Tetanus
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Assistant Editor(s)-in-Chief: Michael Maddaleni, B.S.{{#meta: itemprop="medicalWebPageAudiences" content="patient"}}{{#meta: itemprop="medicalWebPageSpecialities" content="cardiology"}}{{#meta: itemprop="medicalWebPageInfoTypes" content="symptoms,diagnosis,treatment,causes,prognosis,complications"}} Classification Classic::Classification Atypical::
Overview
|
Tetanus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tetanus On the Web |
|
American Roentgen Ray Society Images of Tetanus |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2];Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [3]
Overview
Tetanus is a medical condition that is characterized by a prolonged contraction of skeletal muscle fibers. The primary symptoms are caused by tetanospasmin, a neurotoxin produced by the Gram-positive, obligate anaerobic bacterium Clostridium tetani. Infection generally occurs through wound contamination, and often involves a cut or deep puncture wound. As the infection progresses, muscle spasms in the jaw develop hence the common name, lockjaw. This is followed by difficulty swallowing and general muscle stiffness and spasms in other parts of the body.[1] Infection can be prevented by proper immunization and by post-exposure prophylaxis.[2]
Tetanus affects skeletal muscle, a type of striated muscle. The other type of striated muscle, cardiac or heart muscle cannot be tetanized because of their intrinsic electrical properties. In recent years, approximately 11% of reported tetanus cases have been fatal. The highest mortality rates are in unvaccinated persons and persons over 60 years of age. C. tetani, the bacteria that causes tetanus, is recovered from the initial wound in only about 30% of cases, and can be found in patients who do not have tetanus.
The clinical manifestations of tetanus are caused when tetanus toxin blocks inhibitory nerve impulses, by interfering with the release of neurotransmitters. This leads to unopposed muscle contraction and spasm. Seizures may occur, and the autonomic nervous system may also be affected. The term tetany refers to sustained muscle contraction that is not caused by tetanus.
Historical Perspective
In 1884 Carle and Rattone discovered tetanus by injecting animals with pus from a patient who had died of tetanus. In 1924 Descombey developed the tetanus toxoid, which was extensively utilized in the second World War.
Classification
Tetanus can be classified with respect to its patterns of presentation into neonatal, cephalic, generalized or local.[3]
Pathophysiology
The bacteria that causes tetanus, Clostridium tetani is introduced into the human body usually by a wound. The toxins produced by the bacterium, utilize the blood and/or lymphatics to gain access to target tissues. The toxins can act at various places in the central nervous system, including the spinal cord, peripheral motor end plates, and the brain. They can also act on the sympathetic nervous system.[4][5]
Causes
Clostridium tetani is a rod-shaped, anaerobic bacterium of the genus Clostridium. Like other Clostridium species, it is Gram-positive, and its appearance on a gram stain resembles tennis rackets or drumsticks.[6] C. tetani is found as spores in soil or as parasites in the gastrointestinal tract of animals. C. tetani produces a potent biological toxin, tetanospasmin, and is the causative agent of tetanus.
Differentiating Tetanus from other Diseases
Tetanus must be differentiated from strychnine poisoning, dental infections, drug reactions, hypocalcemia, meningitis, stroke and stiff man syndrome.[7]
Epidemiology and Demographics
Tetanus is an infectious disease which is not know to be contagious and can be prevented with a vaccine. There are less than 100 cases of tetanus in the US and around five deaths can be attributed to tetanus every year. There are about one million cases of tetanus reported worldwide. These according to an estimate lead to 300,000 to 500,000 deaths every year. The incidence of tetanus in the United States is 0.01 cases per 100,000 individuals. Tetanus is more commonly seen in Hispanics. Individuals greater than age 65 have a higher incidence of tetanus. Tetanus has a case fatality rate of 13.2%.[8][9][10]
Risk Factors
Clostridium tetani spores can be found in various locations including manure, soil and dust. Inhabitants of developing countries are at a higher risk of acquiring tetanus because of lack of tetanus vaccination and less focus on general hygiene. Various risk factors for tetanus include contaminated wounds, punctured wounds, crushing, burns and working in unhygienic environment.[11][12]
Screening
The United States Preventive Services Task Force (USPSTF) has not recommended any guidelines for the screening of tetanus.
Natural History, Complications and Prognosis
Tetanus can have an incubation period of 2 to 38 days with the man being 7 to days post exposure. The presentation and progression may vary depending on the type of tetanus. Generalized tetanus can involve the respiratory muscles making it difficult to breathe. The complications of tetanus include fractures, laryngospasm, aspiration pneumonia and pulmonary embolism. Tetanus has a fatality rate of almost 11%. The fatality rate of tetanus might be associated with prolonged convulsions and contractions. Tetanus without spasms has an excellent prognosis. Early diagnosis is also associated with a good prognosis.[13][14]
Diagnosis
History and Symptoms
The history of a patient presenting with tetanus typically reveals soil, rust containing metal or manure related contamination of an injury or a wound. Punctured wounds, burns, scratches by animals, fractures, otitis media and surgical wounds that are contaminated, these can be related to surgeries on the gastrointestinal tract or abortions. History of recent accident or an injury leading to break in the continuity of the skin in the a contaminated environment is helpful in making a diagnosis. Trismus, or lockjaw, spasms of the facial muscles (risus sardonicus), neck stiffness and swallowing difficulty are some important symptoms of tetanus.[15][16]
Physical Examination
Tetanus may initially present with muscle stiffness. The distribution may vary with the type of tetanus. Maseters are commonly involved initially with an accompanying headache. Neck stiffness, difficulty swallowing, spasms involving various muscles groups including the abdominal muscles and sweating may be seen later in the disease.
Laboratory Findings
Tetanus is a clinical diagnosis and there are no laboratory findings characteristic of tetanus. The diagnosis is based on the a detailed history and a thorough physical exam. Bacteriologic confirmation is not required. C. tetani can be found in individuals without tetanus and only 30% of tetanic wounds may yield the pathogen.[17]
Xray
Tetanus is clinical diagnosis and there are no x ray findings associated with tetanus.
CT scan
Tetanus is clinical diagnosis and there are no CT scan findings associated with tetanus.
MRI
Tetanus is clinical diagnosis and there are no MRI findings associated with tetanus.
Ultrasound
Tetanus is clinical diagnosis and there are no ultrasound findings associated with tetanus.
Other Imaging Studies
Tetanus is clinical diagnosis and there are no other imaging studies done for tetanus.
Other Diagnostic Studies
Tetanus is clinical diagnosis and other diagnostic studies are not done for tetanus.
Treatment
Medical Therapy
Tetanus is a medical emergency. Medical therapy includes hospitalization, immediate treatment with human tetanus immune globulin (TIG) (or equine antitoxin if human immune globulin is not available), a tetanus toxoid booster, agents to control muscle spasm, aggressive wound care, and antimicrobial therapy. Mechanical ventilation and agents to control autonomic nervous system instability may be required among patients with severe disease.
