Tezacaftor / ivacaftor
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sonya Gelfand
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Warning Title
See full prescribing information for complete Boxed Warning.
Condition Name: (Content)
|
Overview
Tezacaftor / ivacaftor is a Acetylcholine release inhibitor, Adrenergic receptor agonist that is FDA approved for the (type of indication of drug) of a list of indications, separated by commas.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include a list of adverse reactions, separated by commas..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Contraindications
CONTRAINDICATIONS
Warnings
|
Warning Title
See full prescribing information for complete Boxed Warning.
Condition Name: (Content)
|
Conidition 1
(Description)
Conidition 2
(Description)
Conidition 3
(Description)
Adverse Reactions
Clinical Trials Experience
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Condition 2
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Postmarketing Experience
(Description)
Drug Interactions
- Drug 1
- Drug 2
- Drug 3
- Drug 4
- Drug 5
Drug 1
(Description)
Drug 2
(Description)
Drug 3
(Description)
Drug 4
(Description)
Drug 5
(Description)
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
(Description)
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Tezacaftor / ivacaftor in women who are pregnant.
Labor and Delivery
(Description)
Nursing Mothers
(Description)g
Pediatric Use
(Description)
Geriatic Use
(Description)
Gender
(Description)
Race
(Description)
Renal Impairment
(Description)
Hepatic Impairment
(Description)
Females of Reproductive Potential and Males
(Description)
Immunocompromised Patients
(Description)
Others
(Description)
Administration and Monitoring
Administration
(Oral/Intravenous/etc)
Monitoring
- Confirm the presence of the F508delmutation on both al≤s the cystic fibrosis transmembrane conductance (CFTR) gene.
- Improvement in symptoms of cystic fibrosis is indicative of efficacy.
- ALT, AST, and bilirubin; baseline, every 3 months during the first year of treatment, and annually thereafter. More frequent monitoring may be warranted in patients with a history of transaminase elevations.
- Ophthalmological examinations; in pediatric patients at baseline and periodically during treatment.
IV Compatibility
There is limited information regarding the compatibility of Tezacaftor / ivacaftor and IV administrations.
Overdosage
Acute Overdose
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description)
Pharmacology
| |
Tezacaftor / ivacaftor
| |
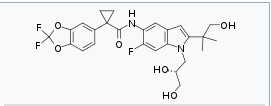
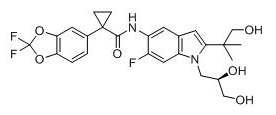
| Systematic (IUPAC) name | |
| 1-(2,2-Difluoro-1,3-benzodioxol-5-yl)-N-[1-[(2R)-2,3-dihydroxypropyl]-6-fluoro-2-(2-hydroxy-1,1-dimethylethyl)-1H-indol-5-yl]-cyclopropanecarboxamide | |
| Identifiers | |
| CAS number | |
| ATC code | ? |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
| |
Tezacaftor / ivacaftor
| |
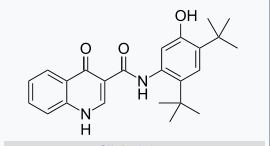
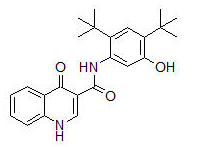
| Systematic (IUPAC) name | |
| N-(2,4-Di-tert-butyl-5-hydroxyphenyl)-4-oxo-1,4-dihydroquinoline-3-carboxamide | |
| Identifiers | |
| CAS number | |
| ATC code | R07 |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 392.490 g/mol |
| SMILES | & |
| Synonyms | VX-770 |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Protein binding | 99% |
| Metabolism | CYP3A |
| Half life | 12 hrs (single dose) |
| Excretion | 88% faeces |
| Therapeutic considerations | |
| Licence data |
, |
| Pregnancy cat. |
B(US) |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | By mouth |
Mechanism of Action
- Tezacaftor facilitates the cellular processing and trafficking of normal and select mutant forms of CFTR (including F508del-CFTR) to increase the amount of mature CFTR protein delivered to the cell surface. Ivacaftor is a CFTR potentiator that facilitates increased chloride transport by potentiating the channel-open probability (or gating) of the CFTR protein at the cell surface. For ivacaftor to function CFTR protein must be present at the cell surface. Ivacaftor can potentiate the CFTR protein delivered to the cell surface by tezacaftor, leading to a further enhancement of chloride transport than either agent alone. The combined effect of tezacaftor and ivacaftor is increased quantity and function of CFTR at the cell surface, resulting in increases in chloride transport.
