WBR0752: Difference between revisions
Jump to navigation
Jump to search
Rim Halaby (talk | contribs) (Created page with "{{WBRQuestion |QuestionAuthor={{Rim}} |ExamType=USMLE Step 1 |MainCategory=Pathology |SubCategory=Musculoskeletal/Rheumatology |MainCategory=Pathology |SubCategory=Musculoskel...") |
YazanDaaboul (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor={{ | |QuestionAuthor={{YD}} (Reviewed by {{YD}}) | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory=Pathology | |MainCategory=Pathology | ||
| Line 8: | Line 8: | ||
|MainCategory=Pathology | |MainCategory=Pathology | ||
|SubCategory=Musculoskeletal/Rheumatology | |SubCategory=Musculoskeletal/Rheumatology | ||
|MainCategory=Pathology | |||
|MainCategory=Pathology | |MainCategory=Pathology | ||
|MainCategory=Pathology | |MainCategory=Pathology | ||
| Line 20: | Line 21: | ||
|MainCategory=Pathology | |MainCategory=Pathology | ||
|SubCategory=Musculoskeletal/Rheumatology | |SubCategory=Musculoskeletal/Rheumatology | ||
|Prompt=A 27 year old man | |Prompt=A 27-year-old man with no past medical history presents to the physician's office for recurrent left knee pain. The patient explains that he has recently received antibiotics to treat a urethral infection 2 weeks ago. He reports his current knee pain does not involve his right knee and is moderately relieved with administration of naproxen. Work-up is remarkable for elevated concentration of C-reactive protein (CRP) and a markedly elevated HLA-B27 surface antigen. Which of the following findings on physical examination is most associated with this patient's condition? | ||
|Explanation= | |Explanation=Reactive arthritis (ReA or Reiter's syndrome) is an autoimmune inflammatory arthritis. Infection with either ''Chlamydia'', ''Salmonella'', ''Shigella'', or ''Campylobacter'' is strongly associated with the development of ReA. ReA typically manifests with mono-inflammatory, non-migratory, arthritic pain 2 to 4 weeks following a gastrointestinal or a urethral infection. Laboratroy findings are usually unremarkable except for elevated concentrations of acute phase reactants, such as CRP and ESR. ReA is a subtype of seronegative spondyloarthropathies (arthritis with negative RF) that is associated with HLA-B27 class I surface antigen. The classic triad of ReA manifestations is conjunctivitis, urethritis, and arthritis [Mnemonic: Can't see (conjunctivitis), can't pee (urethritis), can't climb a tree (arthritis)]. The diagnosis of ReA is clinical, and treatment includes NSAIDs for symptomatic relief in most of the cases until the pain self-resolves. However, rare refractory cases might require either intra-articular, systemic steroids, or disease-modifying antirheumatic drugs (DMARDs).<br> | ||
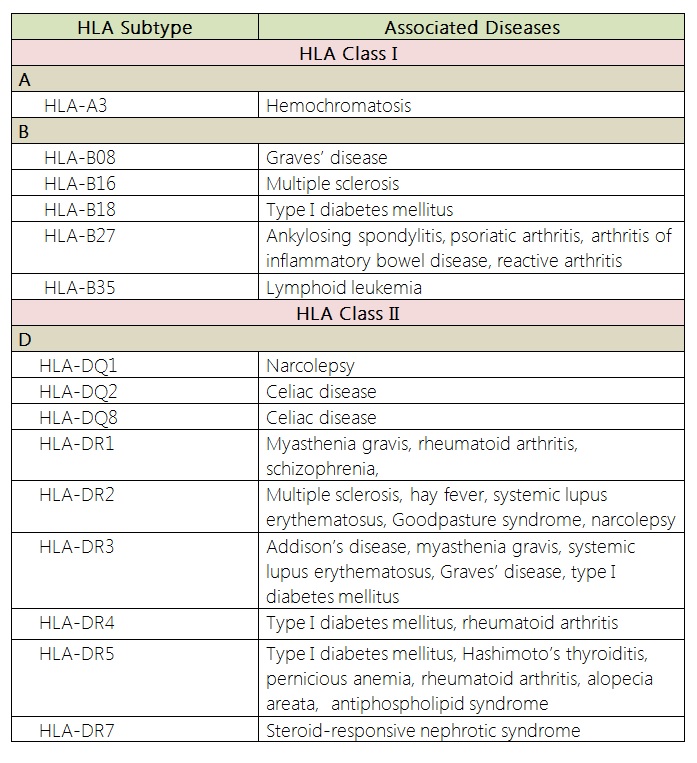
Common HLA subtypes and their associated diseases are shown in the table below.<br> | |||
[[Image:HLA subtypes and associated diseases.jpg|600px]] | |||
|AnswerA=Conjunctival redness | |||
The classic triad of ReA is | |AnswerAExp=Manifestations of reactive arthritis are summarized by the classic triad of conjunctivitis, urethritis, and arthritis. | ||
|AnswerB=Systolic ejection murmur | |||
The diagnosis of ReA is | |AnswerBExp=Aortic stenosis is not common among patients with reactive arthritis. However, ankylosing spondylitis, also a seronegative spondyloarthropathy, is associated with aortic regurgitation. | ||
|AnswerC=Facial rash that spares the nasolabial folds | |||
|AnswerCExp=Malar rash is characteristic of systemic lupus erythematosus. | |||
|AnswerD=Violaceous eruption on the upper eyelids | |||
|AnswerDExp=Heliotrope rash is characteristic of dermatomyositis. | |||
|AnswerE=Excoriated papules on the dorsum of the hands | |||
|AnswerEExp=Skin excoriation is not associated with reactive arthritis. | |||
|AnswerA= | |EducationalObjectives=Reactive arthritis (ReA or Reiter's syndrome) is an autoimmune inflammatory arthritis. Infection with either ''Chlamydia'', ''Salmonella'', ''Shigella'', or ''Campylobacter'' is strongly associated with the development of ReA. ReA typically manifests with mono-inflammatory, non-migratory, arthritic pain 2 to 4 weeks following a gastrointestinal or a urethral infection. Reactive arthritis manifestations are the triad of conjunctivitis, urethritis, and arthritis. | ||