Surgery
The only surgical intervention required for the management of tetanus is wound debridement. The contaminated wound must always be cleaned.
Primary Prevention
A very common primary prevention method for tetanus is vaccinating against the bacteria which causes tetanus, Clostridium tetani. Other methods of primary prevention include proper wound care, avoiding injuries, wearing protective equipment when playing, keeping surroundings clean, controlling diabetes, ensuring aseptic gynecological procedures, aggressively managing burn and compound fracture injuries and avoiding IV drug abuse
Secondary Prevention
Tetanus vaccine can prevent Tetanus for approximately 10 years. Post-exposure care is indicated in people who do not know exactly when their last Tetanus booster was and who did not complete their primary prevention set of vaccinations. These patients will typically receive passive immunity with tetanus immune globulin (TIG).
Cost-Effectiveness of Therapy
The major cost encountered with tetanus is in the form of the vaccine. There are many different trade names associated with the tetanus vaccine that come with slightly different costs. The prices of the vaccines are all listed in the following tables. The tables are separated based upon pediatric doses versus adult doses. The DTaP vaccine that is mentioned in the passage stands for Diptheria, Tetanus, and Pertussis.
References
- ↑ Wells CL, Wilkins TD (1996). Clostridia: Sporeforming Anaerobic Bacilli. In: Baron's Medical Microbiology (Baron S et al, eds.) (4th ed. ed.). Univ of Texas Medical Branch. (via NCBI Bookshelf) ISBN 0-9631172-1-1.
- ↑ "Tetanus" (PDF). CDC Pink Book. Retrieved 2007-01-26.
- ↑ Angurana SK, Jayashree M, Bansal A, Singhi S, Nallasamy K (2017). "Post-neonatal Tetanus in a PICU of a Developing Economy: Intensive Care Needs, Outcome and Predictors of Mortality". J Trop Pediatr. doi:10.1093/tropej/fmx020. PMID 28460120.
- ↑ Farrar JJ, Yen LM, Cook T, Fairweather N, Binh N, Parry J; et al. (2000). "Tetanus". J Neurol Neurosurg Psychiatry. 69 (3): 292–301. PMC 1737078. PMID 10945801.
- ↑ Lalli G, Gschmeissner S, Schiavo G (2003). "Myosin Va and microtubule-based motors are required for fast axonal retrograde transport of tetanus toxin in motor neurons". J Cell Sci. 116 (Pt 22): 4639–50. doi:10.1242/jcs.00727. PMID 14576357.
- ↑ Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. ISBN 0838585299.
- ↑ Anisha Doshi, Clare Warrell, Dima Dahdaleh & Dimitri Kullmann (2014). "Just a graze? Cephalic tetanus presenting as a stroke mimic". Practical neurology. 14 (1): 39–41. doi:10.1136/practneurol-2013-000541. PMID 24052566. Unknown parameter
|month=ignored (help) - ↑ Centers for Disease Control and Prevention (CDC) (2011). "Tetanus surveillance --- United States, 2001-2008". MMWR Morb Mortal Wkly Rep. 60 (12): 365–9. PMID 21451446.
- ↑ "Pinkbook | Tetanus | Epidemiology of Vaccine Preventable Diseases | CDC".
- ↑ Rushdy AA, White JM, Ramsay ME, Crowcroft NS (2003). "Tetanus in England and Wales, 1984-2000". Epidemiol Infect. 130 (1): 71–7. PMC 2869940. PMID 12613747.
- ↑ "Tetanus | About Tetanus Disease | Lockjaw | CDC".
- ↑ Del Pilar Morales E, Bertrán Pasarell J, Cardona Rodriguez Z, Almodovar Mercado JC, Figueroa Navarro A (2014). "Cephalic tetanus following penetrating eye trauma: a case report". Bol Asoc Med P R. 106 (2): 25–9. PMID 25065047.
- ↑ Thwaites CL, Beeching NJ, Newton CR (2015). "Maternal and neonatal tetanus". Lancet. 385 (9965): 362–70. doi:10.1016/S0140-6736(14)60236-1. PMID 25149223.
- ↑ J. C. Patel & B. C. Mehta (1999). "Tetanus: study of 8,697 cases". Indian journal of medical sciences. 53 (9): 393–401. PMID 10710833. Unknown parameter
|month=ignored (help) - ↑ "Tetanus | Symptoms and Complications | Lockjaw | CDC".
- ↑ Anisha Doshi, Clare Warrell, Dima Dahdaleh & Dimitri Kullmann (2014). "Just a graze? Cephalic tetanus presenting as a stroke mimic". Practical neurology. 14 (1): 39–41. doi:10.1136/practneurol-2013-000541. PMID 24052566. Unknown parameter
|month=ignored (help) - ↑ "Tetanus | Diagnosis and Treatment | Lockjaw | CDC".
Historical Perspective
|
Tetanus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tetanus On the Web |
|
American Roentgen Ray Society Images of Tetanus |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4];Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [5]
Overview
In 1884 Carle and Rattone discovered tetanus by injecting animals with pus from a patient who had died of neuromuscular spasticity. In 1924, Descombey developed the tetanus toxoid, which was extensively utilized in the second world war.
Historical Perspective
In 1884 Carle and Rattone discovered tetanus by injecting animals with pus from a patient who had died of tetanus. In 1897, Nocard demonstrated that passive transformation of antitoxin had a protective effect. Kitasato found the organism in a human suffering from tetanus in 1889 and hypothesized that the disease may be reproduced when animals are injected with it. He also proposed the concept of utilization of antibodies to neutralize the toxin. Passive immunization was used for the first time in humans to treat and provide prophylaxis for tetanus during the first world war. In 1924 Descombey first developed the tetanus toxoid, which was extensively utilized in the second world war. In the same year, Nicolaier used samples of soil produced to produce tetanus by injecting animals.
Famous Tetanus Victims
- George Montagu who was an expert on birds got tetanus after stepping on a nail.
- Joe Powell who was a soccer player got tetanus after undergoing a broken arm amputation.
- Fred Thomson who was a silent film actor, also got tetanus after stepping on a nail.
- John A. Roebling who was a civil engineer and an architect and was known for his designing of bridges, in particular the Brooklyn Bridge, got tetanus after a foot amputation as result of a crash of a ferry.
- Henry David Thoreau's brother, John Thoreau also had tetanus.
- Traveller that was the favorite horse of General Robert E. Lee also acquired tetanus after stepping on a nail.
- George Crockett Strong who was during the American Civil War, was a union brigadier general, got tetanus from wounds acquired as result of the assault against Fort Wagner on Morris Island, South Carolina.
- Johann Tserclaes who was injured in the Battle of Rain by a cannon ball also acquired tetanus from this injury.
