Sarilumab: Difference between revisions
No edit summary |
No edit summary |
||
| Line 229: | Line 229: | ||
|othersTitle=Others | |othersTitle=Others | ||
|useInOthers=(Description) | |useInOthers=(Description) | ||
|administration= | |administration======Subcutaneous===== | ||
*Allow to sit at room temperature for 30 minutes prior to administration or 60 minutes if using a pre-filled pen; do not warm any other way. | |||
*Rotate injection sites; do not inject where skin is tender, damaged, bruised, or scarred. | |||
*Inject full amount of pre-filled syringe or pen. | |||
*Missed dose: If 3 days or less since missed dose, take as soon as possible; take next dose at regularly scheduled time. | |||
|monitoring=*Improvement in the signs or symptoms of rheumatoid arthritis may indicate efficacy. | |||
*Neutrophils and platelets: 4 to 8 weeks after treatment initiation and approximately every 3 months thereafter. | |||
*ALT and AST levels: 4 to 8 weeks after treatment initiation and approximately every 3 months thereafter; other liver function tests if clinically indicated. | |||
*Lipid parameters: Approximately 4 to 8 weeks after treatment initiation, and at 6 month intervals thereafter. | |||
*Latent TB: Prior to initiation. | |||
*Active TB: Monitor all patients for active TB during treatment, even if initial latent TB test was negative. | |||
*Signs and symptoms of infection: During and after therapy. | |||
|overdose= | |overdose= | ||
Revision as of 12:07, 30 July 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2];
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
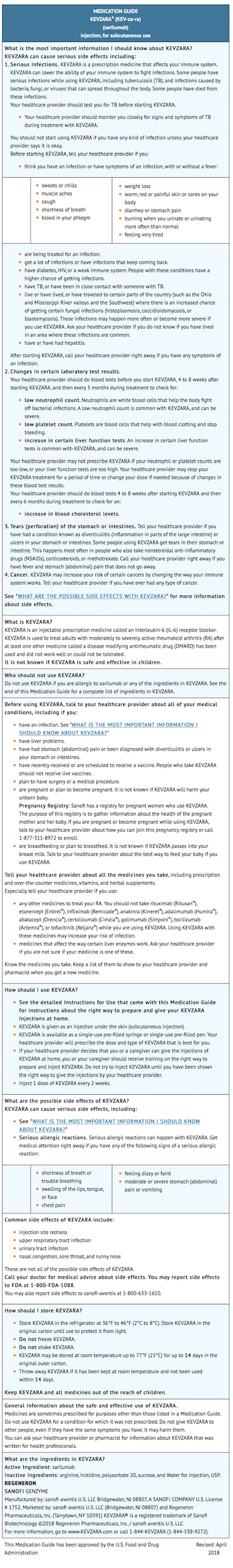
Black Box Warning
|
RISK OF SERIOUS INFECTIONS
See full prescribing information for complete Boxed Warning.
|
Overview
Sarilumab is a Acetylcholine release inhibitor, Adrenergic receptor agonist that is FDA approved for the (type of indication of drug) of a list of indications, separated by commas.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include a list of adverse reactions, separated by commas..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Contraindications
CONTRAINDICATIONS
Warnings
|
RISK OF SERIOUS INFECTIONS
See full prescribing information for complete Boxed Warning.
|
Conidition 1
(Description)
Conidition 2
(Description)
Conidition 3
(Description)
Adverse Reactions
Clinical Trials Experience
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Condition 2
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Postmarketing Experience
(Description)
Drug Interactions
- Drug 1
- Drug 2
- Drug 3
- Drug 4
- Drug 5
Drug 1
(Description)
Drug 2
(Description)
Drug 3
(Description)
Drug 4
(Description)
Drug 5
(Description)
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
(Description)
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Sarilumab in women who are pregnant.