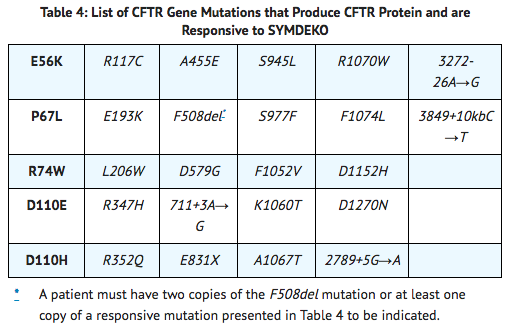
CFTR Chloride Transport Assay in Fisher Rat Thyroid (FRT) cells expressing mutant CFTR
- The chloride transport response of mutant CFTR protein to tezacaftor/ivacaftor was determined in Ussing chamber electrophysiology studies using a panel of FRT cell lines transfected with individual CFTR mutations. The FRT assay was conducted in ivacaftor-responsive mutations and F508del. Tezacaftor/ivacaftor increased chloride transport in FRT cells expressing CFTR mutations that result in CFTR protein being delivered to the cell surface.
- The minimum response threshold was designated as a net increase of at least 10% of untreated normal over baseline. The tezacaftor/ivacaftor incubation resulted in either similar or increased chloride transport compared to ivacaftor alone. In vitro data may not accurately predict added clinical benefit of SYMDEKO (tezacaftor/ivacaftor combination) over KALYDECO (ivacaftor) alone for individual mutations. In addition, the magnitude of the net change over baseline in CFTR-mediated chloride transport is not correlated with the magnitude of clinical response for individual mutations.

- Table 4 lists responsive CFTR mutations based on (1) a clinical FEV1 response and/or (2) in vitro data in FRT cells, indicating that tezacaftor/ivacaftor increases chloride transport to at least 10% of untreated normal over baseline. CFTR gene mutations that are not responsive to ivacaftor alone are not expected to respond to SYMDEKO except for F508del homozygotes.
Structure
- Tezacaftor:
- Ivacaftor:
Pharmacodynamics
Effects on Sweat Chloride
- In Trial 1 (patients homozygous for the F508del mutation), the treatment difference between SYMDEKO and placebo in mean absolute change from baseline in sweat chloride through Week 24 was -10.1 mmol/L (95% CI: -11.4, -8.8).
- In Trial 2 (patients heterozygous for the F508del mutation and a second mutation predicted to be responsive to tezacaftor/ivacaftor), the treatment difference in mean absolute change from baseline in sweat chloride through Week 8 was -9.5 mmol/L (95% CI: -11.7, -7.3) between SYMDEKO and placebo, and -4.5 mmol/L (95% CI: -6.7, -2.3) between ivacaftor and placebo.
Cardiac Electrophysiology
- At a dose 3 times the maximum approved recommended dose, tezacaftor does not prolong the QT interval to any clinically relevant extent.
- In a separate study of ivacaftor evaluating doses up to 3 times the maximum approved recommended dose, ivacaftor does not prolong the QT interval to any clinically relevant extent.
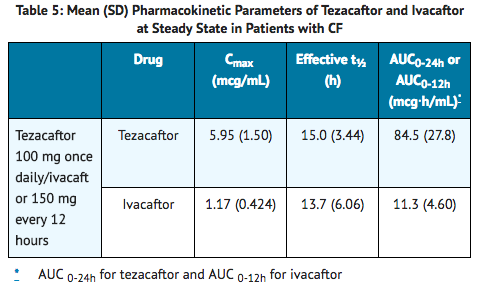
Pharmacokinetics
- The pharmacokinetics of tezacaftor and ivacaftor are similar between healthy adult volunteers and patients with CF. Following once-daily dosing of tezacaftor and twice-daily dosing of ivacaftor in patients with CF, plasma concentrations of tezacaftor and ivacaftor reach steady-state within 8 days and within 3 to 5 days, respectively, after starting treatment. At steady-state, the accumulation ratio is approximately 1.5 for tezacaftor and 2.2 for ivacaftor. Exposures of tezacaftor (administered alone or in combination with ivacaftor) increase in an approximately dose-proportional manner with increasing doses from 10 mg to 300 mg once daily.
- Key pharmacokinetic parameters for tezacaftor and ivacaftor at steady state are shown in Table 5.
Absorption
- After a single dose in healthy subjects in the fed state, tezacaftor was absorbed with a median (range) time to maximum concentration (tmax) of approximately 4.0 hours (2 to 6 hours). The median (range) tmax of ivacaftor was approximately 6.0 hours (3 to 10 hours) in the fed state.
- When a single dose of tezacaftor/ivacaftor was administered with fat-containing foods, tezacaftor exposure was similar and ivacaftor exposure was approximately 3 times higher than when taken in a fasting state.