References
Pathophysiology
|
Tetanus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tetanus On the Web |
|
American Roentgen Ray Society Images of Tetanus |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [6]; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [7]
Overview
The bacteria that causes tetanus, Clostridium tetani, is usually introduced into the human body by direct inoculation of an open wound. The toxins produced by the bacterium, utilize the blood and/or lymphatics to gain access to target tissues. The toxins can act at various places in the central nervous system including the spinal cord, peripheral motor end plates, and the brain. Toxins can also act on the sympathetic nervous system.[1][2]
Pathophysiology
Tetanus is caused by an exotoxin from Clostridium tetani that leads to acute and often fatal illness. Generalized, widespread rigidity and skeletal muscle spasms are common presentations of tetanus. The muscle stiffness begins from the jaw (lockjaw) progressing to the neck and then becomes generalized. C. tetani is a terminal spore forming bacteria. The spores are resistant to extremes of temperature and to the normally used antiseptics. The spores can be found in the soil as well as in the intestines and feces of cattle, dogs, sheep, horses, cats, guinea pigs, rats, and chickens. Soil that has been treated with manure may contain a large quantity of spores. Human adults who work in agriculture may also harbor the pathogen.[3]
Pathogenesis
The pathogenesis of tetanus is as follows:[1][2][4][5][6][7][8]
- C. tetani gains access to the human body through a wound contaminated with the organism or through an umbilical stump (in cases of neonatal tetanus) by contact with contaminated medical tools.
- The spores germinate in the wound because of their anaerobic character.
- Toxins are produced and spread through the blood and lymphatics.
- C. tetani produces two exotoxins
- Tetanolysin,the function, of which, is not well understood
- Tetanospasmin, a metalloprotease, which is a neurotoxin responsible for the spasticity associated with tetanus. Tetanospasmin is among the most potent toxins known to man.
- The minimum lethal dose of tetanospasmin for humans is around 2.5 nanograms per kg of body weight or 175 nanograms for an individual who weighs 70-kg (154lb).
- The toxin uses retrograde transport along the nerve axon to reach the spinal cord and the brainstem.
- The toxins binds irreversibly with the receptors.
- The tetanus toxin cleaves the membrane proteins (SNARE proteins) that are responsible for expulsion of inhibitory neurotransmitters at the neuronal synapses.
- The disinhibition of upper motor neurons affects the lower motor neurons responsible for carrying motor cortex excitatory impulses affecting the autonomic neurons and the anterior horn cells.
- The disinhibition involving anterior horn cells leads to an unopposed contraction of the muscles, leading to excessive tone and muscular spasm which can be painful.
- The autonomic nervous system when disinhibited can lead to seizures.
- Neonatal tetanus develops within hours due to the shorter length of the axons.
Genetics
The role of genetics in the development of tetanus has not been well established. It is, however, believed that the formation of tetanus toxin is induced by the depletion of amino acids.[9]
Microscopic Pathology

References
- ↑ 1.0 1.1 Farrar JJ, Yen LM, Cook T, Fairweather N, Binh N, Parry J; et al. (2000). "Tetanus". J Neurol Neurosurg Psychiatry. 69 (3): 292–301. PMC 1737078. PMID 10945801.
- ↑ 2.0 2.1 Lalli G, Gschmeissner S, Schiavo G (2003). "Myosin Va and microtubule-based motors are required for fast axonal retrograde transport of tetanus toxin in motor neurons". J Cell Sci. 116 (Pt 22): 4639–50. doi:10.1242/jcs.00727. PMID 14576357.
- ↑ Del Pilar Morales E, Bertrán Pasarell J, Cardona Rodriguez Z, Almodovar Mercado JC, Figueroa Navarro A (2014). "Cephalic tetanus following penetrating eye trauma: a case report". Bol Asoc Med P R. 106 (2): 25–9. PMID 25065047.
- ↑ Rummel A, Bade S, Alves J, Bigalke H, Binz T (2003). "Two carbohydrate binding sites in the H(CC)-domain of tetanus neurotoxin are required for toxicity". J Mol Biol. 326 (3): 835–47. PMID 12581644.
- ↑ Schiavo G, Benfenati F, Poulain B, Rossetto O, Polverino de Laureto P, DasGupta BR; et al. (1992). "Tetanus and botulinum-B neurotoxins block neurotransmitter release by proteolytic cleavage of synaptobrevin". Nature. 359 (6398): 832–5. doi:10.1038/359832a0. PMID 1331807.
- ↑ Caccin P, Rossetto O, Rigoni M, Johnson E, Schiavo G, Montecucco C (2003). "VAMP/synaptobrevin cleavage by tetanus and botulinum neurotoxins is strongly enhanced by acidic liposomes". FEBS Lett. 542 (1–3): 132–6. PMID 12729912.
- ↑ Martha H. Roper, Jos H. Vandelaer & Francois L. Gasse (2007). "Maternal and neonatal tetanus". Lancet (London, England). 370 (9603): 1947–1959. doi:10.1016/S0140-6736(07)61261-6. PMID 17854885. Unknown parameter
|month=ignored (help) - ↑ Martha H. Roper, Jos H. Vandelaer & Francois L. Gasse (2007). "Maternal and neonatal tetanus". Lancet (London, England). 370 (9603): 1947–1959. doi:10.1016/S0140-6736(07)61261-6. PMID 17854885. Unknown parameter
|month=ignored (help) - ↑ Licona-Cassani C, Steen JA, Zaragoza NE, Moonen G, Moutafis G, Hodson MP; et al. (2016). "Tetanus toxin production is triggered by the transition from amino acid consumption to peptides". Anaerobe. 41: 113–124. doi:10.1016/j.anaerobe.2016.07.006. PMID 27492724.
Epidemiology and Demographics
|
Tetanus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tetanus On the Web |
|
American Roentgen Ray Society Images of Tetanus |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [8]; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [9]
Overview
Tetanus is an infectious disease which is not know to be contagious and can be prevented with a vaccine. There are less than 100 cases of tetanus in the US and around five deaths can be attributed to tetanus every year. There are about one million cases of tetanus reported worldwide. These according to an estimate lead to 300,000 to 500,000 deaths every year. The incidence of tetanus in the United States is 0.01 cases per 100,000 individuals. Tetanus is more commonly seen in Hispanics. Individuals greater than age 65 have a higher incidence of tetanus. Tetanus has a case fatality rate of 13.2%.[1][2][3][4] [5][6][7]
Epidemiology and Demographics
Incidence
- Between 2001 and 2008 the general incidence of tetanus in the United States was calculated to be 0.01 cases per 100,000 individuals. [1][2][3][4] [5][6][7]
- The incidence of tetanus for individuals with age more than 65 years is estimated to be 0.023 cases per 100,000 individuals.
- The incidence of tetanus in England and Whales is 0.02 cases per 100,000 individuals.
Prevalence
- The prevalence of tetanus throughout the world is almost 1 million cases.[8]
- The prevalence of tetanus in the US is less that 100 cases.
Case Fatality Rates
- Tetanus is a life threatening disease.
- There is variation in data regarding the case fatality rates of tetanus in various populations.
- The annual case fatality rate of tetanus is approximately 13.2 %.
- The case fatality rate of tetanus in developing countries is 8-50%.
