Schistosomiasis laboratory findings: Difference between revisions
Aditya Ganti (talk | contribs) No edit summary |
Aditya Ganti (talk | contribs) |
||
| (21 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Schistosomiasis}} | {{Schistosomiasis}} | ||
{{CMG}} | {{CMG}} ; {{AE}} {{ADG}} | ||
==Overview== | ==Overview== | ||
Methods for diagnosing schistosomiasis include visualization of Schistosoma eggs in [[stool]], [[urine]], and crushed [[Biopsy|biopsy tissues]]. [[Serological testing|serologic assays]] and urinary antigen testing have also been used. Laboratory findings consistent with the diagnosis of schistosomiasis include detection of circulating [[antibodies]] to schistosomes and schistosomal [[antigen]] in [[serum]]. | |||
==Laboratory Findings== | ==Laboratory Findings== | ||
Visualization of | Visualization of Schistosoma eggs in [[stool]], [[urine]], and [[Biopsy|crushed biopsy tissues]] is diagnostic of schistosomiasis. Laboratory findings consistent with the diagnosis of schistosomiasis include detection of circulating [[antibodies]] to schistosomes and schistosomal [[antigen]] in [[serum]]. Diagnostic tests for schistosomiasis include the following:<ref name="pmid21633040">{{cite journal |vauthors=Ibironke OA, Phillips AE, Garba A, Lamine SM, Shiff C |title=Diagnosis of Schistosoma haematobium by detection of specific DNA fragments from filtered urine samples |journal=Am. J. Trop. Med. Hyg. |volume=84 |issue=6 |pages=998–1001 |year=2011 |pmid=21633040 |pmc=3110375 |doi=10.4269/ajtmh.2011.10-0691 |url=}}</ref><ref name="urlCDC - DPDx - Schistosomiasis Infection - Laboratory Diagnosis">{{cite web |url=https://www.cdc.gov/dpdx/schistosomiasis/dx.html |title=CDC - DPDx - Schistosomiasis Infection - Laboratory Diagnosis |format= |work= |accessdate=}}</ref><ref name="pmid26224883">{{cite journal |vauthors=Weerakoon KG, Gobert GN, Cai P, McManus DP |title=Advances in the Diagnosis of Human Schistosomiasis |journal=Clin. Microbiol. Rev. |volume=28 |issue=4 |pages=939–67 |year=2015 |pmid=26224883 |pmc=4548261 |doi=10.1128/CMR.00137-14 |url=}}</ref> | ||
*Microscopic examination of stool | *[[Microscopic examination]] of [[stool]] | ||
*Urine testing for schistosome eggs | *[[Urinalysis|Urine testing]] for schistosome eggs | ||
*Serologic testing | *[[Serological testing|Serologic testing]] | ||
*Schistosomal antigen testing (urine or serum) | *Schistosomal [[antigen]] testing ([[urine]] or [[serum]]) | ||
*Microscopic examination of tissue | *[[Microscopic examination]] of [[Tissue (biology)|tissue]] | ||
*PCR to detect schistosomal DNA | *[[PCR]] to detect schistosomal [[DNA]] | ||
===Microscopic examination of stool=== | |||
*The classic and most commonly used method for identification of schistosome eggs in [[stool]] is a modified [[Kato-Katz thick smear]].<ref name="pmid19772859">{{cite journal |vauthors=Tarafder MR, Carabin H, Joseph L, Balolong E, Olveda R, McGarvey ST |title=Estimating the sensitivity and specificity of Kato-Katz stool examination technique for detection of hookworms, Ascaris lumbricoides and Trichuris trichiura infections in humans in the absence of a 'gold standard' |journal=Int. J. Parasitol. |volume=40 |issue=4 |pages=399–404 |year=2010 |pmid=19772859 |pmc=2829363 |doi=10.1016/j.ijpara.2009.09.003 |url=}}</ref> | |||
*Testing should be done on formed [[stool]], as schistosomiasis typically does not cause [[diarrhea]]. | |||
*Several areas of a [[Stool examination|stool specimen]] should be evaluated independently, as eggs are not deposited uniformly throughout. In addition, eggs are not deposited uniformly throughout the day, and, thus, three different [[Stool examination|stool specimens]] should be evaluated. | |||
*One to 99 eggs/g is suggestive of mild infection, 100 to 299 eggs/g indicate moderate infection, and more than 300 eggs/g are indicative of high-intensity infection. | |||
*[[Kato-Katz thick smear|Kato Katz smears]] are not sufficiently [[Sensitive Skin|sensitive]] for detection of low-intensity [[infections]]. Other techniques may be superior but often are unavailable or more difficult to use. | |||
{{#ev:youtube|WpcZejHa_jM}} | |||
'''Other laboratory tests''' | |||
Other diagnostic tests that are helpful in diagnosis of schistosomiasis include: | |||
*[[Urinalysis]], including [[Dipsticks|dipstick]] testing and [[Microscope image processing|microscopic analysis]] for [[leukocytes]], [[erythrocytes]], and [[Urinary casts|casts]]. | |||
*Measurement of [[blood urea nitrogen]] ([[Blood urea nitrogen|BUN]]) and [[serum creatinine]] to test [[renal function]]. | |||
*[[Liver function tests]] | |||
*[[Complete blood count|Complete blood count (]]CBC) | |||
**[[Anemia]] | |||
**[[Eosinophilia]] | |||
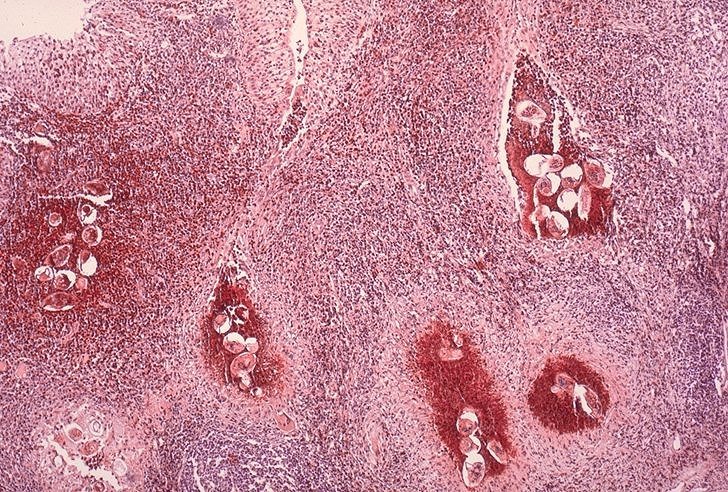
[[Image:Schistosoma bladder histopathology.jpeg|thumb|center|Photomicrography of bladder in ''S. hematobium'' infection, showing clusters of the parasite eggs with intense eosinophilia, Source: CDC]] | [[Image:Schistosoma bladder histopathology.jpeg|thumb|center|Photomicrography of bladder in ''S. hematobium'' infection, showing clusters of the parasite eggs with intense eosinophilia, Source: CDC]] | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Latest revision as of 12:46, 23 August 2017
|
Schistosomiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Schistosomiasis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Schistosomiasis laboratory findings |
|
Risk calculators and risk factors for Schistosomiasis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
Methods for diagnosing schistosomiasis include visualization of Schistosoma eggs in stool, urine, and crushed biopsy tissues. serologic assays and urinary antigen testing have also been used. Laboratory findings consistent with the diagnosis of schistosomiasis include detection of circulating antibodies to schistosomes and schistosomal antigen in serum.
Laboratory Findings
Visualization of Schistosoma eggs in stool, urine, and crushed biopsy tissues is diagnostic of schistosomiasis. Laboratory findings consistent with the diagnosis of schistosomiasis include detection of circulating antibodies to schistosomes and schistosomal antigen in serum. Diagnostic tests for schistosomiasis include the following:[1][2][3]
- Microscopic examination of stool
- Urine testing for schistosome eggs
- Serologic testing
- Schistosomal antigen testing (urine or serum)
- Microscopic examination of tissue
- PCR to detect schistosomal DNA
Microscopic examination of stool
- The classic and most commonly used method for identification of schistosome eggs in stool is a modified Kato-Katz thick smear.[4]
- Testing should be done on formed stool, as schistosomiasis typically does not cause diarrhea.
- Several areas of a stool specimen should be evaluated independently, as eggs are not deposited uniformly throughout. In addition, eggs are not deposited uniformly throughout the day, and, thus, three different stool specimens should be evaluated.
- One to 99 eggs/g is suggestive of mild infection, 100 to 299 eggs/g indicate moderate infection, and more than 300 eggs/g are indicative of high-intensity infection.
- Kato Katz smears are not sufficiently sensitive for detection of low-intensity infections. Other techniques may be superior but often are unavailable or more difficult to use.
{{#ev:youtube|WpcZejHa_jM}}
Other laboratory tests
Other diagnostic tests that are helpful in diagnosis of schistosomiasis include:
- Urinalysis, including dipstick testing and microscopic analysis for leukocytes, erythrocytes, and casts.
- Measurement of blood urea nitrogen (BUN) and serum creatinine to test renal function.
- Liver function tests
- Complete blood count (CBC)
References
- ↑ Ibironke OA, Phillips AE, Garba A, Lamine SM, Shiff C (2011). "Diagnosis of Schistosoma haematobium by detection of specific DNA fragments from filtered urine samples". Am. J. Trop. Med. Hyg. 84 (6): 998–1001. doi:10.4269/ajtmh.2011.10-0691. PMC 3110375. PMID 21633040.
- ↑ "CDC - DPDx - Schistosomiasis Infection - Laboratory Diagnosis".
- ↑ Weerakoon KG, Gobert GN, Cai P, McManus DP (2015). "Advances in the Diagnosis of Human Schistosomiasis". Clin. Microbiol. Rev. 28 (4): 939–67. doi:10.1128/CMR.00137-14. PMC 4548261. PMID 26224883.
- ↑ Tarafder MR, Carabin H, Joseph L, Balolong E, Olveda R, McGarvey ST (2010). "Estimating the sensitivity and specificity of Kato-Katz stool examination technique for detection of hookworms, Ascaris lumbricoides and Trichuris trichiura infections in humans in the absence of a 'gold standard'". Int. J. Parasitol. 40 (4): 399–404. doi:10.1016/j.ijpara.2009.09.003. PMC 2829363. PMID 19772859.