Distribution
- Tezacaftor is approximately 99% bound to plasma proteins, primarily to albumin. Ivacaftor is approximately 99% bound to plasma proteins, primarily to alpha 1-acid glycoprotein and albumin. After oral administration of tezacaftor 100 mg once daily/ivacaftor 150 mg every 12 hours in patients with CF in the fed state, the mean (±SD) for apparent volume of distribution of tezacaftor and ivacaftor was 271 (157) L and 206 (82.9) L, respectively. Neither tezacaftor nor ivacaftor partition preferentially into human red blood cells.
Elimination
- After oral administration of tezacaftor 100 mg once daily/ivacaftor 150 mg every 12 hours in patients with CF in the fed state, the mean (±SD) for apparent clearance values of tezacaftor and ivacaftor were 1.31 (0.41) and 15.7 (6.38) L/h, respectively. After steady-state dosing of tezacaftor in combination with ivacaftor in CF patients, the effective half-lives of tezacaftor and ivacaftor were approximately 15.0 (3.44) and 13.7 (6.06) hours, respectively.
Metabolism
- Tezacaftor is metabolized extensively in humans. In vitro data suggested that tezacaftor is metabolized mainly by CYP3A4 and CYP3A5. Following oral administration of a single dose of 100 mg 14C-tezacaftor to healthy male subjects, M1, M2, and M5 were the 3 major circulating metabolites of tezacaftor in humans. M1 has the similar potency to that of tezacaftor and is considered pharmacologically active. M2 is much less pharmacologically active than tezacaftor or M1, and M5 is not considered pharmacologically active. Another minor circulating metabolite, M3, is formed by direct glucuronidation of tezacaftor.
- Ivacaftor is also metabolized extensively in humans. In vitro and in vivo data indicate that ivacaftor is metabolized primarily by CYP3A4 and CYP3A5. M1 and M6 are the two major metabolites of ivacaftor in humans. M1 has approximately one-sixth the potency of ivacaftor and is considered pharmacologically active. M6 is not considered pharmacologically active.
Excretion
- Following oral administration of 14C-tezacaftor, the majority of the dose (72%) was excreted in the feces (unchanged or as the M2 metabolite) and about 14% was recovered in urine (mostly as M2 metabolite), resulting in a mean overall recovery of 86% up to 21 days after the dose. Less than 1% of the administrated dose was excreted in urine as unchanged tezacaftor, showing that renal excretion is not the major pathway of tezacaftor elimination in humans.
- Following oral administration of ivacaftor alone, the majority of ivacaftor (87.8%) is eliminated in the feces after metabolic conversion. There was minimal elimination of ivacaftor and its metabolites in urine (only 6.6% of total radioactivity was recovered in the urine), and there was negligible urinary excretion of ivacaftor as unchanged drug.
Specific Populations
Pediatric patients 12 to less than 18 years of age
- The following conclusions about exposures between adults and the pediatric population are based on population PK analyses:
- Following oral administration of SYMDEKO tablets, tezacaftor 100 mg once daily / ivacaftor 150 mg every 12 hours, the mean (±SD) AUCss was 97.3 (35.7) mcg∙h/mL and 11.4 (5.46) mcg∙h/mL, respectively for tezacaftor and ivacaftor, similar to the mean AUCss in adult patients administered SYMDEKO tablets, tezacaftor 100 mg once daily/ivacaftor 150 mg every 12 hours.
Patients with Hepatic Impairment
- Following multiple doses of tezacaftor and ivacaftor for 10 days, subjects with moderately impaired hepatic function (Child-Pugh Class B, score 7 to 9) had an approximately 36% increase in AUC and a 10% increase in Cmax for tezacaftor, and a 1.5-fold increase in ivacaftor AUC compared with healthy subjects matched for demographics. In a separate study, subjects with moderately impaired hepatic function (Child-Pugh Class B, score 7-9) had similar ivacaftor Cmax, but an approximately 2.0-fold increase in ivacaftor AUC0-∞ compared with healthy subjects matched for demographics.
- Pharmacokinetic studies have not been conducted in patients with mild (Child-Pugh Class A, score 5 to 6) or severe hepatic impairment (Child-Pugh Class C, score 10 to 15) receiving SYMDEKO. The magnitude of increase in exposure in patients with severe hepatic impairment is unknown, but is expected to be higher than that observed in patients with moderate hepatic impairment.
Patients with Renal Impairment
- SYMDEKO has not been studied in patients with moderate or severe renal impairment (creatinine clearance ≤30 mL/min) or in patients with end-stage renal disease. In a human pharmacokinetic study with tezacaftor alone, there was minimal elimination of tezacaftor and its metabolites in urine (only 13.7% of total radioactivity was recovered in the urine with 0.79% as unchanged drug).
