Secondary hyperparathyroidism (patient information): Difference between revisions
| (31 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
'''For the WikiDoc page for this topic, click [[Secondary hyperparathyroidism|here]]''' | '''For the WikiDoc page for this topic, click [[Secondary hyperparathyroidism|here]]''' | ||
{{Infobox_Disease | | |||
Name = Secondary hyperparathyroidism | | |||
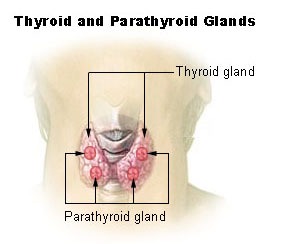
Image = Illu thyroid parathyroid.jpg | | |||
Caption = Thyroid and parathyroid. | | |||
DiseasesDB = 6301 | | |||
ICD10 = {{ICD10|E|21|1|e|20}} | | |||
ICD9 = {{ICD9|252.02}}, {{ICD9|588.81}} | | |||
ICDO = | | |||
OMIM = | | |||
MedlinePlus = | | |||
eMedicineSubj = | | |||
eMedicineTopic = | | |||
MeshID = D006962 | | |||
}} | |||
{{Secondary hyperparathyroidism (patient information)}} | |||
{{ | {{CMG}}; '''Associate Editor-In-Chief:''' Jinhui Wu, M.Dd | ||
==Overview== | |||
Secondary hyperparathyroidism is an endocrine disorder that the parathyroid glands produce too much [[parathyroid hormone]] (PTH). The most important cause of secondary hyperparathyroidism is [[chronic renal failure]]. Other causes include [[rickets]], [[malnutrition]] or [[malabsorption]], and certain types of [[cancer]]. Signs and symptoms include symptoms of diseases above, such as [[weakness]], poor growth, bowed limbs and swollen joints in children, [[bone pain]], [[osteomalacia]], [[osteoporosis]], [[fractures]], even symptoms of certain cancer. Blood tests of parathyroid hormone and biochemistry, and imaging tests may help the diagnosis of secondary hyperparathyroidism. Treatments and prognosis of secondary hyperparathyroidism depend on the underlying cause. | |||
==What are the symptoms of Secondary hyperparathyroidism?== | |||
==What | |||
Symptoms of secondary hyperparathyroidism include symptoms of [[chronic renal failure]], [[malabsorption]], [[rickets]] and underlying cancer. General symptoms are the following: | Symptoms of secondary hyperparathyroidism include symptoms of [[chronic renal failure]], [[malabsorption]], [[rickets]] and underlying cancer. General symptoms are the following: | ||
:*[[Weakness]] | :*[[Weakness]] | ||
:*Poor growth, | :*[[Bone deformities]] | ||
:*Poor growth, bowed limbs and swollen joints in children | |||
:*[[Bone pain]] | :*[[Bone pain]] | ||
:*[[Osteomalacia]], [[osteoporosis]] | :*[[Osteomalacia]], [[osteoporosis]] | ||
:*[[Fracture]]s | :*[[Fracture]]s | ||
==Who is at risk | ==Who is at highest risk?== | ||
:*Kidney disease, [[chronic renal failure]] | |||
:*[[Rickets]] | :*[[Rickets]] | ||
:*[[Malnutrition]], [[malabsorption]], [[vitamin D deficiency]] | :*[[Malnutrition]], [[malabsorption]], [[vitamin D deficiency]] | ||
:*Certain types of [[cancer]] | :*Certain types of [[cancer]] | ||
== | ==What causes Secondary hyperparathyroidism?== | ||
The [[parathyroid gland]]s help control [[calcium]] use and removal by the body. They do this by producing [[parathyroid hormone]], or [[PTH]]. [[PTH]] helps control [[calcium]], [[phosphorus]], and [[vitamin D]] levels within the [[blood]] and [[bone]]. | |||
When calcium levels are too low, the body responds by increasing production of [[parathyroid hormone]]. This increase in [[parathyroid hormone]] causes more [[calcium]] to be taken from the bone and more [[calcium]] to be reabsorbed by the [[intestine]]s and [[kidney]]. | |||
Medical conditions that cause [[low blood calcium]] levels or interfere with the body's ability to break down and remove phosphate can lead to secondary hyperparathyroidism. Too much [[phosphate]] causes changes in calcium levels. | |||
[[Kidney failure]] is a common cause of secondary hyperparathyroidism. [[Kidney failure]] can interfere with the body's ability to remove [[phosphate]]. | |||
Other causes of secondary hyperparathyroidism may include: | |||
* Calcium deficiency | |||
** Not enough [[calcium]] in the diet | |||
** Too much [[calcium]] loss in the urine | |||
* Conditions that make it hard for the body to break down phosphate, including: | |||
** [[Aluminum]] poisoning | |||
** Certain types of [[cancer]] | |||
** Kidney disease | |||
** [[Malnutrition]] | |||
** [[Malabsorption]] | |||
* Vitamin D disorders (often seen in children with malnutrition and older adults who do not get enough sunlight): | |||
** Problems absorbing vitamin D into the body ([[malabsorption]]) | |||
** Problems breaking down [[vitamin D]] (due to the use of certain drugs) | |||
** [[Rickets]] | |||
** Too little [[vitamin D ]](deficiency) | |||
==Diagnosis== | |||
:*Blood tests: Patients with secondary hyperparathyroidism may indicate signs, such as elevated levels of [[parathyroid hormone]] (PTH), a low serum [[calcium]], and an abnormal serum phosphorus. Blood tests can also check renal functions of the patients. | :*Blood tests: Patients with secondary hyperparathyroidism may indicate signs, such as elevated levels of [[parathyroid hormone]] (PTH), a low serum [[calcium]], and an abnormal serum phosphorus. Blood tests can also check renal functions of the patients. | ||
:*Bone densitometry: The doctor may arrange a dual x-ray absorptiometry to determine bone density and to reveal bone loss, [[fracture]]s, or bone softening. | :*[[Bone densitometry]]: The doctor may arrange a dual x-ray absorptiometry to determine bone density and to reveal bone loss, [[fracture]]s, or bone softening. | ||
:*Imaging tests: Imaging tests such as x- | :*Imaging tests: Imaging tests such as [[x-ray]]s, [[ultrasound]], [[CT]] or [[MRI]] scans of the kidneys and nuclear imaging may show signs of calcium deposits or a blockage, certain type of [[cancer]]. | ||
==When to seek urgent medical care?== | ==When to seek urgent medical care?== | ||
Call your health care provider if you have symptoms of secondary hyperparathyroidism , particularly if you are being treated for kidney disease. If you suffer either of the following symptoms, seeking urgent medical care as soon as possible: | |||
:*[[Bone pain]] | |||
:*[[Fracture]]s | |||
==Treatment options== | ==Treatment options== | ||
Correcting the calcium level and the underlying problem can bring the [[PTH]] levels back to normal. | |||
Treatment may involve: | |||
* A special form of [[vitamin D]] (requires a doctor's prescription) if you have low [[vitamin D]] levels | |||
* Surgery for [[cancer]] | |||
Patients with [[chronic kidney failure]] are usually given [[calcium]] and [[vitamin D]], and are told to avoid [[phosphate]] in their diet. A medication called [[cinacalcet]] ([[Sensipar]]) may also be recommended. [[Dialysis]], a [[kidney transplant]], or parathyroid surgery may be needed. | |||
==Diseases with similar symptoms== | ==Diseases with similar symptoms== | ||
:*[[Rickets]] | |||
:*[[Gout]] | |||
:*[[Ewing's Sarcoma]] | |||
:*[[Chondroblastoma]] | |||
:*Bone metastases | |||
==Where to find medical care for secondary hyperparathyroidism?== | ==Where to find medical care for secondary hyperparathyroidism?== | ||
| Line 39: | Line 101: | ||
==Prevention of secondary hyperparathyroidism== | ==Prevention of secondary hyperparathyroidism== | ||
Early diagnosis and treatment of rickets or vitamin D deficiency may prevent this condition. Proper treatment of kidney failure helps reduce symptoms of secondary hyperparathyroidism. | |||
==What to expect (Outook/Prognosis)?== | ==What to expect (Outook/Prognosis)?== | ||
The prognosis of secondary hyperparathyroidism depends on the underlying cause. | |||
==Possible complications== | |||
Persons with kidney problems may continue to produce too much [[parathyroid hormone]] even when their [[calcium]] level is back to normal. This is called "tertiary hyperthyroidism." Parathyroid surgery may be needed. | |||
Other complications include: | |||
* Increased risk of broken bones | |||
* [[Renal osteodystrophy]] (a condition that causes bone pain, weakness, and fractures) | |||
http:// | ==Sources== | ||
http://www.nlm.nih.gov/medlineplus/ency/article/000318.htm | |||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category:Patient | |||
[[Category:Patient information]] | |||
[[Category:Endocrinology patient information]] | |||
[[Category:Endocrinology]] | |||
[[Category:Mature chapter]] | |||
[[Category:Disease]] | |||
Latest revision as of 18:06, 20 September 2012
For the WikiDoc page for this topic, click here
| Secondary hyperparathyroidism | |
 | |
|---|---|
| Thyroid and parathyroid. | |
| ICD-10 | E21.1 |
| ICD-9 | 252.02, 588.81 |
| DiseasesDB | 6301 |
| MeSH | D006962 |
|
Secondary hyperparathyroidism |
|
Where to find medical care for Secondary hyperparathyroidism? |
|---|
|
Secondary hyperparathyroidism On the Web |
|
Directions to Hospitals Treating Secondary hyperparathyroidism |
|
Risk calculators and risk factors for Secondary hyperparathyroidism |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Jinhui Wu, M.Dd
Overview
Secondary hyperparathyroidism is an endocrine disorder that the parathyroid glands produce too much parathyroid hormone (PTH). The most important cause of secondary hyperparathyroidism is chronic renal failure. Other causes include rickets, malnutrition or malabsorption, and certain types of cancer. Signs and symptoms include symptoms of diseases above, such as weakness, poor growth, bowed limbs and swollen joints in children, bone pain, osteomalacia, osteoporosis, fractures, even symptoms of certain cancer. Blood tests of parathyroid hormone and biochemistry, and imaging tests may help the diagnosis of secondary hyperparathyroidism. Treatments and prognosis of secondary hyperparathyroidism depend on the underlying cause.
What are the symptoms of Secondary hyperparathyroidism?
Symptoms of secondary hyperparathyroidism include symptoms of chronic renal failure, malabsorption, rickets and underlying cancer. General symptoms are the following:
- Weakness
- Bone deformities
- Poor growth, bowed limbs and swollen joints in children
- Bone pain
- Osteomalacia, osteoporosis
- Fractures
Who is at highest risk?
- Kidney disease, chronic renal failure
- Rickets
- Malnutrition, malabsorption, vitamin D deficiency
- Certain types of cancer
What causes Secondary hyperparathyroidism?
The parathyroid glands help control calcium use and removal by the body. They do this by producing parathyroid hormone, or PTH. PTH helps control calcium, phosphorus, and vitamin D levels within the blood and bone.
When calcium levels are too low, the body responds by increasing production of parathyroid hormone. This increase in parathyroid hormone causes more calcium to be taken from the bone and more calcium to be reabsorbed by the intestines and kidney.
Medical conditions that cause low blood calcium levels or interfere with the body's ability to break down and remove phosphate can lead to secondary hyperparathyroidism. Too much phosphate causes changes in calcium levels.
Kidney failure is a common cause of secondary hyperparathyroidism. Kidney failure can interfere with the body's ability to remove phosphate.
Other causes of secondary hyperparathyroidism may include:
- Calcium deficiency
- Conditions that make it hard for the body to break down phosphate, including:
- Aluminum poisoning
- Certain types of cancer
- Kidney disease
- Malnutrition
- Malabsorption
- Vitamin D disorders (often seen in children with malnutrition and older adults who do not get enough sunlight):
- Problems absorbing vitamin D into the body (malabsorption)
- Problems breaking down vitamin D (due to the use of certain drugs)
- Rickets
- Too little vitamin D (deficiency)
Diagnosis
- Blood tests: Patients with secondary hyperparathyroidism may indicate signs, such as elevated levels of parathyroid hormone (PTH), a low serum calcium, and an abnormal serum phosphorus. Blood tests can also check renal functions of the patients.
- Bone densitometry: The doctor may arrange a dual x-ray absorptiometry to determine bone density and to reveal bone loss, fractures, or bone softening.
- Imaging tests: Imaging tests such as x-rays, ultrasound, CT or MRI scans of the kidneys and nuclear imaging may show signs of calcium deposits or a blockage, certain type of cancer.
When to seek urgent medical care?
Call your health care provider if you have symptoms of secondary hyperparathyroidism , particularly if you are being treated for kidney disease. If you suffer either of the following symptoms, seeking urgent medical care as soon as possible:
Treatment options
Correcting the calcium level and the underlying problem can bring the PTH levels back to normal.
Treatment may involve:
- A special form of vitamin D (requires a doctor's prescription) if you have low vitamin D levels
- Surgery for cancer
Patients with chronic kidney failure are usually given calcium and vitamin D, and are told to avoid phosphate in their diet. A medication called cinacalcet (Sensipar) may also be recommended. Dialysis, a kidney transplant, or parathyroid surgery may be needed.
Diseases with similar symptoms
- Rickets
- Gout
- Ewing's Sarcoma
- Chondroblastoma
- Bone metastases
Where to find medical care for secondary hyperparathyroidism?
Directions to Hospitals Treating secondary hyperparathyroidism
Prevention of secondary hyperparathyroidism
Early diagnosis and treatment of rickets or vitamin D deficiency may prevent this condition. Proper treatment of kidney failure helps reduce symptoms of secondary hyperparathyroidism.
What to expect (Outook/Prognosis)?
The prognosis of secondary hyperparathyroidism depends on the underlying cause.
Possible complications
Persons with kidney problems may continue to produce too much parathyroid hormone even when their calcium level is back to normal. This is called "tertiary hyperthyroidism." Parathyroid surgery may be needed.
Other complications include:
- Increased risk of broken bones
- Renal osteodystrophy (a condition that causes bone pain, weakness, and fractures)