- The mortality rate of neonatal tetanus is 3-88%.
- Neonatal tetanus is associated with 14% of overall neonatal deaths.
Age
- The incidence of tetanus is greater in individuals older than age 65.
Race
- Tetanus is more prevalent in Hispanics.
- Hispanics are two times more prone to have tetanus as compared to non-Hispaic individuals.
Developed Countries
- Tetanus is less common in developed countries.[9]
- There has been a 95% decrease in the reported cases of tetanus in the United States.
- Deaths in the United States as a result of tetanus have declined by 99%.
- The incidence of tetanus in England and Whales is 0.02 cases per 100,000 individuals.
Developing Countries
- Tetanus is more common in developing countries as compared to the developed countries.[9]
Trends of Tetanus in the USA
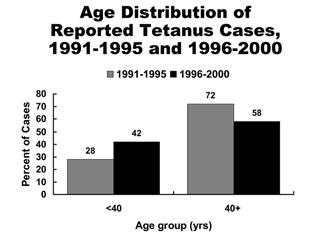
A marked decrease in mortality from tetanus occurred from the early 1900s to the late 1940s. In the late 1940s, tetanus toxoid was introduced into routine childhood immunization and tetanus became nationally notifiable. At that time, 500–600 cases (approximately 0.4 cases per 100,000 population) were reported per year. After the 1940s, reported tetanus incidence rates declined steadily. Since the mid-1970s, 50–100 cases (~0.05 cases per 100,000) have been reported annually. From 2000 through 2007 an average of 31 cases were reported per year. The death-to-case ratio has declined from 30% to approximately 10% in recent years. An all-time low of 18 cases (0.01 cases per 100,000) was reported in 2009. From 1980 through 2000, 70% of reported cases of tetanus were among persons 40 years of age or older. From 1980 through 1990, a median of 21% of reported cases were among persons younger than 40 years of age. The age distribution of reported cases shifted to a younger age group in the last half of the 1990s. Persons younger than 40 years accounted for 28% of cases during 1991–1995, increasing to 42% of cases during 1996–2000. This change in age distribution is a result of both an increase in cases in persons younger than 40 years and a decrease in cases in older people. The increase in cases among younger persons is related in part to an increased number of cases among young injection-drug users in California in the late 1990s.[1]
Almost all reported cases of tetanus are in persons who have either never been vaccinated, or who completed a primary series but have not had a booster in the preceding 10 years. Heroin users, particularly persons who inject themselves subcutaneously, appear to be at high risk for tetanus. Quinine is used to dilute heroin and may support the growth of C. tetani. Neonatal tetanus is rare in the United States, with only two cases reported since 1989. Neither of the infants' mothers had ever received tetanus toxoid. During 1998–2000 (the most recent years for which compiled data are available), acute injuries or wounds preceded tetanus in 94 (73%) of the 129 cases for which information was available. Among the most frequent wound types were puncture wounds (50%), lacerations (33%), and abrasions (9%). The most common puncture wound was from stepping on a nail (15 cases). Other puncture wounds involved barbed wire, splinters, animal or insect bites, self-piercing, and self performed tattoos. The environment in which acute injuries occurred was indoors or at home in 45%, in the yard, garden, or farm in 31%, and other outdoor locations in 23%. Five percent of reported case-patients were intravenous drug users without other known injury, and 11% had chronic wounds. Twenty patients were reported to have received at least a primary series of tetanus toxoid; 18 had an outcome reported. Among these 18 patients, one (6%) death occurred; the death was in an injection-drug user whose last dose of tetanus toxoid was 11 years before the onset of tetanus. A total of 110 patients reported fewer than three doses of tetanus toxoid or had an unknown vaccination history; 95 of these patients had an outcome reported. Nineteen (20%) deaths occurred among these 95 patients.[1]
References
- ↑ 1.0 1.1 1.2 1.3 Centers for Disease Control and Prevention (CDC) (2011). "Tetanus surveillance --- United States, 2001-2008". MMWR Morb Mortal Wkly Rep. 60 (12): 365–9. PMID 21451446.
- ↑ 2.0 2.1 "Pinkbook | Tetanus | Epidemiology of Vaccine Preventable Diseases | CDC".
- ↑ 3.0 3.1 Rushdy AA, White JM, Ramsay ME, Crowcroft NS (2003). "Tetanus in England and Wales, 1984-2000". Epidemiol Infect. 130 (1): 71–7. PMC 2869940. PMID 12613747.
- ↑ 4.0 4.1 Thwaites CL, Beeching NJ, Newton CR (2015). "Maternal and neonatal tetanus". Lancet. 385 (9965): 362–70. doi:10.1016/S0140-6736(14)60236-1. PMID 25149223.
- ↑ 5.0 5.1 C. Louise Thwaites, Nicholas J. Beeching & Charles R. Newton (2015). "Maternal and neonatal tetanus". Lancet (London, England). 385 (9965): 362–370. doi:10.1016/S0140-6736(14)60236-1. PMID 25149223. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Martha H. Roper, Jos H. Vandelaer & Francois L. Gasse (2007). "Maternal and neonatal tetanus". Lancet (London, England). 370 (9603): 1947–1959. doi:10.1016/S0140-6736(07)61261-6. PMID 17854885. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 M. H. Trujillo, A. Castillo, J. Espana, A. Manzo & R. Zerpa (1987). "Impact of intensive care management on the prognosis of tetanus. Analysis of 641 cases". Chest. 92 (1): 63–65. PMID 3595250. Unknown parameter
|month=ignored (help) - ↑ Afshar M, Raju M, Ansell D, Bleck TP (2011). "Narrative review: tetanus-a health threat after natural disasters in developing countries". Ann Intern Med. 154 (5): 329–35. doi:10.7326/0003-4819-154-5-201103010-00007. PMID 21357910.
- ↑ 9.0 9.1 World Health Organization (2000-11-01). "Maternal and Neonatal Tetanus Elimination by 2005" (PDF). Retrieved 2007-01-26.
Risk Factors
|
Tetanus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tetanus On the Web |
|
American Roentgen Ray Society Images of Tetanus |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [10] Michael Maddaleni, B.S.; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [11]
Overview
Risk factors for the development of a tetanus infection include contaminated wounds, punctured wounds, crushing, burns and working or living in poor hygiene conditions.[1][2]
Risk Factors
Risk factors for developing a tetanus infection include:[1][2][3][4][5]
- Inadequate immunization
- Never immunized for tetanus
- No booster after 10 years of last dose
- Presence of a puncture wound
- Simultaneous infection with other pathogens
- Penetrating injury with a foreign body such as a splinter or a nail
- Untreated necrotic tissue
- Crushing injuries
- Burns
- Limited ischemia
- Hiking in bat caves
- Sports injuries
- Road side accidents
Injuries that have been associated with an increased risk of tetanus include:[1][3]
- Animal bites
- Different types of dental procedures
- Wounds from surgeries
- Infection of umbilical stump in neonates
- Septic abortion
- Male circumcision (specially in sub Saharan Africa)
- Crush injuries
- Gunshot wounds
- Puncture wounds
- Burns
- Foot ulcers in diabetic patients
- Ear infections
- Compound fractures
- Intravenous drug use
- Self tattooing
Rare Conditions leading to Tetanus
Rarely, the following conditions may increase the risk of developing tetanus:[6]
- Intramuscular injections
- IV drug abuse
- Chronic sores
- Dental infections
- Superficial clean wounds
- Insect bites
- Immunocompromised (cephalic tetanus)
References
- ↑ 1.0 1.1 1.2 "Tetanus | About Tetanus Disease | Lockjaw | CDC".