- In a human pharmacokinetic study with ivacaftor alone, there was minimal elimination of ivacaftor and its metabolites in urine (only 6.6% of total radioactivity was recovered in the urine).
- In population pharmacokinetic analysis, data from 665 patients on tezacaftor or tezacaftor in combination with ivacaftor in Phase 2/3 clinical trials indicated that mild renal impairment (N=147; eGFR 60 to less than 90 mL/min/1.73 m2) and moderate renal impairment (N=7; eGFR 30 to less than 60 mL/min/1.73 m2) did not affect the clearance of tezacaftor significantly.
Male and Female Patients
- The pharmacokinetic parameters of tezacaftor and ivacaftor are similar in males and females.
Drug Interactions Studies
- Drug interaction studies were performed with SYMDEKO and other drugs likely to be co-administered or drugs commonly used as probes for pharmacokinetic interaction studies.
Potential for Tezacaftor/Ivacaftor to Affect Other Drugs
- Clinical studies (with rosiglitazone and desipramine – see TABLE 6) showed that ivacaftor is not an inhibitor of CYP2C8 or CYP2D6. Based on in vitro results, ivacaftor has the potential to inhibit CYP3A and P-gp, and may also inhibit CYP2C9. In vitro, ivacaftor was not an inducer of CYP isozymes. Ivacaftor is not an inhibitor of transporters OATP1B1, OATP1B3, OCT1, OCT2, OAT1, or OAT3.
- Based on in vitro results, tezacaftor has a low potential to inhibit CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP3A4. Tezacaftor has a low potential to induce CYP3A, but it is not an inducer of CYP1A2 and CYP2B6. Tezacaftor has a low potential to inhibit transporters P-gp, BCRP, OATP1B1, OATP1B3, OCT2, OAT1, or OAT3.
- Clinical studies with midazolam showed that SYMDEKO is not an inhibitor of CYP3A. Co-administration of SYMDEKO with digoxin, a sensitive P-gp substrate, increased digoxin exposure by 1.3-fold. Co administration of SYMDEKO with an ethinyl estradiol/ norethindrone oral contraceptive had no significant effect on the exposures of the hormonal contraceptives.
- The effects of tezacaftor and ivacaftor (or ivacaftor alone) on the exposure of co-administered drugs are shown in Table 6.
Potential for Other Drugs to Affect Tezacaftor/Ivacaftor
- In vitro studies showed that ivacaftor and tezacaftor were substrates of CYP3A enzymes (i.e., CYP3A4 and CYP3A5). Exposure to ivacaftor and tezacaftor will be reduced by concomitant CYP3A inducers and increased by concomitant CYP3A inhibitors.
- In vitro studies showed that tezacaftor is a substrate for the uptake transporter OATP1B1, and efflux transporters P-gp and BCRP. Tezacaftor is not a substrate for OATP1B3. In vitro studies showed that ivacaftor is not a substrate for OATP1B1, OATP1B3, or P-gp.
- The effects of co-administered drugs on the exposure of tezacaftor and ivacaftor (or ivacaftor alone) are shown in Table 7.


Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- No studies of carcinogenicity, mutagenicity, or impairment of fertility were conducted with the combination of tezacaftor and ivacaftor, however, separate studies of tezacaftor and ivacaftor are described below.
Tezacaftor
- A 2-year study in Sprague-Dawley rats and a 6-month study in Tg.rasH2 transgenic mice were conducted to assess the carcinogenic potential of tezacaftor. No evidence of tumorigenicity from tezacaftor was observed in male and female rats at oral doses up to 50 and 75 mg/kg/day (approximately 2 and 3 times the MRHD based on summed AUCs of tezacaftor and its metabolites in males and females, respectively). No evidence of tumorigenicity was observed in male and female Tg.rasH2 transgenic mice at tezacaftor doses up to 500 mg/kg/day.
- Tezacaftor was negative for genotoxicity in the following assays: Ames test for bacterial gene mutation, in vitro chromosomal aberration assay in Chinese hamster ovary cells, and in vivo mouse micronucleus test.
- There were no effects on male or female fertility and early embryonic development in rats at oral tezacaftor doses up to 100 mg/kg/day (approximately 3 times the MRHD based on summed AUC of tezacaftor and M1 metabolite).