Labor and Delivery
(Description)
Nursing Mothers
(Description)g
Pediatric Use
(Description)
Geriatic Use
(Description)
Gender
(Description)
Race
(Description)
Renal Impairment
(Description)
Hepatic Impairment
(Description)
Females of Reproductive Potential and Males
(Description)
Immunocompromised Patients
(Description)
Others
(Description)
Administration and Monitoring
Administration
Subcutaneous
- Allow to sit at room temperature for 30 minutes prior to administration or 60 minutes if using a pre-filled pen; do not warm any other way.
- Rotate injection sites; do not inject where skin is tender, damaged, bruised, or scarred.
- Inject full amount of pre-filled syringe or pen.
- Missed dose: If 3 days or less since missed dose, take as soon as possible; take next dose at regularly scheduled time.
Monitoring
- Improvement in the signs or symptoms of rheumatoid arthritis may indicate efficacy.
- Neutrophils and platelets: 4 to 8 weeks after treatment initiation and approximately every 3 months thereafter.
- ALT and AST levels: 4 to 8 weeks after treatment initiation and approximately every 3 months thereafter; other liver function tests if clinically indicated.
- Lipid parameters: Approximately 4 to 8 weeks after treatment initiation, and at 6 month intervals thereafter.
- Latent TB: Prior to initiation.
- Active TB: Monitor all patients for active TB during treatment, even if initial latent TB test was negative.
- Signs and symptoms of infection: During and after therapy.
IV Compatibility
There is limited information regarding the compatibility of Sarilumab and IV administrations.
Overdosage
There is limited information regarding Sarilumab overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Sarilumab?
| |
| Therapeutic monoclonal antibody | |
| Source | u |
| Target | IL-6R |
| Identifiers | |
| CAS number | |
| ATC code | L04 |
| PubChem | ? |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 144.13 kg/mol |
| Pharmacokinetic data | |
| Bioavailability | 80% |
| Metabolism | likely proteases |
| Half life | 21 days (steady-state, estimated) |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Subcutaneous injection |
Mechanism of Action
- Sarilumab binds to both soluble and membrane-bound IL-6 receptors (sIL-6R and mIL-6R), and has been shown to inhibit IL-6-mediated signaling through these receptors. IL-6 is a pleiotropic pro-inflammatory cytokine produced by a variety of cell types including T- and B-cells, lymphocytes, monocytes, and fibroblasts. IL-6 has been shown to be involved in diverse physiological processes such as T-cell activation, induction of immunoglobulin secretion, initiation of hepatic acute phase protein synthesis, and stimulation of hematopoietic precursor cell proliferation and differentiation. IL-6 is also produced by synovial and endothelial cells leading to local production of IL-6 in joints affected by inflammatory processes such as rheumatoid arthritis.
Structure
There is limited information regarding Sarilumab Structure in the drug label.
Pharmacodynamics
- Following single-dose subcutaneous administration of sarilumab 200-mg and 150-mg in patients with RA, rapid reduction of CRP levels was observed. Levels were reduced to normal within 2 weeks after treatment initiation. Following single-dose sarilumab administration, in patients with RA, absolute neutrophil counts decreased to the nadir between 3 to 4 days and thereafter recovered towards baseline. Treatment with sarilumab resulted in decreases in fibrinogen and serum amyloid A, and increases in hemoglobin and serum albumin.
Pharmacokinetics
Absorption
- The pharmacokinetics of sarilumab were characterized in 1770 patients with rheumatoid arthritis (RA) treated with sarilumab which included 631 patients treated with 150 mg and 682 patients treated with 200 mg doses by subcutaneous injection every two weeks for up to 52 weeks. The median tmax was observed in 2 to 4 days.
- At steady state, exposure over the dosing interval measured by area under curve (AUC) increased 2-fold with an increase in dose from 150 to 200 mg every two weeks. Steady state was reached in 14 to 16 weeks with a 2- to 3-fold accumulation compared to single dose exposure.
- For the 150 mg every two weeks dose regimen, the estimated mean (± SD) steady-state AUC, Cmin and Cmax of sarilumab were 202 ± 120 mg.day/L, 6.35 ± 7.54 mg/L, and 20.0 ± 9.20 mg/L, respectively.