- ↑ 2.0 2.1 Del Pilar Morales E, Bertrán Pasarell J, Cardona Rodriguez Z, Almodovar Mercado JC, Figueroa Navarro A (2014). "Cephalic tetanus following penetrating eye trauma: a case report". Bol Asoc Med P R. 106 (2): 25–9. PMID 25065047.
- ↑ 3.0 3.1 Grund JM, Toledo C, Davis SM, Ridzon R, Moturi E, Scobie H; et al. (2016). "Notes from the Field: Tetanus Cases After Voluntary Medical Male Circumcision for HIV Prevention--Eastern and Southern Africa, 2012-2015". MMWR Morb Mortal Wkly Rep. 65 (2): 36–7. doi:10.15585/mmwr.mm6502a5. PMID 26797167.
- ↑ Robert A. Felter & Lauren E. Zinns (2015). "Cephalic Tetanus in an Immunized Teenager: An Unusual Case Report". Pediatric emergency care. 31 (7): 511–513. doi:10.1097/PEC.0000000000000360. PMID 25853723. Unknown parameter
|month=ignored (help) - ↑ Anisha Doshi, Clare Warrell, Dima Dahdaleh & Dimitri Kullmann (2014). "Just a graze? Cephalic tetanus presenting as a stroke mimic". Practical neurology. 14 (1): 39–41. doi:10.1136/practneurol-2013-000541. PMID 24052566. Unknown parameter
|month=ignored (help) - ↑ Robert A. Felter & Lauren E. Zinns (2015). "Cephalic Tetanus in an Immunized Teenager: An Unusual Case Report". Pediatric emergency care. 31 (7): 511–513. doi:10.1097/PEC.0000000000000360. PMID 25853723. Unknown parameter
|month=ignored (help)
Causes
| style="background:#Template:Taxobox colour;"|Template:Taxobox name | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| File:Clostridium tetani 01.png Clostridium tetani with characteristic 'tennis racket' appearance.
| ||||||||||||||
| style="background:#Template:Taxobox colour;" | Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Clostridium tetani Flügge, 1881 |
|
Tetanus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tetanus On the Web |
|
American Roentgen Ray Society Images of Tetanus |
|
WikiDoc Resources for Tetanus |
|
Articles |
|---|
|
Most recent articles on Tetanus |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Tetanus at Clinical Trials.gov Clinical Trials on Tetanus at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Tetanus
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Tetanus Risk calculators and risk factors for Tetanus
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Tetanus |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [12]
Overview
Clostridium tetani is a rod-shaped, anaerobic bacterium of the genus Clostridium. Like other Clostridium species, it is Gram-positive, and its appearance on a gram stain resembles tennis rackets or drumsticks.[1] C. tetani is found as spores in soil or as parasites in the gastrointestinal tract of animals. C. tetani produces a potent biological toxin, tetanospasmin, and is the causative agent of tetanus.
Organism
Clostridium tetani is a box-car shaped, anaerobic bacterium of the genus species Clostridium. Like other Clostridium genus species, it is Gram-positive, and its appearance on a gram stain resembles tennis rackets or drumsticks.[1] C. tetani is found as spores in soil or in the gastrointestinal tract of animals. C. tetani produces a potent biological toxin, tetanospasmin, and is the causative agent of tetanus, a disease characterized by painful muscular spasms that can lead to respiratory failure and, in up to 40% of cases, death.
History
Tetanus was known to ancient people, who recognized the relationship between wounds and fatal muscle spasms. In 1884, Arthur Nicolaier isolated the strychnine-like toxin of tetanus from free-living, anaerobic soil bacteria. The etiology of the disease was further elucidated in 1890 by Antonie Carl and Giorgio Rattone, who demonstrated the transmissibility of tetanus for the first time. They produced tetanus in rabbits by injecting their sciatic nerve with pus from a fatal human tetanus case in that same year. In 1889, C. tetani was isolated from a human victim, by Kitasato Shibasaburō, who later showed that the organism could produce disease when injected into animals, and that the toxin could be neutralized by specific antibodies. In 1897, Edmond Nocard showed that tetanus antitoxin induced passive immunity in humans, and could be used for prophylaxis and treatment. Tetanus toxoid vaccine was developed by P. Descombey in 1924, and was widely used to prevent tetanus induced by battle wounds during World War II.[2]
Characteristics
C. tetani is a rod-shaped, obligate anaerobe which stains Gram positive in fresh cultures; established cultures may stain Gram negative.[1] During vegetative growth, the organism cannot survive in the presence of oxygen, is heat-sensitive and exhibits flagellar motility. As the bacterium matures, it develops a terminal spore, which gives the organism its characteristic appearance. C. tetani spores are extremely hardy as they are resistant to heat and most antiseptics.[3] The spores are distributed widely in manure-treated soils and can also be found on human skin.[2]
Vaccination
Tetanus can be prevented through the highly effective tetanus vaccine, which is a tetanus toxin inactivated with formaldehyde to be immunogenic but not pathogenic. The vaccine can be formulated as simple or adsorbed tetanus vaccine, combined tetanus and killed polio vaccine, or the older (diphtheria, tetanus, pertussis) (DPT) vaccine. Side effects are rare, but if they do occur, include fever, pain (sometimes long lasting) at the injection site, unexplained crying in infants, and irritability in older children or adults. Severe reactions are extremely rare and include anaphylaxis, seizures and encephalopathy. All infants are recommended to receive the vaccine at 2, 4, 6, and 15 months of age[citation needed]. A fifth booster dose should be given at 4–6 years of age (again, this needs a reference to the supporting data). After that, it should be given every 10 years. However, if a bite, scratch, or puncture occurs more than five years after the last dose of vaccine, the patients should receive another dose of vaccine.
Toxicity
C. tetani usually enters a host through a wound to the skin, then it replicates. High risk individuals are people exposed to soil or animal feces. The spores are widely distributed in soil and in the intestines and feces of horses, sheep, cattle, dogs, cats, rats, guinea pigs, and chickens. Manure-treated soil may contain large numbers of spores. In agricultural areas, a significant number of human adults may harbor the organism. The spores can also be found on skin surfaces and in contaminated heroin.[2] Once an infection is established, C. tetani produces two exotoxins, tetanolysin and tetanospasmin. Eleven strains of C. tetani have been identified, which differ primarily in flagellar antigens and in their ability to produce tetanospasmin. The genes for toxin production are encoded on a plasmid which is present in all toxigenic strains, and all strains that are capable of producing toxin produce identical toxins.[4] Tetanolysin serves no known benefit to C. tetani. Tetanospasmin is a neurotoxin that causes the clinical manifestations of tetanus. Tetanus toxin is generated in living bacteria, and is released when the bacteria lyse, such as during spore germination or vegetative growth. A minimal amount of spore germination and vegetative cell growth are required for toxin production.[4] Tetanus toxin is a potent neurotoxin. On the basis of weight, tetanospasmin is one of the most potent toxins known (based on tests conducted on mice). The estimated minimum human lethal dose is 2.5 nanograms per kilogram of body weight, or 175 nanograms in a 70 kg (154 lb) human.[2] The only toxins more lethal to mice are botulinum toxin, produced by close relative Clostridium botulinum and the exotoxin produced by Corynebacterium diphtheriae, the causative agent of diphtheria. It should be noted, however, that humans and other animals may react to specific toxins differently from mice, and that the overall lethality of a specific toxin likely varies between different animals. Tetanospasmin is a zinc-dependent metalloproteinase that is structurally similar to botulinum toxin, but with different effects. C. tetani synthesizes tetanospasmin as a single 150kDa polypeptide progenitor toxin that is then cleaved by a protease into two fragments; fragment A (a 50kDa "light chain") and fragment B (a 100 kDa "heavy chain") which remain connected via a disulfide bridge. Cleavage of the progenitor toxin into A and B fragments can be induced artificially by trypsin.[4]
Toxin action
Tetanospasmin released in the wound is absorbed into the circulation and reaches the ends of motor neurons all over the body. The toxin acts at several sites within the central nervous system, including nerve terminals, the spinal cord, and brain, and within the sympathetic nervous system. By binding to peripheral motor neuron terminals, the toxin enters the nerve axons, and is transported across synaptic junctions to the nerve-cell body in the brain stem and spinal cord by retrograde intraneuronal transport, until it reaches the central nervous system, where it rapidly binds to gangliosides at the presynaptic membrane of inhibitory motor nerve endings.[2] The clinical manifestations of tetanus are caused when tetanus toxin blocks inhibitory impulses, by interfering with the release of neurotransmitters, including glycine and gamma-aminobutyric acid. These inhibitory neurotransmitters inhibit the alpha motor neurons. With diminished inhibition, the resting firing rate of the alpha motor neuron increases, producing rigidity, unopposed muscle contraction and spasm. Characteristic features are risus sardonicus (a rigid smile), trismus (commonly known as "lock-jaw"), and opisthotonus (rigid, arched back). Seizures may occur, and the autonomic nervous system may also be affected. Tetanospasmin appears to prevent the release of neurotransmitters by selectively cleaving a component of synaptic vesicles called synaptobrevin II.[4] Loss of inhibition also affects preganglionic sympathetic neurons in the lateral gray matter of the spinal cord and produces sympathetic hyperactivity and high circulating catecholamine levels. Hypertension and tachycardia alternating with hypotension and bradycardia may develop.[5][6]
Genome structure
Clostridium tetani has a genome that contains 2.80 Mbp with 2,373 protein coding genes.[7]
References
- ↑ 1.0 1.1 1.2 Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. ISBN 0838585299.
- ↑ 2.0 2.1 2.2 2.3 2.4 Centers for Disease Control and Prevention (2006). "Tetanus" (PDF). In Atkinson, W; Hamborsky, J; McIntyre, L; Wolfe, S. Epidemiology and Prevention of Vaccine-Preventable Diseases (The Pink Book) (10th ed.). Public Health Foundation.
- ↑ Madigan, M; Martinko, J, eds. (2005). Brock Biology of Microorganisms (11th ed.). Prentice Hall. ISBN 0-13-144329-1.
- ↑ 4.0 4.1 4.2 4.3 Todar, Ken (2005) Pathogenic Clostridia, Ken Todar's Microbial World, University of Wisconsin - Madison.
- ↑ Loscalzo, Joseph; Fauci, Anthony S.; Braunwald, Eugene; Dennis L. Kasper; Hauser, Stephen L; Longo, Dan L. (2008). Harrison's principles of internal medicine. McGraw-Hill Medical. ISBN 0-07-146633-9.
- ↑ "Tetanus in Emergency Medicine". Emedicine. Retrieved 2011-09-01.
- ↑ Bruggemann, H.; Baumer, S.; Fricke, WF.; Wiezer, A.; Liesegang, H.; Decker, I.; Herzberg, C.; Martinez-Arias, R.; et al. (Feb 2003). "The genome sequence of Clostridium tetani, the causative agent of tetanus disease". Proc Natl Acad Sci U S A. 100 (3): 1316–21. doi:10.1073/pnas.0335853100. PMC 298770. PMID 12552129.
Further reading
- Clinical Microbiogrophy. ISBN 0-940780-49-6.
External links
- Pathema-Clostridium Resource
- Centers for Disease Control and Prevention (2012). "Ch. 20: Tetanus". In Atkinson, W; Wolfe, S; Hamborsky, J. Epidemiology and Prevention of Vaccine-Preventable Diseases (12th ed.). Washington DC: Public Health Foundation. pp. 291–300.
Differential Diagnosis

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [13] Michael Maddaleni, B.S.; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [14]
Overview
Tetanus must be differentiated from other diseases that present with fever and rigidity such as strychnine poisoning, dental infections, drug reactions, hypocalcemia, meningitis, stroke, and stiff man syndrome.[1]
Differentiating Tetanus from other Diseases
Tetanus must be differentiated from other diseases that present with fever and rigidity such as::[2][3][4]
| Disease | Diagnosis | Treatment | ||
|---|---|---|---|---|
| Symptoms | Signs | Laboratory Findings | ||
| Tetanus[5][6] |
|
|
|
|
| Neuroleptic Malignant Syndrome [7][8] |
|
|
| |
| Viral Meningitis[9][10][11] |
|
|
|
|
| Stiff man syndrome |
|
|
|
|
| Drug induced (Tardive dyskinesia)[12][13][14] |
|
|
|
|
| Strychnine poisoning[15][16][17][18] |
|
|
|
|
| Hypocalcaemia[19][20] |
|
|
|
|
| Dental abscess[21][22] |
|
|
|
|
| Parkinson's disease[23][24] |
|
|
|
|
Differential for Unilateral Involuntary Face Movements
Tetanus must also be differentiated from the following diseases that cause abnormal one sided movements of the face:[25][26][27][28][29][30][31][32][33][34][35]
- Tetanus associated trismus
- Temporomandibular joint (TMJ) dysfunction
- Unilateral jaw dystonia
- Isolated facial myokymia
- Isolated hemifacial spasm
- Multiple sclerosis (MS) associated tonic spasms
- Focal motor epilepsy
References
- ↑ Anisha Doshi, Clare Warrell, Dima Dahdaleh & Dimitri Kullmann (2014). "Just a graze? Cephalic tetanus presenting as a stroke mimic". Practical neurology. 14 (1): 39–41. doi:10.1136/practneurol-2013-000541. PMID 24052566. Unknown parameter
|month=ignored (help) - ↑ E. Andreadou, E. Kattoulas, C. Sfagos & D. Vassilopoulos (2007). "Stiff person syndrome: avoiding misdiagnosis". Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 28 (1): 35–37. doi:10.1007/s10072-007-0745-9. PMID 17385093. Unknown parameter
|month=ignored (help) - ↑ Lisa Mitchell, William Adams & Francois Aspesberro (2017). "Case 6: Episodic Stiffness in a 30-month-old Girl". Pediatrics in review. 38 (1): 52–53. doi:10.1542/pir.2014-0142. PMID 28044038. Unknown parameter
|month=ignored (help) - ↑ P. D. Thompson, J. A. Obeso, G. Delgado, J. Gallego & C. D. Marsden (1986). "Focal dystonia of the jaw and the differential diagnosis of unilateral jaw and masticatory spasm". Journal of neurology, neurosurgery, and psychiatry. 49 (6): 651–656. PMID 3734821. Unknown parameter
|month=ignored (help) - ↑ Woldeamanuel YW, Andemeskel AT, Kyei K, Woldeamanuel MW, Woldeamanuel W (2016). "Case fatality of adult tetanus in Africa: Systematic review and meta-analysis". J Neurol Sci. 368: 292–9. doi:10.1016/j.jns.2016.07.025. PMID 27538652.
