Traumatic diaphragmatic hernia: Difference between revisions
AwniShahait (talk | contribs) No edit summary |
AwniShahait (talk | contribs) No edit summary |
||
| Line 33: | Line 33: | ||
==Diagnosis== | ==Diagnosis== | ||
Diaphragmatic ruptures present in two ways. In the acute form, the patient has recently experienced blunt trauma or a penetrating wound to the chest, abdomen, or back. The clinical manifestations are essentially those of the associated injuries, but occasionally, massive herniation of abdominal viscera through the diaphragm causes respiratory insufficiency. | |||
In the chronic form, the diaphragmatic tear is unrecognized at the time of the original injury. Some time later, symptoms appear from herniation of viscera: pain, bowel obstruction, etc. Respiratory symptoms in such cases are rare. | |||
The grading of severity has been proposed by Grimes,<ref name="pmid4843862">{{cite journal |author=Grimes OF |title=Traumatic injuries of the diaphragm. Diaphragmatic hernia |journal=Am. J. Surg. |volume=128 |issue=2 |pages=175–81 |year=1974 |month=August |pmid=4843862 |doi= |url=}}</ref> who discussed diaphragmatic rupture in phases: acute, latent and the obstructive phase. The acute presentation is in the patient with poly trauma associated with multiple intra abdominal and chest injuries. The latent phase is when herniation occurs through undetected diaphragmatic ruptures and rents. The obstructive phase is when the loop herniating obstructs and the patient develops distension and strangulation. | |||
===Investigation=== | |||
Plain films of the chest may show a radiopaque area and occasionally an air-fluid level if hollow viscera have herniated. If the stomach has entered the chest, the abnormal path of a nasogastric tube may be diagnostic. The collar sign is seen when abdominal contents are seen in the thorax with/without focal constriction. Elevation and distortion of the hemi diaphragm are corroborative signs.<ref name="pmid9460108">{{cite journal |author=Shackleton KL, Stewart ET, Taylor AJ |title=Traumatic diaphragmatic injuries: spectrum of radiographic findings |journal=Radiographics |volume=18 |issue=1 |pages=49–59 |year=1998 |pmid=9460108 |doi= |url=}}</ref> | |||