Ivacaftor
- Two-year studies were conducted in CD-1 mice and Sprague-Dawley rats to assess the carcinogenic potential of ivacaftor. No evidence of tumorigenicity from ivacaftor was observed in mice or rats at oral doses up to 200 mg/kg/day and 50 mg/kg/day, respectively (approximately equivalent to 2 and 9 times the MRHD, respectively, based on summed AUCs of ivacaftor and its metabolites).
- Ivacaftor was negative for genotoxicity in the following assays: Ames test for bacterial gene mutation, in vitro chromosomal aberration assay in Chinese hamster ovary cells, and in vivo mouse micronucleus test.
- Ivacaftor impaired fertility and reproductive performance indices in male and female rats at 200 mg/kg/day (approximately 9 and 6 times, respectively, the MRHD based on summed AUCs of ivacaftor and its metabolites). Increases in prolonged diestrus were observed in females at 200 mg/kg/day. Ivacaftor also increased the number of females with all nonviable embryos and decreased corpora lutea, implantations, and viable embryos in rats at 200 mg/kg/day (approximately 6 times the MRHD based on summed AUCs of ivacaftor and its metabolites) when dams were dosed prior to and during early pregnancy. These impairments of fertility and reproductive performance in male and female rats at 200 mg/kg/day were attributed to severe toxicity. No effects on male or female fertility and reproductive performance indices were observed at ≤100 mg/kg/day (approximately 6 and 4 times, respectively, the MRHD based on summed AUCs of ivacaftor and its metabolites).
Clinical Studies
Dose Ranging:
- Dose selection for the clinical program primarily consisted of one double-blind, placebo-controlled, multiple-cohort trial which included 176 patients with CF (homozygous for the F508del mutation) 18 years of age and older with a screening ppFEV1≥40. In the study, 34 and 106 patients, respectively, received tezacaftor at once-daily doses of 10 mg, 30 mg, 100 mg, or 150 mg alone or in combination with ivacaftor 150 mg q12h, and 33 patients received placebo. During the 28-day treatment period, dose-dependent increases in mean ppFEV1 change from baseline were observed with tezacaftor in combination with ivacaftor. Tezacaftor/ivacaftor in general had a greater mean treatment effect than tezacaftor alone. No additional benefit was observed at tezacaftor doses greater than 100 mg daily.
Efficacy:
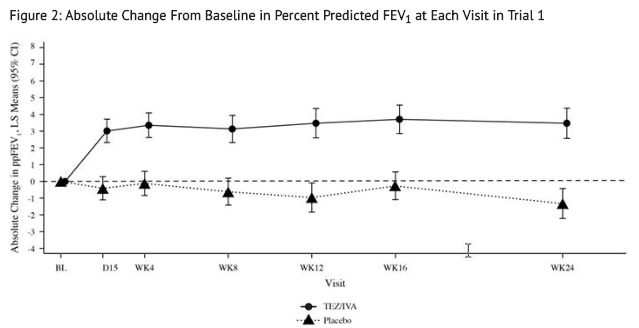
- The efficacy of SYMDEKO in patients with CF aged 12 years and older was evaluated in three Phase 3, double-blind, placebo-controlled trials (Trials1, 2, and 3).
- Trial 1 was a 24-week randomized, double-blind, placebo-controlled, two-arm study in CF patients who were homozygous for the F508del mutation in the CFTR gene.
- Trial 2 was a randomized, double-blind, placebo-controlled, 2-period, 3-treatment, 8-week crossover study in CF patients who were heterozygous for the F508del mutation and a second mutation predicted to be responsive to tezacaftor/ivacaftor. Mutations predicted to be responsive were selected for the study based on the clinical phenotype (pancreatic sufficiency), biomarker data (sweat chloride), and in vitro responsiveness to tezacaftor/ivacaftor. Patients were randomized to and received sequences of treatment that included SYMDEKO, ivacaftor, and placebo.
- Trial 3 was a 12-week randomized, double-blind, placebo-controlled, two-arm study in CF patients who were heterozygous for the F508del mutation and a second CFTR mutation predicted to be unresponsive to tezacaftor/ivacaftor. Mutations predicted to be non-responsive were selected for the study based on biologic plausibility (mutation class), clinical phenotype (pancreatic insufficiency), biomarker data (sweat chloride), and in vitro testing to tezacaftor and/or ivacaftor.
- Patients in all trials continued on their standard-of-care CF therapies (e.g., bronchodilators, inhaled antibiotics, dornase alfa, and hypertonic saline) and were eligible to roll over into a 96-week open-label extension. Patients had a ppFEV1 at screening between 40-90%. Patients with a history of colonization with organisms associated with a more rapid decline in pulmonary status such as Burkholderia cenocepacia, Burkholderia dolosa, or Mycobacterium abscessus, or who had 2 or more abnormal liver function tests at screening (ALT, AST, AP, GGT ≥3 × ULN or total bilirubin ≥2 × ULN) or AST or ALT ≥5 × ULN, were excluded from the trials.