- ↑ Thwaites CL, Loan HT (2015). "Eradication of tetanus". Br Med Bull. 116: 69–77. doi:10.1093/bmb/ldv044. PMC 4674006. PMID 26598719.
- ↑ Hosseini S, Elyasi F (2017). "Olanzapine-Induced Neuroleptic Malignant Syndrome". Iran J Med Sci. 42 (3): 306–309. PMC 5429500. PMID 28533580.
- ↑ Leenhardt F, Perier D, Pinzani V, Giraud I, Villiet M, Castet-Nicolas A; et al. (2017). "Pharmacist intervention to detect drug adverse events on admission to the emergency department: Two case reports of neuroleptic malignant syndrome". J Clin Pharm Ther. doi:10.1111/jcpt.12531. PMID 28488314.
- ↑ Chow E, Troy SB (2014). "The differential diagnosis of hypoglycorrhachia in adult patients". Am J Med Sci. 348 (3): 186–90. doi:10.1097/MAJ.0000000000000217. PMC 4065645. PMID 24326618.
- ↑ Leen WG, Willemsen MA, Wevers RA, Verbeek MM (2012). "Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice". PLoS One. 7 (8): e42745. doi:10.1371/journal.pone.0042745. PMC 3412827. PMID 22880096.
- ↑ Tyler KL (2004). "Herpes simplex virus infections of the central nervous system: encephalitis and meningitis, including Mollaret's". Herpes. 11 Suppl 2: 57A–64A. PMID 15319091.
- ↑ Deng ZD, Li DY, Zhang CC, Pan YX, Zhang J, Jin H; et al. (2017). "Long-term follow-up of bilateral subthalamic deep brain stimulation for refractory tardive dystonia". Parkinsonism Relat Disord. doi:10.1016/j.parkreldis.2017.05.010. PMID 28552340.
- ↑ "Valbenazine (Ingrezza) for tardive dyskinesia". Med Lett Drugs Ther. 59 (1521): 83–84. 2017. PMID 28520698.
- ↑ Voelker R (2017). "Tardive Dyskinesia Drug Approved". JAMA. 317 (19): 1942. doi:10.1001/jama.2017.5537. PMID 28510661.
- ↑ Charlotte Duverneuil, Geoffroy Lorin de la Grandmaison, Philippe de Mazancourt & Jean-Claude Alvarez (2004). "Liquid chromatography/photodiode array detection for determination of strychnine in blood: a fatal case report". Forensic science international. 141 (1): 17–21. doi:10.1016/j.forsciint.2003.12.010. PMID 15066709. Unknown parameter
|month=ignored (help) - ↑ B. A. Smith (1990). "Strychnine poisoning". The Journal of emergency medicine. 8 (3): 321–325. PMID 2197324. Unknown parameter
|month=ignored (help) - ↑ B. J. Maron, J. R. Krupp & B. Tune (1971). "Strychnine poisoning successfully treated with diazepam". The Journal of pediatrics. 78 (4): 697–699. PMID 5547830. Unknown parameter
|month=ignored (help) - ↑ B. Oberpaur, A. Donoso, C. Claveria, C. Valverde & M. Azocar (1999). "Strychnine poisoning: an uncommon intoxication in children". Pediatric emergency care. 15 (4): 264–265. PMID 10460082. Unknown parameter
|month=ignored (help) - ↑ Chhabra P, Rana SS, Sharma V, Sharma R, Bhasin DK (2016). "Hypocalcemic tetany: a simple bedside marker of poor outcome in acute pancreatitis". Ann Gastroenterol. 29 (2): 214–20. doi:10.20524/aog.2016.0015. PMC 4805743. PMID 27065735.
- ↑ Desai M, Kolla PK, Reddy PL (2013). "Calcium unresponsive hypocalcemic tetany: gitelman syndrome with hypocalcemia". Case Rep Med. 2013: 197374. doi:10.1155/2013/197374. PMC 3792521. PMID 24171002.
- ↑ Ogle OE (2017). "Odontogenic Infections". Dent Clin North Am. 61 (2): 235–252. doi:10.1016/j.cden.2016.11.004. PMID 28317564.
- ↑ Bertossi D, Barone A, Iurlaro A, Marconcini S, De Santis D, Finotti M; et al. (2017). "Odontogenic Orofacial Infections". J Craniofac Surg. 28 (1): 197–202. doi:10.1097/SCS.0000000000003250. PMID 27930461.
- ↑ Olanow CW, Watts RL, Koller WC (2001). "An algorithm (decision tree) for the management of Parkinson's disease (2001): treatment guidelines". Neurology. 56 (11 Suppl 5): S1–S88. PMID 11402154.
- ↑ Connolly BS, Lang AE (2014). "Pharmacological treatment of Parkinson disease: a review". JAMA. 311 (16): 1670–83. doi:10.1001/jama.2014.3654. PMID 24756517.
- ↑ P. D. Thompson, J. A. Obeso, G. Delgado, J. Gallego & C. D. Marsden (1986). "Focal dystonia of the jaw and the differential diagnosis of unilateral jaw and masticatory spasm". Journal of neurology, neurosurgery, and psychiatry. 49 (6): 651–656. PMID 3734821. Unknown parameter
|month=ignored (help) - ↑ J. R. Berger, W. A. Sheremata & E. Melamed (1984). "Paroxysmal dystonia as the initial manifestation of multiple sclerosis". Archives of neurology. 41 (7): 747–750. PMID 6743065. Unknown parameter
|month=ignored (help) - ↑ W. B. Matthews (1975). "Paroxysmal symptoms in multiple sclerosis". Journal of neurology, neurosurgery, and psychiatry. 38 (6): 617–623. PMID 1151430. Unknown parameter
|month=ignored (help) - ↑ P. D. Thompson & W. M. Carroll (1983). "Hemimasticatory spasm--a peripheral paroxysmal cranial neuropathy?". Journal of neurology, neurosurgery, and psychiatry. 46 (3): 274–276. PMID 6842234. Unknown parameter
|month=ignored (help) - ↑ P. D. Thompson & W. M. Carroll (1983). "Hemimasticatory and hemifacial spasm: a common pathophysiology?". Clinical and experimental neurology. 19: 110–119. PMID 6568919.
- ↑ L. R. Jenkyn, D. B. Walsh, C. M. Culver & A. G. Reeves (1977). "Clinical signs in diffuse cerebral dysfunction". Journal of neurology, neurosurgery, and psychiatry. 40 (10): 956–966. PMID 591973. Unknown parameter
|month=ignored (help) - ↑ J. D. Rugh & W. K. Solberg (1976). "Psychological implications in temporomandibular pain and dysfunction". Oral sciences reviews. 7: 3–30. PMID 775369.
- ↑ Bond WS (1984). "Detection and management of the neuroleptic malignant syndrome". Clin Pharm. 3 (3): 302–7. PMID 6145537.
- ↑ S. Fahn, S. B. Bressman & C. D. Marsden (1998). "Classification of dystonia". Advances in neurology. 78: 1–10. PMID 9750897.
- ↑ Howard L. Geyer & Susan B. Bressman (2006). "The diagnosis of dystonia". The Lancet. Neurology. 5 (9): 780–790. doi:10.1016/S1474-4422(06)70547-6. PMID 16914406. Unknown parameter
|month=ignored (help) - ↑ Christine Klein & Laurie J. Ozelius (2002). "Dystonia: clinical features, genetics, and treatment". Current opinion in neurology. 15 (4): 491–497. PMID 12151848. Unknown parameter
|month=ignored (help)
Natural History, Complications & Prognosis
Natural History
|
Tetanus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tetanus On the Web |
|
American Roentgen Ray Society Images of Tetanus |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [15]; Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [16]
Overview
Tetanus can have an incubation period of 2 to 38 days. The presentation and progression may vary depending on the type of tetanus. Generalized tetanus can involve the diaphragm making it difficult to breathe. The complications of tetanus include respiratory arrest, fractures, laryngospasm, aspiration pneumonia and pulmonary embolism. Tetanus has a case fatality rate of approximately 11%. The fatality rate of tetanus is associated with prolonged convulsions and contractions. Tetanus without spasms has an excellent prognosis. Early diagnosis is associated with a good prognosis.[1][2]
Natural History
Tetanus can have an incubation period of 2 to 38 days. Initial presentation involves neck and jaw stiffness. Spasms are common in the first week and may persist for up to 3 weeks, followed by rigidity that can persist for 4-8 weeks. Patients with the generalized type can have spasmodic contractions of the muscles associated with inability to breathe which may lead to apnea. If left untreated this can lead to the death.[1][3]
Complications
Complications of a tetanus infection may include:
- Respiratory or diaphragmatic paralysis
- Laryngospasm
- This can be associated with spasms of the muscles of respiration which leads to breathing difficulties.
- Fractures of the spine or long bones
- This may result from prolonged contractions and convulsions
- Hyperactivity of autonomic nervous system
- This may lead to an abnormal heart rhythm and/or hypertension
- Nosocomial infections
- Common because of prolonged hospitalization
- Pulmonary embolism
- Apparent in drug users and the elderly
- Aspiration pneumonia
- Common late complication
- Found in 50%-70% of autopsied cases
Common secondary complications of prolonged hospitalization for tetanus include:
- Sepsis from indwelling catheters
- Hospital-acquired pneumonia
- Decubitus ulcers
Prognosis
Tetanus results in death in approximately 10-20% of cases. The mortality rate is higher among older people. The fatality rate of tetanus is associated with prolonged contractions and convulsions. Tetanus without spasms has an excellent prognosis. Early diagnosis is associated with a good prognosis.[1][4][5][6][7]
- Poor prognostic factors include:
- Individuals of age 60 years or older (approximately 18%)
- Unvaccinated people (approximately 22%)
- Delayed diagnosis
References
- ↑ 1.0 1.1 1.2 Thwaites CL, Beeching NJ, Newton CR (2015). "Maternal and neonatal tetanus". Lancet. 385 (9965): 362–70. doi:10.1016/S0140-6736(14)60236-1. PMID 25149223.
- ↑ J. C. Patel & B. C. Mehta (1999). "Tetanus: study of 8,697 cases". Indian journal of medical sciences. 53 (9): 393–401. PMID 10710833. Unknown parameter
|month=ignored (help) - ↑ "Tetanus | Symptoms and Complications | Lockjaw | CDC".
- ↑ C. Louise Thwaites, Nicholas J. Beeching & Charles R. Newton (2015). "Maternal and neonatal tetanus". Lancet (London, England). 385 (9965): 362–370. doi:10.1016/S0140-6736(14)60236-1. PMID 25149223. Unknown parameter
|month=ignored (help) - ↑ Martha H. Roper, Jos H. Vandelaer & Francois L. Gasse (2007). "Maternal and neonatal tetanus". Lancet (London, England). 370 (9603): 1947–1959. doi:10.1016/S0140-6736(07)61261-6. PMID 17854885. Unknown parameter
|month=ignored (help) - ↑ M. H. Trujillo, A. Castillo, J. Espana, A. Manzo & R. Zerpa (1987). "Impact of intensive care management on the prognosis of tetanus. Analysis of 641 cases". Chest. 92 (1): 63–65. PMID 3595250. Unknown parameter
|month=ignored (help) - ↑ J. C. Patel & B. C. Mehta (1999). "Tetanus: study of 8,697 cases". Indian journal of medical sciences. 53 (9): 393–401. PMID 10710833. Unknown parameter
|month=ignored (help)
Diagnosis
{{#ask:Used To Diagnose::Tetanus |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTestQuery |sort=Sort Order }}
Treatment
{{#ask:Used To Treat::Tetanus |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery |sort=Sort Order }} {{#ask:Prevents::Tetanus |?Sort Order |intro= | |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery2 |sort=Sort Order }}
- Pages with reference errors
- CS1 maint: Extra text
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- CS1 maint: Extra text: authors list
- Pages with citations using unsupported parameters
- Disease
- Bacterial diseases
- Emergency mdicine
- Up-To-Date
- Infectious disease
- Neurology
- Needs overview
- All articles with unsourced statements
- Articles with unsourced statements from April 2015
- Articles with invalid date parameter in template
- Clostridiaceae
- Gram-positive bacteria
- Tetanus
- Bacteria with sequenced genomes
- Needs content