Ultrasonography, CT scan, and MRI may demonstrate the diaphragmatic rent. A CT thorax has a sensitivity of 14-82% and a specificity of 87% and permits direct visualization of the contents and the rupture.Focussed abdominal sonography for trauma(FAST) is now a good aid in diagnosing diaphragmatic hernia.<ref name="pmid15666270">{{cite journal |author=Blaivas M, Brannam L, Hawkins M, Lyon M, Sriram K |title=Bedside emergency ultrasonographic diagnosis of diaphragmatic rupture in blunt abdominal trauma |journal=Am J Emerg Med |volume=22 |issue=7 |pages=601–4 |year=2004 |month=November |pmid=15666270 |doi= |url=}}</ref> Barium study of the colon may show irregular patches of barium in the colon above the diaphragm or a smooth colonic outline if the colon does not contain feces. | |||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
Traumatic rupture of the diaphragm must be differentiated from atelectasis, space-consuming tumors of the lower pleural space, pleural effusion, and intestinal obstruction due to other causes. | |||
==Complications== | ==Complications== | ||
Hemorrhage and obstruction may occur. If herniation is massive, progressive cardiorespiratory insufficiency may threaten life. The most severe complication is strangulating obstruction of the herniated viscera. | |||
==Treatment== | ==Treatment== | ||
For acute ruptures, a transabdominal (most commonly) or transthoracic route is used depending on the procedure required to treat ancillary injuries. When the diaphragmatic tear is the only injury, it is usually fixed by laparotomy. Chronic injuries can be repaired by either approach. Asymptomatic tears of the diaphragm with herniated viscera should be repaired, because the risk of strangulating obstruction is high. | |||
==Prognosis== | ==Prognosis== | ||
Surgical repair of the rent in the diaphragm is curative, and the prognosis is excellent. The diaphragm supports sutures well, so that recurrence is practically unknown. | |||
==See also== | ==See also== | ||
Revision as of 14:41, 21 April 2012
| Traumatic diaphragmatic hernia | |
 | |
|---|---|
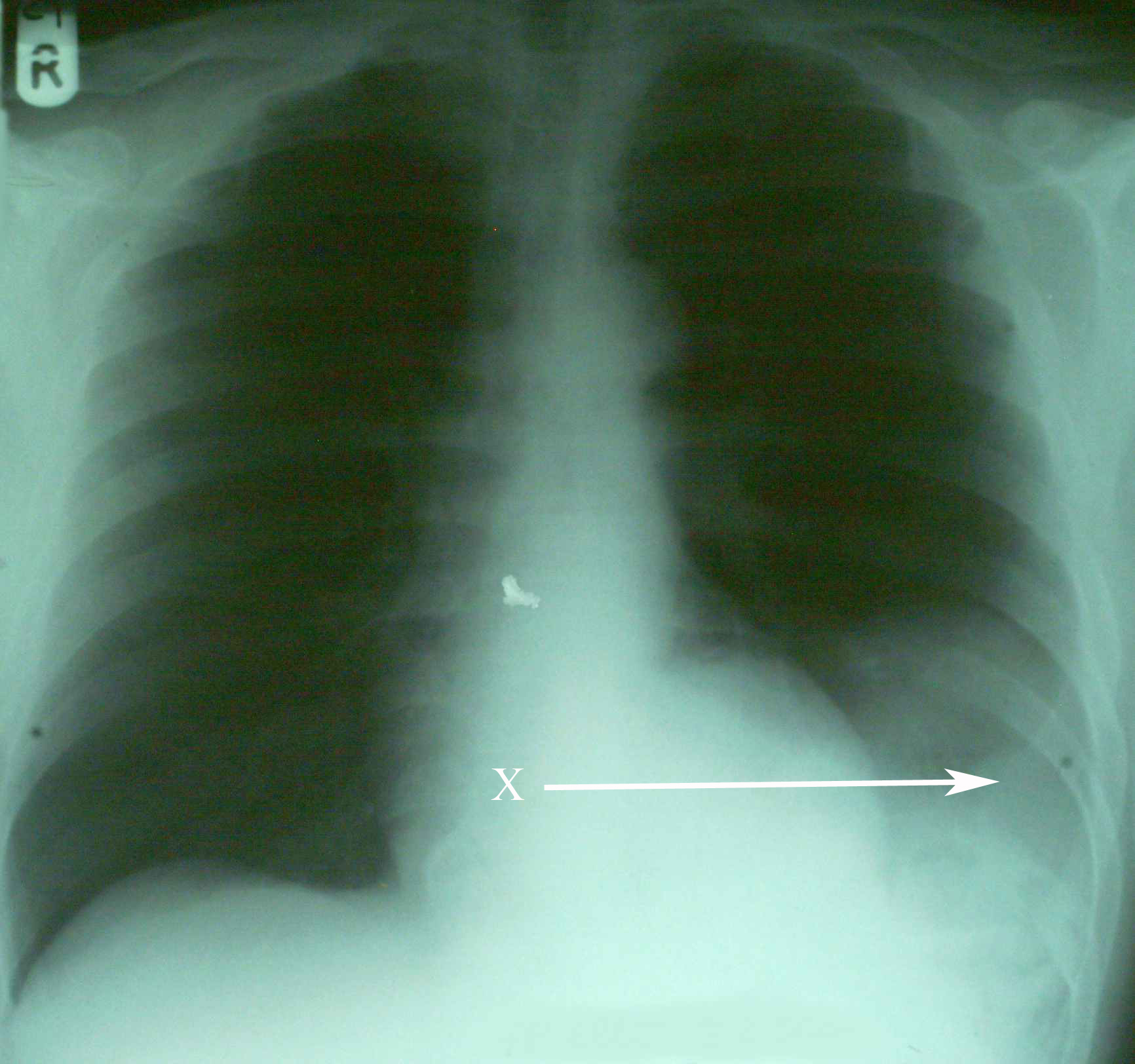
| An X-ray showing the spleen in the left lower portion of the chest cavity (X and arrow) after a diaphragmatic tear[1] | |
| ICD-9 | 862.0 |
| eMedicine | med/3487 |
| MeSH | D006549 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
A traumatic diaphragmatic hernia is a type of diaphragmatic hernia which is acquired through an abdominal injury. This is in contrast to a congenital diaphragmatic hernia, which is present from birth.