|AnswerAExp= | |References=Kim PS, Klausmeier TL, Orr DP. Reactive arthritis: a review. J Adolesc Health. 2009;44(4):309-15.<br> | ||
|AnswerB= | First Aid 2014 page 426 | ||
|AnswerBExp=Aortic stenosis is not | |||
|AnswerC= | |||
|AnswerCExp=Malar rash is | |||
|AnswerD= | |||
|AnswerDExp=Heliotrope rash is | |||
|AnswerE= | |||
|AnswerEExp=Skin excoriation is not | |||
|RightAnswer=A | |RightAnswer=A | ||
|WBRKeyword= | |WBRKeyword=Reactive arthritis, Seronegative spondyloarthropathies, HLA-B27, HLA subtypes, Conjunctival redness, Conjunctivitis, Urethritis, Arthritis, Autoimmune, Inflammatory arthritis, | ||
|Approved= | |Approved=Yes | ||
}} | }} | ||
Revision as of 20:36, 6 March 2015
| Author | [[PageAuthor::Yazan Daaboul, M.D. (Reviewed by Yazan Daaboul, M.D.)]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Pathology |
| Sub Category | SubCategory::Musculoskeletal/Rheumatology |
| Prompt | [[Prompt::A 27-year-old man with no past medical history presents to the physician's office for recurrent left knee pain. The patient explains that he has recently received antibiotics to treat a urethral infection 2 weeks ago. He reports his current knee pain does not involve his right knee and is moderately relieved with administration of naproxen. Work-up is remarkable for elevated concentration of C-reactive protein (CRP) and a markedly elevated HLA-B27 surface antigen. Which of the following findings on physical examination is most associated with this patient's condition?]] |
| Answer A | AnswerA::Conjunctival redness |
| Answer A Explanation | AnswerAExp::Manifestations of reactive arthritis are summarized by the classic triad of conjunctivitis, urethritis, and arthritis. |
| Answer B | AnswerB::Systolic ejection murmur |
| Answer B Explanation | AnswerBExp::Aortic stenosis is not common among patients with reactive arthritis. However, ankylosing spondylitis, also a seronegative spondyloarthropathy, is associated with aortic regurgitation. |
| Answer C | AnswerC::Facial rash that spares the nasolabial folds |
| Answer C Explanation | AnswerCExp::Malar rash is characteristic of systemic lupus erythematosus. |
| Answer D | AnswerD::Violaceous eruption on the upper eyelids |
| Answer D Explanation | AnswerDExp::Heliotrope rash is characteristic of dermatomyositis. |
| Answer E | AnswerE::Excoriated papules on the dorsum of the hands |
| Answer E Explanation | AnswerEExp::Skin excoriation is not associated with reactive arthritis. |
| Right Answer | RightAnswer::A |
| Explanation | [[Explanation::Reactive arthritis (ReA or Reiter's syndrome) is an autoimmune inflammatory arthritis. Infection with either Chlamydia, Salmonella, Shigella, or Campylobacter is strongly associated with the development of ReA. ReA typically manifests with mono-inflammatory, non-migratory, arthritic pain 2 to 4 weeks following a gastrointestinal or a urethral infection. Laboratroy findings are usually unremarkable except for elevated concentrations of acute phase reactants, such as CRP and ESR. ReA is a subtype of seronegative spondyloarthropathies (arthritis with negative RF) that is associated with HLA-B27 class I surface antigen. The classic triad of ReA manifestations is conjunctivitis, urethritis, and arthritis [Mnemonic: Can't see (conjunctivitis), can't pee (urethritis), can't climb a tree (arthritis)]. The diagnosis of ReA is clinical, and treatment includes NSAIDs for symptomatic relief in most of the cases until the pain self-resolves. However, rare refractory cases might require either intra-articular, systemic steroids, or disease-modifying antirheumatic drugs (DMARDs). Common HLA subtypes and their associated diseases are shown in the table below. |
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Reactive arthritis, WBRKeyword::Seronegative spondyloarthropathies, WBRKeyword::HLA-B27, WBRKeyword::HLA subtypes, WBRKeyword::Conjunctival redness, WBRKeyword::Conjunctivitis, WBRKeyword::Urethritis, WBRKeyword::Arthritis, WBRKeyword::Autoimmune, WBRKeyword::Inflammatory arthritis |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |