Splenic infarction
| Splenic infarction | |
 | |
|---|---|
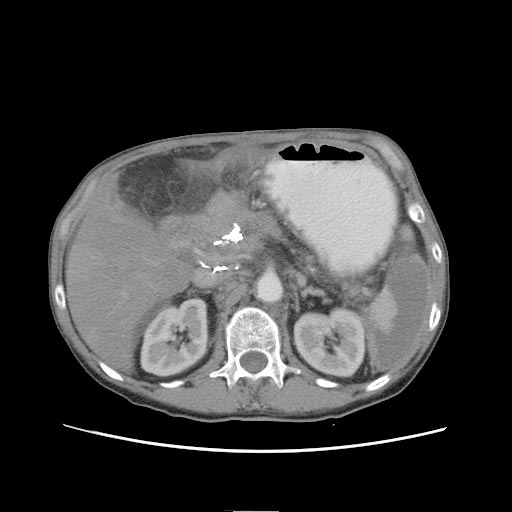
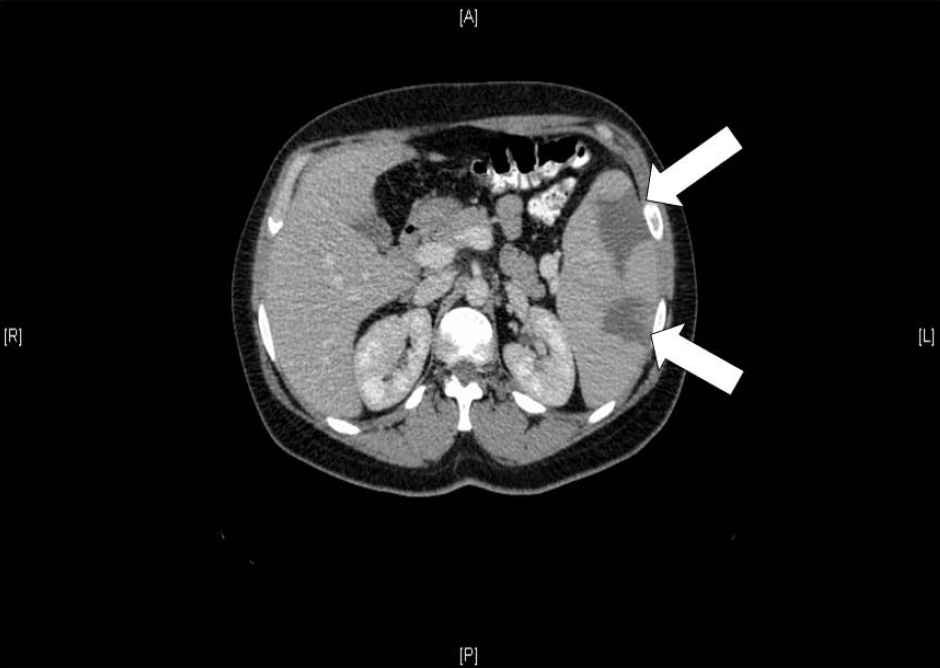
| Two large splenic infarcts, as demonstrated on an abdominal CT scan (white arrows) in a 36-year-old Caucasian woman with acute cytomegalovirus infection. The patient was also found to be heterozygous for the Factor V Leiden mutation. | |
| ICD-10 | D73.5 |
| DiseasesDB | 12365 |
| MedlinePlus | 001293 |
| MeSH | D013159 |
|
Splenic infarction Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Splenic infarction On the Web |
|
American Roentgen Ray Society Images of Splenic infarction |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Diagnosis
Laboratory tests
- Laboratory tests are not diagnostic for splenic infarction, although in a few cases there is leucocytosis, thrombocytosis, and anaemia.
Imaging Studies
Radiological imaging tests are diagnostic. Ultrasound imaging is useful in cases where the splenic parenchyma can be visualized, but significant amount of luminal bowel gas, as well as morbid obesity, render this modality less useful.
- Computerized tomography scan is the current diagnostic modality of choice. Prior to the CT era, diagnosis of splenic infarct was made most commonly at laparotomy for intra-abdominal catastrophe or on postmortem examination. An abdominal CT scan is the most commonly used modality to confirm the diagnosis,[1] although abdominal ultrasound can also contribute.[2][3][4] In CT; focal infarcts appear as wedge-shaped areas of decreased attenuation that extend to the surface of the spleen. Global infarction can manifest as diffuse areas of decreased attenuation in the spleen and can mimic splenic abscess or tumor. In some cases of global infarction, the splenic periphery remains enhanced due to perfusion from capsular vessels.
Patient #1 Note peripheral enhancement due to perfusion from capsular vessels
-
CT: Splenic infarction
-
CT: Splenic infarction
-
CT: Splenic infarction
Patient #2 Note peripheral enhancement due to perfusion from capsular vessels
-
CT: Splenic infarction
-
CT: Splenic infarction
-
CT: Splenic infarction
- Contrast studies clearly depict the classic segmental wedge-shaped, low-attenuation defect. Less frequently, the entire spleen may be infarcted, leaving only a rim of contrast-enhancing capsule.
- Other modes of diagnosis include radioisotope scans and ultrasound evaluation of the spleen.
- Angiography is indicated when a vascular lesion is suspected as the etiologic cause, as in cases of arterial embolization, or to manage segmental bleeding by embolization.
- Magnetic resonance imaging is another useful modality that clearly identifies infarcted splenic parenchyma. Magnetic resonance images may be reconstructed easily in 3 dimensions (as can spiral CT scan images) if the images are obtained using gadolinium contrast.
Treatment
There is no specific treatment, except treating the underlying disorder and providing adequate pain relief. Splenectomy is only required if complications ensue; surgical removal predisposes to overwhelming post-splenectomy infections.[5]
Medical therapy
Surgery is indicated only in the presence of complications. Otherwise, the infarcted spleen can be left in situ, and the patient is observed. Due to the rarity of this disorder and the largely anecdotal character of many reports, the roles of antibiotics and antiplatelet agents (for the treatment of thrombocytosis) have not been formally addressed. Similarly, no scientifically supported information exists regarding the possible increase in susceptibility to overwhelming postsplenectomy sepsis in these patients.
The principal mainstay of medical therapy is analgesia with either narcotics or nonsteroidal anti-inflammatory agents.
In one series of 59 patients, mortality amounted to 5%.[1] Complications include a ruptured spleen, hemorrhage, splenic abscess (for example, if the underlying cause is endocarditis) or pseudocyst formation. Splenectomy may be warranted for persistent pseudocysts due to the high risk of subsequent rupture.[6]
Surgical therapy
- For an infarcted spleen with any of the above-mentioned complications, splenectomy is required.
- Because of the small but real risk of fatal overwhelming post splenectomy sepsis, splenic preservation is preferable whenever possible.
- In cases of torsion of a wandering spleen, splenopexy with splenic salvage is the procedure of choice in the well-perfused, non infarcted spleen.
- Complications such as bleeding or pseudocyst formation also may be amenable to splenic salvage using techniques of partial splenectomy.
- While a unilocular abscess can be managed successfully in select cases with percutaneous catheter drainage, some authors advocate splenectomy in all cases of splenic infarct and abscess, questioning the utility of preserving the residual partially functioning spleen. This may be accomplished using traditional open techniques or laparoscopic techniques.
- Perisplenic inflammation and dense adhesions can make splenectomy difficult. Another choice is to perform preoperative splenic artery embolization, which purposely infarcts the remaining spleen and minimizes blood loss that otherwise can be quite profuse in these difficult dissections.
Intraoperative ligation of the splenic artery at the superior margin of the pancreas in the lesser sac is another alternative to minimize blood loss if the spleen is enlarged.
Contraindications:
- Asymptomatic infarct without complication does not require surgical intervention.
- Overall, most splenic infarcts do not require surgical intervention.
Source
- Guth AA, Pachter HL, Kaplan LJ et. al., Splenic Infarct, [3]
References
- ↑ 1.0 1.1 Nores M, Phillips EH, Morgenstern L, Hiatt JR (1998). "The clinical spectrum of splenic infarction". Am Surg. 64 (2): 182–8. PMID 9486895. Unknown parameter
|month=ignored (help) - ↑ Görg C, Seifart U, Görg K (2004). "Acute, complete splenic infarction in cancer patient is associated with a fatal outcome". Abdom Imaging. 29 (2): 224–7. doi:10.1007/s00261-003-0108-9. PMID 15290950.
- ↑ O'Keefe JH, Holmes DR, Schaff HV, Sheedy PF, Edwards WD (1986). "Thromboembolic splenic infarction". Mayo Clin. Proc. 61 (12): 967–72. PMID 3773568. Unknown parameter
|month=ignored (help) - ↑ Frippiat F, Donckier J, Vandenbossche P, Stoffel M, Boland B, Lambert M (1996). "Splenic infarction: report of three cases of atherosclerotic embolization originating in the aorta and retrospective study of 64 cases". Acta Clin Belg. 51 (6): 395–402. PMID 8997756.
- ↑ Salvi PF, Stagnitti F, Mongardini M, Schillaci F, Stagnitti A, Chirletti P (2007). "Splenic infarction, rare cause of acute abdomen, only seldom requires splenectomy. Case report and literature review". Ann Ital Chir. 78 (6): 529–32. PMID 18510036.
- ↑ Pachter HL, Hofstetter SR, Elkowitz A, Harris L, Liang HG (1993). "Traumatic cysts of the spleen--the role of cystectomy and splenic preservation: experience with seven consecutive patients". J Trauma. 35 (3): 430–6. PMID 8371303. Unknown parameter
|month=ignored (help)
Additional Resources
- Argiris A: Splenic and renal infarctions complicating atrial fibrillation. Mt Sinai J Med 1997 Sep-Oct; 64(4-5): 342-9[Medline].
- Balcar I, Seltzer SE, Davis S: CT patterns of splenic infarction: a clinical and experimental study. Radiology 1984 Jun; 151(3): 723-9.
- Cohen BA, Mitty HA, Mendelson DS: Computed tomography of splenic infarction. J Comput Assist Tomogr 1984 Feb; 8(1): 167-8.
- Desai DC, Hebra A, Davidoff AM: Wandering spleen: a challenging diagnosis. South Med J 1997 Apr; 90(4): 439-43.
- Franklin QJ, Compeggie M: Splenic syndrome in sickle cell trait: four case presentations and a review of the literature. Mil Med 1999 Mar; 164(3): 230-3.
- Goerg C, Schwerk WB: Splenic infarction: sonographic patterns, diagnosis, follow-up, and complications. Radiology 1990 Mar; 174(3 Pt 1): 803-7.
- Jaroch MT, Broughan TA, Hermann RE: The natural history of splenic infarction. Surgery 1986 Oct; 100(4): 743-50.
- Kluger Y, Paul DB, Townsend RN: Enhanced rim around infarcted, traumatized spleen on computed tomographic scans: case report. J Trauma 1994 Mar; 36(3): 436-7.
- Lo AY, Reich H, Harvey J: Splenic infarction associated with adult respiratory distress syndrome. Mt Sinai J Med 1994 Sep; 61(4): 369-71.
- Nores M, Phillips EH, Morgenstern L: The clinical spectrum of splenic infarction. Am Surg 1998 Feb; 64(2): 182-8.
- O'Keefe JH Jr, Holmes DR Jr, Schaff HV: Thromboembolic splenic infarction. Mayo Clin Proc 1986 Dec; 61(12): 967-72.
- Pachter HL, Hofstetter SR, Elkowitz A: Traumatic cysts of the spleen--the role of cystectomy and splenic preservation: experience with seven consecutive patients. J Trauma 1993 Sep; 35(3): 430-6.
- Pachter HL, Guth AA, Hofstetter SR: Changing patterns in the management of splenic trauma: the impact of nonoperative management. Ann Surg 1998 May; 227(5): 708-17; discussion 717-9.
- Shackford SR, Wald SL, Ross SE: The clinical utility of computed tomographic scanning and neurologic examination in the management of patients with minor head injuries. J Trauma 1992 Sep; 33(3): 385-94.
- Sheikha A: Splenic syndrome in patients at high altitude with unrecognized sickle cell trait: splenectomy is often unnecessary. Can J Surg 2005; 48: 377-381.
- Torda A: Postpartum toxic shock syndrome associated with multiple splenic infarcts. Med J Aust 2005; 182: 93.
- Walcher F, Schneider G, Marzi I: Torsion of a wandering spleen after blunt abdominal trauma. J Trauma 1997 Dec; 43(6): 983-4.
- Yu LK, Hsu CW, Liu NJ: Splenic infarction complicated by splenic artery occlusion after N-butyl-2-cyanoacrylate injection for gastric varices: case report. Gastrointest Endosc 2005; 61: 343-345.