::Percutaneous catheter drainage of the cyst |
| Answer C Explanation | [[AnswerCExp::Incorrect-Non resolving pseudocysts after a period of 6 weeks observation, pseudocysts larger than 5 cm and complicated pseudocysts should be drained by either percutaneous catheter or endoscopic gastrostomy or laparoscopic gastrostomy drainage.]] |
| Answer D | AnswerD::Endoscopic gastrostomy and drainage of the cyst |
| Answer D Explanation | [[AnswerDExp::Incorrect-Non resolving pseudocysts after a period of 6 weeks observation, pseudocysts larger than 5 cm and complicated pseudocysts should be drained by either percutaneous catheter or endoscopic gastrostomy or laparoscopic gastrostomy drainage.]] |
| Answer E | AnswerE::Laparoscopic gastrostomy and drainage of the cyst |
| Answer E Explanation | [[AnswerEExp::Incorrect-Non resolving pseudocysts after a period of 6 weeks observation, pseudocysts larger than 5 cm and complicated pseudocysts should be drained by either percutaneous catheter or endoscopic gastrostomy or laparoscopic gastrostomy drainage.]] |
| Right Answer | RightAnswer::A |
| Explanation | [[Explanation::The patient is suffering from dysphagia due to external compression of the lower esophagus by a cyst arising from the tail of the pancreas. Pancreatic pseudocysts can occur following an attack of acute pancreatitis as in this case, in patients with chronic pancreatitis, and in patients who have suffered blunt or penetrating trauma. The diagnosis of a pancreatic pseudocyst can be made by compatible imaging results in the appropriate clinical context. However, the differential diagnosis includes pancreatic cystic neoplasms, especially in the absence of a history or signs of acute or chronic pancreatitis or pancreatic trauma, in the absence of associated inflammatory changes on CT scan and in the presence of internal septae within the cyst cavity. Endoscopic ultrasonography or CT guided aspiration of the cyst should be done to find the diagnosis and plan the management accordingly.
Educational Objective:
In the absence of a history or signs of acute or chronic pancreatitis or pancreatic trauma, in the absence of associated inflammatory changes on CT scan and in the presence of internal septae within the cyst cavity, pancreatic cystic neoplasms should be considered as a differential diagnosis to pancreatic pseudocyst and should be followed with either endoscopic ultrasonography or CT guided aspiration of cyst for differentiating the both and to plan the management accordingly. |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Pancreatic mucinous cystadenoma, WBRKeyword::acute pancreatitis, WBRKeyword::pancreatic pseudocyst |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |