Transitional cell carcinoma natural history, complications and prognosis: Difference between revisions
| Line 50: | Line 50: | ||
*Depending on the stage and grade of the tumor at the time of diagnosis, the prognosis may vary. However, the 5-year survival rate of patients with upper urinary tract transitional cell carcinoma is approximately 75%.<ref name="pmid11025695">{{cite journal| author=Munoz JJ, Ellison LM| title=Upper tract urothelial neoplasms: incidence and survival during the last 2 decades. | journal=J Urol | year= 2000 | volume= 164 | issue= 5 | pages= 1523-5 | pmid=11025695 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11025695 }} </ref> | *Depending on the stage and grade of the tumor at the time of diagnosis, the prognosis may vary. However, the 5-year survival rate of patients with upper urinary tract transitional cell carcinoma is approximately 75%.<ref name="pmid11025695">{{cite journal| author=Munoz JJ, Ellison LM| title=Upper tract urothelial neoplasms: incidence and survival during the last 2 decades. | journal=J Urol | year= 2000 | volume= 164 | issue= 5 | pages= 1523-5 | pmid=11025695 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11025695 }} </ref> | ||
*The major prognostic factor at the time of diagnosis of upper tract transitional cell cancer is the depth of infiltration into or through the uroepithelial wall. | *The major prognostic factor at the time of diagnosis of upper tract transitional cell cancer is the depth of infiltration into or through the uroepithelial wall. | ||
*Most superficial tumors are likely to be well differentiated, while infiltrative tumors are likely to be poorly differentiated. | *Most superficial tumors are likely to be well differentiated, while infiltrative tumors are likely to be poorly differentiated.ref name= NIH>Transitional cell cancer. National cancer institute. http://www.cancer.gov/types/kidney/hp/transitional-cell-treatment-pdq#section/_1</ref> | ||
*They are curable in more than 90% of patients if they are superficial and confined to the renal pelvis or ureter. | *They are curable in more than 90% of patients if they are superficial and confined to the renal pelvis or ureter. | ||
*Patients with deeply invasive tumors that are still confined to the renal pelvis or ureter have a 10% to 15% likelihood of cure. | *Patients with deeply invasive tumors that are still confined to the renal pelvis or ureter have a 10% to 15% likelihood of cure. | ||
*Patients with tumors with penetration through the urothelial wall or with distant metastases usually cannot be cured with currently available forms of treatment. | *Patients with tumors with penetration through the urothelial wall or with distant metastases usually cannot be cured with currently available forms of treatment. | ||
*When involvement of the upper tract is diffuse (involving both the renal pelvis and ureter), the likelihood of subsequent development of bladder cancer increases to 75%. | *When involvement of the upper tract is diffuse (involving both the renal pelvis and ureter), the likelihood of subsequent development of bladder cancer increases to 75%. | ||
*DNA ploidy has not added significant prognostic information beyond that provided by stage and grade. | *DNA ploidy has not added significant prognostic information beyond that provided by stage and grade. | ||
==References== | ==References== | ||
Revision as of 14:29, 22 February 2016
|
Transitional cell carcinoma Microchapters |
|
Differentiating Transitional cell carcinoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Transitional cell carcinoma natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Transitional cell carcinoma natural history, complications and prognosis |
|
FDA on Transitional cell carcinoma natural history, complications and prognosis |
|
CDC on Transitional cell carcinoma natural history, complications and prognosis |
|
Transitional cell carcinoma natural history, complications and prognosis in the news |
|
Blogs on Transitional cell carcinoma natural history, complications and prognosis |
|
Directions to Hospitals Treating Transitional cell carcinoma |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Natural History
Complications
Bladder cancers may spread into the nearby organs. They may also travel through the pelvic lymph nodes and spread to the liver, lungs, and bones. Additional complications of bladder cancer include:
- Anemia
- Swelling of the ureters(hydronephrosis)
- Urethral stricture
- Urinary incontinence
- The incidence of synchronous or metachronous contralateral upper tract cancers ranges from 2% to 4%; the incidence of subsequent bladder cancer after prior upper tract transitional cell cancer ranges from 30% to 50%.
Prognosis
Transitional cell carcinoma of bladder
- Based on data from 2005-2011, the 5-year survival rate of patients with bladder cancer is approximately 77.4%.[1]
- Between 2004 and 2010, the 5-year relative survival of patients with bladder cancer was 79.1%.[2]
- When stratified by age, the 5-year relative survival of patients with bladder cancer was 83.8% and 74.1% for patients <65 and ≥ 65 years of age respectively.[2]
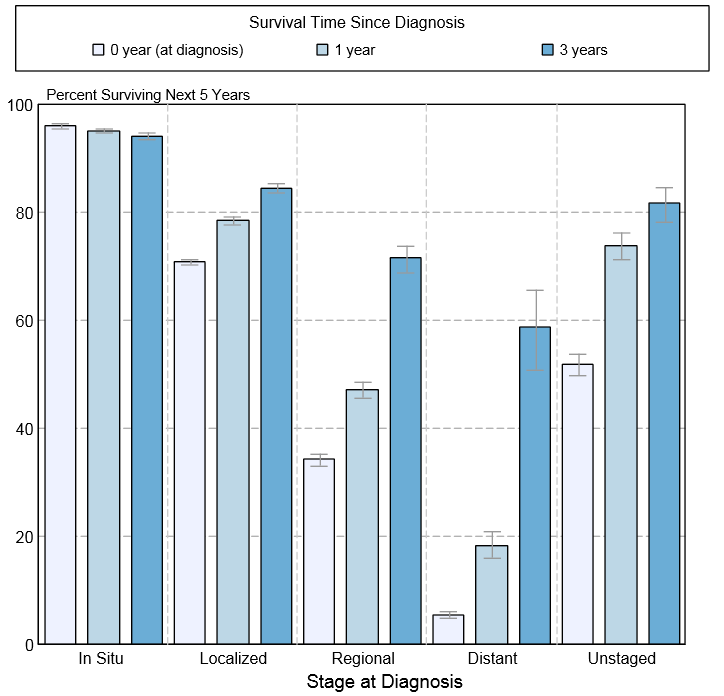
- The survival of patients with bladder cancer varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of bladder cancer:[2]
| Stage | 5-year relative survival (%), (2004-2010) |
| All stages | 77.4% |
| In situ | 96.2% |
| Localized | 69.2% |
| Regional | 33.7% |
| Distant | 5.5% |
| Unstaged | 48.7% |
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 2004 and 2010 of bladder cancer by stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[2]
Transitional cell carcinoma of upper urinary tract
- Depending on the stage and grade of the tumor at the time of diagnosis, the prognosis may vary. However, the 5-year survival rate of patients with upper urinary tract transitional cell carcinoma is approximately 75%.[3]
- The major prognostic factor at the time of diagnosis of upper tract transitional cell cancer is the depth of infiltration into or through the uroepithelial wall.
- Most superficial tumors are likely to be well differentiated, while infiltrative tumors are likely to be poorly differentiated.ref name= NIH>Transitional cell cancer. National cancer institute. http://www.cancer.gov/types/kidney/hp/transitional-cell-treatment-pdq#section/_1</ref>
- They are curable in more than 90% of patients if they are superficial and confined to the renal pelvis or ureter.
- Patients with deeply invasive tumors that are still confined to the renal pelvis or ureter have a 10% to 15% likelihood of cure.
- Patients with tumors with penetration through the urothelial wall or with distant metastases usually cannot be cured with currently available forms of treatment.
- When involvement of the upper tract is diffuse (involving both the renal pelvis and ureter), the likelihood of subsequent development of bladder cancer increases to 75%.
- DNA ploidy has not added significant prognostic information beyond that provided by stage and grade.
References
- ↑ Bladder Cancer. Surveillance, Epidemiology, and End Results Program 2015.http://seer.cancer.gov/statfacts/html/urinb.html
- ↑ 2.0 2.1 2.2 2.3 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
- ↑ Munoz JJ, Ellison LM (2000). "Upper tract urothelial neoplasms: incidence and survival during the last 2 decades". J Urol. 164 (5): 1523–5. PMID 11025695.