- For the 200 mg every two weeks dose regimen, the estimated mean (± SD) steady-state AUC, Cmin and Cmax of sarilumab were 395 ± 207 mg.day/L, 16.5 ± 14.1 mg/L, and 35.6 ± 15.2 mg/L, respectively.
Distribution
- In patients with RA, the apparent volume of distribution at steady state was 7.3 L.
Elimination
- Sarilumab is eliminated by parallel linear and non-linear pathways. At higher concentrations, the elimination is predominantly through the linear, non-saturable proteolytic pathway, while at lower concentrations, non-linear saturable target-mediated elimination predominates. The half-life of sarilumab is concentration-dependent. At 200 mg every 2 weeks, the concentration-dependent half-life is up to 10 days in patients with RA at steady state. At 150 mg every 2 weeks, the concentration-dependent half-life is up to 8 days in patients with RA at steady state.
- After the last steady state dose of 150 mg and 200 mg sarilumab, the median times to non-detectable concentration are 28 and 43 days, respectively.
- Population pharmacokinetic analyses in patients with RA revealed that there was a trend toward higher apparent clearance of sarilumab in the presence of anti-sarilumab antibodies.
Metabolism
- The metabolic pathway of sarilumab has not been characterized. As a monoclonal antibody sarilumab is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as endogenous IgG.
Excretion
- Monoclonal antibodies, including sarilumab, are not eliminated via renal or hepatic pathways.
Specific Populations
- Population pharmacokinetic analyses in adult patients with rheumatoid arthritis showed that age, gender and race did not meaningfully influence the pharmacokinetics of sarilumab. Although body weight influenced the pharmacokinetics of sarilumab, no dose adjustments are recommended for any of these demographics.
Hepatic impairment
- No formal study of the effect of hepatic impairment on the pharmacokinetics of sarilumab was conducted.
Renal impairment
- No formal study of the effect of renal impairment on the pharmacokinetics of sarilumab was conducted. Based on population pharmacokinetic analysis of data from 1770 patients with RA, including patients with mild (creatinine clearance (CLcr): 60 to 90 mL/min; N=471 at baseline) or moderate (CLcr: 30 to 60 mL/min; N=74 at baseline) renal impairment, CLcr was correlated with sarilumab exposure. However, the effect of CLcr on exposure is not sufficient to warrant a dose adjustment. Patients with severe renal impairment were not studied.
Drug-Drug Interactions
CYP450 substrates
- Simvastatin is a CYP3A4 and OATP1B1 substrate. In 17 patients with RA, one week following a single 200-mg subcutaneous administration of sarilumab, exposure of simvastatin and simvastatin acid decreased by 45% and 36%, respectively.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- No long-term animal studies have been performed to establish the carcinogenicity potential of sarilumab. Literature indicates that the IL-6 pathway can mediate anti-tumor responses by promoting increased immune cell surveillance of the tumor microenvironment. However, available published evidence also supports that IL-6 signaling through the IL-6 receptor may be involved in pathways that lead to tumorigenesis. The malignancy risk in humans from an antibody that disrupts signaling through the IL-6 receptor, such as sarilumab, is presently unknown.
- Fertility and reproductive performance were unaffected in male and female mice treated with an analogous antibody, which binds to murine IL-6Rα to inhibit IL-6 mediated signaling, at subcutaneous doses of 10, 25, and 100 mg/kg twice per week.
Clinical Studies
Design of Clinical Studies in Adults with Moderately to Severely Active RA
- The efficacy and safety of KEVZARA were assessed in two randomized, double-blind, placebo-controlled multicenter studies (Study 1 and Study 2) in patients older than 18 years with moderately to severely active rheumatoid arthritis (RA) diagnosed according to American College of Rheumatology (ACR) criteria. Patients had at least 8 tender and 6 swollen joints at baseline.