Diaphragmatic injury accounts for 0.8-1.6% of blunt trauma abdomen. Approximately 4-6% of patients who undergo surgery for trauma have a diaphragmatic injury.[2]
Historical Perspective
Traumatic diaphragmatic hernia apparently was described by Sennertus, who in 1541 reported an instance of delayed herniation of viscera through an injured diaphragm.[3] Ambroise Paré, in 1579, described the first case of diaphragmatic rupture diagnosed at autopsy. The first successful diaphragmatic repair was reported by Riolfi in 1886 in a patient with omental prolapse, and Naumann in 1888 repaired the defect with herniated stomach.
Pathophysiology
Diaphragmatic injuries are caused either by penetrating or blunt injuries to the abdomen. They are diagnosed immediately as part of multi-organ injury, or present later either with respiratory distress or as intestinal obstruction.[4] The mechanism in blunt injury is explained by shearing of a stretched membrane, avulsion at the point of diaphragmatic attachment, and the sudden force transmission through viscera acting as viscous fluid. Left sided injuries are more often seen. Left-sided rupture occurred in 68.5% of the patients, 24.2% had right-sided rupture, 1.5% had bilateral rupture, 0.9% had pericardial rupture, and 4.9% were unclassified.[2] Increased strength of the right hemi-diaphragm, hepatic protection of the right side, under diagnosis of right-sided ruptures, and weakness of the left hemi-diaphragm at points of embryonic fusion all have been proposed to explain the predominance of left sided diaphragmatic injuries.[2] Autopsy studies reveals that the incidence of rupture is almost equal on both sides but the greater force needed for the right rupture. A positive pressure gradient of 7-20 cms of H2O between the intraperitoneal and the intra pleural cavities forces the contents into the thorax. With severe blunt trauma the pressures may rise to as high as 100cms of water.
It can occur after splenectomy.[5]
Because it can be indicative of severe trauma, it often co-presents with pelvic fracture.[6]
Diagnosis
Diaphragmatic ruptures present in two ways. In the acute form, the patient has recently experienced blunt trauma or a penetrating wound to the chest, abdomen, or back. The clinical manifestations are essentially those of the associated injuries, but occasionally, massive herniation of abdominal viscera through the diaphragm causes respiratory insufficiency.
In the chronic form, the diaphragmatic tear is unrecognized at the time of the original injury. Some time later, symptoms appear from herniation of viscera: pain, bowel obstruction, etc. Respiratory symptoms in such cases are rare.
The grading of severity has been proposed by Grimes,[7] who discussed diaphragmatic rupture in phases: acute, latent and the obstructive phase. The acute presentation is in the patient with poly trauma associated with multiple intra abdominal and chest injuries. The latent phase is when herniation occurs through undetected diaphragmatic ruptures and rents. The obstructive phase is when the loop herniating obstructs and the patient develops distension and strangulation.
Investigation
Plain films of the chest may show a radiopaque area and occasionally an air-fluid level if hollow viscera have herniated. If the stomach has entered the chest, the abnormal path of a nasogastric tube may be diagnostic. The collar sign is seen when abdominal contents are seen in the thorax with/without focal constriction. Elevation and distortion of the hemi diaphragm are corroborative signs.[8]
Ultrasonography, CT scan, and MRI may demonstrate the diaphragmatic rent. A CT thorax has a sensitivity of 14-82% and a specificity of 87% and permits direct visualization of the contents and the rupture.Focussed abdominal sonography for trauma(FAST) is now a good aid in diagnosing diaphragmatic hernia.[9] Barium study of the colon may show irregular patches of barium in the colon above the diaphragm or a smooth colonic outline if the colon does not contain feces.
Differential Diagnosis
Traumatic rupture of the diaphragm must be differentiated from atelectasis, space-consuming tumors of the lower pleural space, pleural effusion, and intestinal obstruction due to other causes.
Complications
Hemorrhage and obstruction may occur. If herniation is massive, progressive cardiorespiratory insufficiency may threaten life. The most severe complication is strangulating obstruction of the herniated viscera.
Treatment
For acute ruptures, a transabdominal (most commonly) or transthoracic route is used depending on the procedure required to treat ancillary injuries. When the diaphragmatic tear is the only injury, it is usually fixed by laparotomy. Chronic injuries can be repaired by either approach. Asymptomatic tears of the diaphragm with herniated viscera should be repaired, because the risk of strangulating obstruction is high.
Prognosis
Surgical repair of the rent in the diaphragm is curative, and the prognosis is excellent. The diaphragm supports sutures well, so that recurrence is practically unknown.
See also
References
- ↑ Hariharan D, Singhal R, Kinra S, Chilton A (2006). "Post traumatic intra thoracic spleen presenting with upper GI bleed! A case report". BMC Gastroenterol. 6: 38. doi:10.1186/1471-230X-6-38. PMC 1687187. PMID 17132174.
- ↑ 2.0 2.1 2.2 Ala-Kulju K, Verkkala K, Ketonen P, Harjola PT (1986). "Traumatic rupture of the right hemidiaphragm". Scand J Thorac Cardiovasc Surg. 20 (2): 109–14. PMID 3738439.
- ↑ Shah R, Sabanathan S, Mearns AJ, Choudhury AK (1995). "Traumatic rupture of diaphragm". Ann. Thorac. Surg. 60 (5): 1444–9. doi:10.1016/0003-4975(95)00629-Y. PMID 8526655. Unknown parameter
|month=ignored (help) - ↑ CARTER BN, GIUSEFFI J, FELSON B (1951). "Traumatic diaphragmatic hernia". Am J Roentgenol Radium Ther. 65 (1): 56–72. PMID 14799666. Unknown parameter
|month=ignored (help) - ↑ Tsuboi K, Omura N, Kashiwagi H, Kawasaki N, Suzuki Y, Yanaga K (2008). "Delayed traumatic diaphragmatic hernia after open splenectomy: report of a case". Surg. Today. 38 (4): 352–4. doi:10.1007/s00595-007-3627-0. PMID 18368327.
- ↑ Meyers BF, McCabe CJ (1993). "Traumatic diaphragmatic hernia. Occult marker of serious injury". Ann. Surg. 218 (6): 783–90. PMC 1243075. PMID 8257229. Unknown parameter
|month=ignored (help) - ↑ Grimes OF (1974). "Traumatic injuries of the diaphragm. Diaphragmatic hernia". Am. J. Surg. 128 (2): 175–81. PMID 4843862. Unknown parameter
|month=ignored (help) - ↑ Shackleton KL, Stewart ET, Taylor AJ (1998). "Traumatic diaphragmatic injuries: spectrum of radiographic findings". Radiographics. 18 (1): 49–59. PMID 9460108.
- ↑ Blaivas M, Brannam L, Hawkins M, Lyon M, Sriram K (2004). "Bedside emergency ultrasonographic diagnosis of diaphragmatic rupture in blunt abdominal trauma". Am J Emerg Med. 22 (7): 601–4. PMID 15666270. Unknown parameter
|month=ignored (help)
Template:Injuries, other than fractures, dislocations, sprains and strains
Template:SIB
Template:WH
Template:WikiDoc Sources