Trial in Patients with CF Who Were Homozygous for the F508del Mutation in the CFTR Gene (Trial 1)
- Trial 1 evaluated 504 patients (248 SYMDEKO, 256 placebo) with CF aged 12 years and older (mean age 26.3 years). The mean ppFEV1 at baseline was 60.0% [range: 27.8% to 96.2%]. The primary efficacy endpoint was change in lung function as determined by absolute change from baseline in ppFEV1 through Week 24. Treatment with SYMDEKO resulted in a statistically significant improvement in ppFEV1. The treatment difference between SYMDEKO and placebo for the mean absolute change in ppFEV1 from baseline through Week 24 was 4.0 percentage points (95% CI: 3.1, 4.8; P<0.0001). These changes persisted throughout the 24-week treatment period (Figure 2). Improvements in ppFEV1 were observed regardless of age, sex, baseline ppFEV1, colonization with Pseudomonas, concomitant use of standard-of-care medications for CF, and geographic region.
- Key secondary efficacy variables included relative change from baseline in ppFEV1 through Week 24; number of pulmonary exacerbations from baseline through Week 24; absolute change in BMI from baseline at Week 24, and absolute change in CFQ-R Respiratory Domain Score (a measure of respiratory symptoms relevant to patients with CF, such as cough, sputum production, and difficulty breathing) from baseline through Week 24. For the purposes of this trial, a pulmonary exacerbation was defined as a change in antibiotic therapy (IV, inhaled, or oral) as a result of 4 or more of 12 pre-specified sino-pulmonary signs/symptoms. See TABLE 8 for a summary of key secondary outcomes in Trial 1.

Trial in Patients with CF Who Were Heterozygous for the F508del Mutation and a Second Mutation Predicted to be Responsive to Tezacaftor/Ivacaftor (Trial 2)
- Trial 2 evaluated 244 patients with CF aged 12 years and older (mean age 34.8 years). The mean ppFEV1 at baseline was 62.3% [range: 34.6 to 93.5]. Of the 244 patients included in the efficacy analysis, 146 patients had a splice mutation and 98 patients had a missense mutation as the second allele. 161 patients received SYMDEKO, 156 patients received ivacaftor, and 161 patients received placebo. The primary efficacy endpoint was the mean absolute change from study baseline in percent predicted FEV1 averaged at Weeks 4 and 8 of treatment. The key secondary efficacy endpoint was absolute change in CFQ-R Respiratory Domain Score from study baseline averaged at Weeks 4 and 8 of treatment. For the overall population, treatment with SYMDEKO compared to placebo resulted in significant improvement in ppFEV1 [6.8 percentage points (95% CI: 5.7, 7.8); P<0.0001] and CFQ-R Respiratory Domain Score [11.1 points (95% CI 8.7, 13.6); P<0.0001]. Treatment difference for ppFEV1 between ivacaftor- and placebo-treated patients was 4.7 percentage points (95% CI: 3.7, 5.8; P<0.0001) and 2.1 percentage points (95% CI: 1.2, 2.9; P<0.0001) between SYMDEKO- and ivacaftor-treated patients, which were statistically significant. Improvements in ppFEV11 were observed regardless of age, baseline ppFEV1, sex, mutation class, colonization with Pseudomonas, concomitant use of standard-of-care medications for CF, and geographic region. Statistically significant improvements compared to placebo were also observed in the subgroup of patients with splice mutations and missense mutations (Table 9).

- In an analysis of BMI at Week 8, an exploratory endpoint, patients treated with SYMDEKO had a mean improvement of 0.2 kg/m2 [95% CI (0.0, 0.3)], 0.1 kg/m2 [95% CI (-0.1, 0.3)], and 0.3 kg/m2 [95% CI (0.1, 0.5)] versus placebo for the overall, splice, and missense mutation populations of patients, respectively.
Trial in Patients with CF Who Were Heterozygous for the F508del Mutation and a Second Mutation Not Predicted to be Responsive to Tezacaftor/Ivacaftor (Trial 3)
- Trial 3 evaluated 168 patients with CF (83 SYMDEKO and 85 placebo) aged 12 years and older (mean age 26.1 years) who were heterozygous for the F508del mutation and had a second CFTR mutation predicted to be unresponsive to tezacaftor/ivacaftor. CF patients with the F508del mutation and one of the following mutations in the CFTR gene were enrolled in the study (listed in decreasing frequency): W1282X, G542X, N1303K, 621+1G>T, 1717-1G>A, 1898+1G>A, CFTRdele2,3, 2183delAA>G, 2184insA, R1162X, R553X, 3659delC, 3905insT, G970R, I507del, R1066C, R347P, 1154insTC, 1811+1.6kbA>G, 2184delA, 405+1G>A, E60X, G85E, L1077P, Q39X, S466X, Y1092X, 1078delT, 1248+1G>A, 1677delTA, 1812-1G>A, 2869INSG, 3120+1G>A, 394delTT, 457TAT>G, 711+1G>T, 711+5G>A, 712-1G>T, G673x, L1065P, Q220X, Q493X, R709X, V520F. The mean ppFEV1 at baseline was 57.5% [range: 31.0 to 96.7]. The primary efficacy endpoint was change from baseline in absolute ppFEV1 through Week 12. The overall treatment difference between SYMDEKO and placebo for the mean absolute change in ppFEV1 from baseline through Week 12 was 1.2 percentage points (95% CI: -0.3, 2.6). This study was terminated following the planned interim analysis because the pre-specified futility criteria were met.
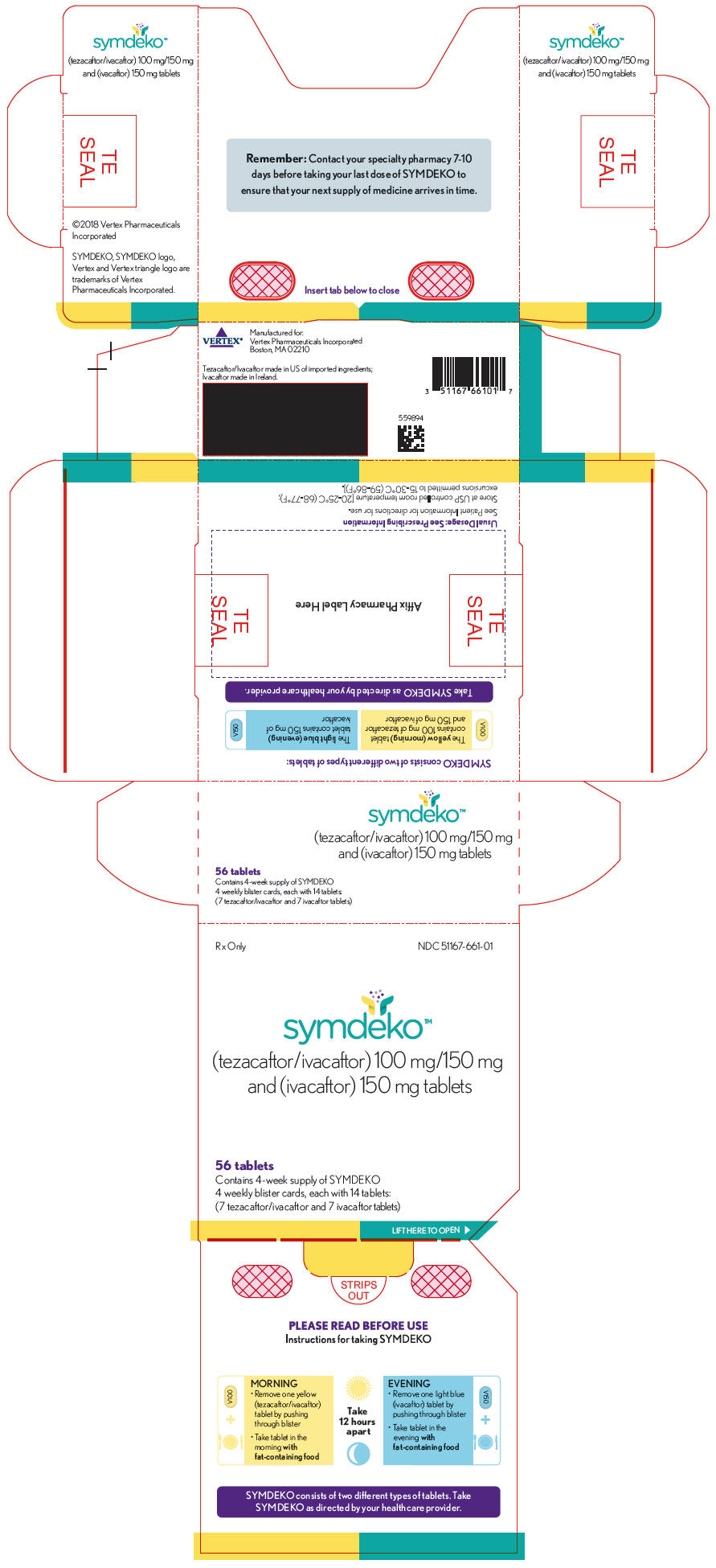
How Supplied
- SYMDEKO is co-packaged as a tezacaftor/ivacaftor fixed-dose combination tablet and an ivacaftor tablet. The tezacaftor/ivacaftor fixed dose combination tablets are supplied as yellow, capsule-shaped tablets containing 100 mg of tezacaftor and 150 mg of ivacaftor. Each tablet is debossed with "V100" on one side and plain on the other. Ivacaftor tablets are supplied as light blue, film-coated, capsule-shaped tablets containing 150 mg of ivacaftor. Each tablet is printed with the characters "V150" on one side and plain on the other. SYMDEKO is supplied as:
- 56-count tablet carton containing a 4-week supply (4 weekly wallets, each with 14 tablets)
- NDC 51167-661-01
Storage
- Store at 20-25ºC (68-77ºF); excursions permitted to 15-30ºC (59-86ºF).
Images
Drug Images
{{#ask: Page Name::Tezacaftor / ivacaftor |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Tezacaftor / ivacaftor |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling.
Transaminase (ALT or AST) Elevations and Monitoring
- Inform patients that elevation in liver tests has occurred in patients treated with SYMDEKO or with ivacaftor alone. Transaminases (ALT and AST) should be assessed prior to initiating SYMDEKO, every 3 months during the first year of treatment, and annually thereafter. More frequent monitoring should be considered in patients with a history of transaminase elevations.
Drug Interactions with CYP3A Inducers and Inhibitors
- Ask patients to tell you all the medications they are taking including any herbal supplements or vitamins. Co-administration of SYMDEKO with strong CYP3A inducers (e.g., rifampin, St. John's wort) is not recommended, as they may reduce the therapeutic effectiveness of SYMDEKO. Adjustment of the dose to one tablet of tezacaftor 100 mg/ivacaftor 150 mg twice a week, taken approximately 3 to 4 days apart is recommended when co-administered with strong CYP3A inhibitors, such as ketoconazole. Advise the patient not to take the evening dose of ivacaftor 150 mg. Dose reduction to one tablet of tezacaftor 100 mg/ivacaftor 150 mg or ivacaftor 150 mg, taken on alternate days in the morning is recommended when co-administered with moderate CYP3A inhibitors, such as fluconazole. Advise the patient not to take the evening dose of ivacaftor 150 mg. Food or drink containing grapefruit or Seville oranges should be avoided.
Cataracts
- Inform patients that abnormality of the eye lens (cataract) has been noted in some children and adolescents receiving SYMDEKO or with ivacaftor alone. Baseline and follow-up ophthalmological examinations should be performed in pediatric patients initiating treatment with SYMDEKO.
Use in Patients with Hepatic Impairment
- Inquire and/or assess whether patients have liver impairment. Adjust the dose in patients with moderately impaired hepatic function (Child-Pugh Class B, score 7-9) to one tablet of tezacaftor 100 mg/ivacaftor 150 mg once daily in the morning and advise the patient not to take the evening dose of ivacaftor 150 mg. SYMDEKO has not been studied in patients with severe hepatic impairment (Child-Pugh Class C, score 10-15); however, exposure is expected to be substantially higher than that observed in patients with moderate hepatic impairment. When benefits are expected to outweigh the risks, SYMDEKO should be used with caution in patients with severe hepatic impairment at a dose of one tablet of tezacaftor 100 mg/ivacaftor 150 mg once daily in the morning or less frequently. Advise the patient not to take the evening dose of ivacaftor 150 mg. No dose adjustment is recommended for patients with mild hepatic impairment (Child-Pugh Class A, score 5-6).
Administration
- Inform patients that SYMDEKO is best absorbed by the body when taken with food that contains fat. A typical CF diet will satisfy this requirement. Examples include eggs, butter, peanut butter, cheese pizza, whole-milk dairy products (such as whole milk, cheese, and yogurt), etc..
- Patients should be informed about what to do in the event they miss a dose of SYMDEKO or ivacaftor:
- If 6 hours or less have passed since the time SYMDEKO is usually taken, patients should be instructed to take the prescribed dose of SYMDEKO with fat-containing food as soon as possible.
- If more than 6 hours have passed since the time SYMDEKO is usually taken, the missed dose should NOT be taken and the patient should resume the usual dosing schedule.
- Patients should be advised to contact their health care provider if they have questions.

Precautions with Alcohol
Alcohol-Tezacaftor / ivacaftor interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Symdeko
Look-Alike Drug Names
There is limited information regarding Tezacaftor / ivacaftor Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.