- Study 1 evaluated 1197 patients with moderately to severely active rheumatoid arthritis who had inadequate clinical response to methotrexate (MTX). Patients received subcutaneous KEVZARA 200 mg, KEVZARA 150 mg, or placebo every two weeks with concomitant MTX. After Week 16 in Study 1, patients with an inadequate response could have been rescued with KEVZARA 200 mg every two weeks.
- Study 2 evaluated 546 patients with moderately to severely active rheumatoid arthritis who had an inadequate clinical response or were intolerant to one or more TNF-α antagonists. Patients received subcutaneous KEVZARA 200 mg, KEVZARA 150 mg, or placebo every two weeks with concomitant conventional DMARDs (MTX, sulfasalazine, leflunomide, and/or hydroxychloroquine). After Week 12 in Study 2, patients with an inadequate response could have been rescued with KEVZARA 200 mg every two weeks.
- In Studies 1 and 2, the primary endpoint was the proportion of patients who achieved an ACR20 response at Week 24. Other key endpoints evaluated included change from baseline in HAQ-DI at Week 16 in Study 1 and at Week 12 in Study 2, and change from baseline in van der Heijde-modified Total Sharp Score (mTSS) at Week 52 in Study 1.
Clinical Response
- The percentages of KEVZARA every two weeks + MTX/DMARD-treated patients achieving ACR20, ACR50 and ACR70 responses in Studies 1 and 2 are shown Table 4. In both studies, patients treated with either 200 mg or 150 mg of KEVZARA every two weeks + MTX/DMARD had higher ACR20, ACR50, and ACR70 response rates versus placebo + MTX/DMARD-treated patients at Week 24.
- In Studies 1 and 2, a greater proportion of patients treated with KEVZARA 200 mg or 150 mg every two weeks plus MTX/DMARD achieved a low level of disease activity as measured by a Disease Activity Score 28-C-Reactive Protein (DAS28-CRP) <2.6 compared with placebo + MTX/DMARD at the end of the studies (Table 4). In Study 1, the proportion of patients achieving DAS28-CRP <2.6 who had at least 3 or more active joints at the end of Week 24 was 33.1%, 37.8% and 20%, in the KEVZARA 200 mg + MTX/DMARD arm, KEVZARA 150 mg + MTX/DMARD arm, and placebo arm respectively.

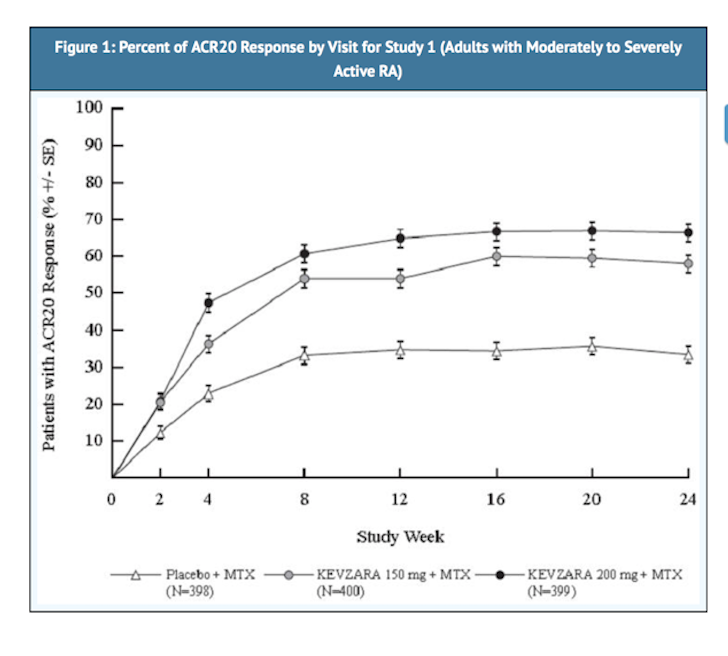
- The percent ACR20 response by visit in Study 1 is shown in Figure 1. A similar response curve was observed in Study 2.
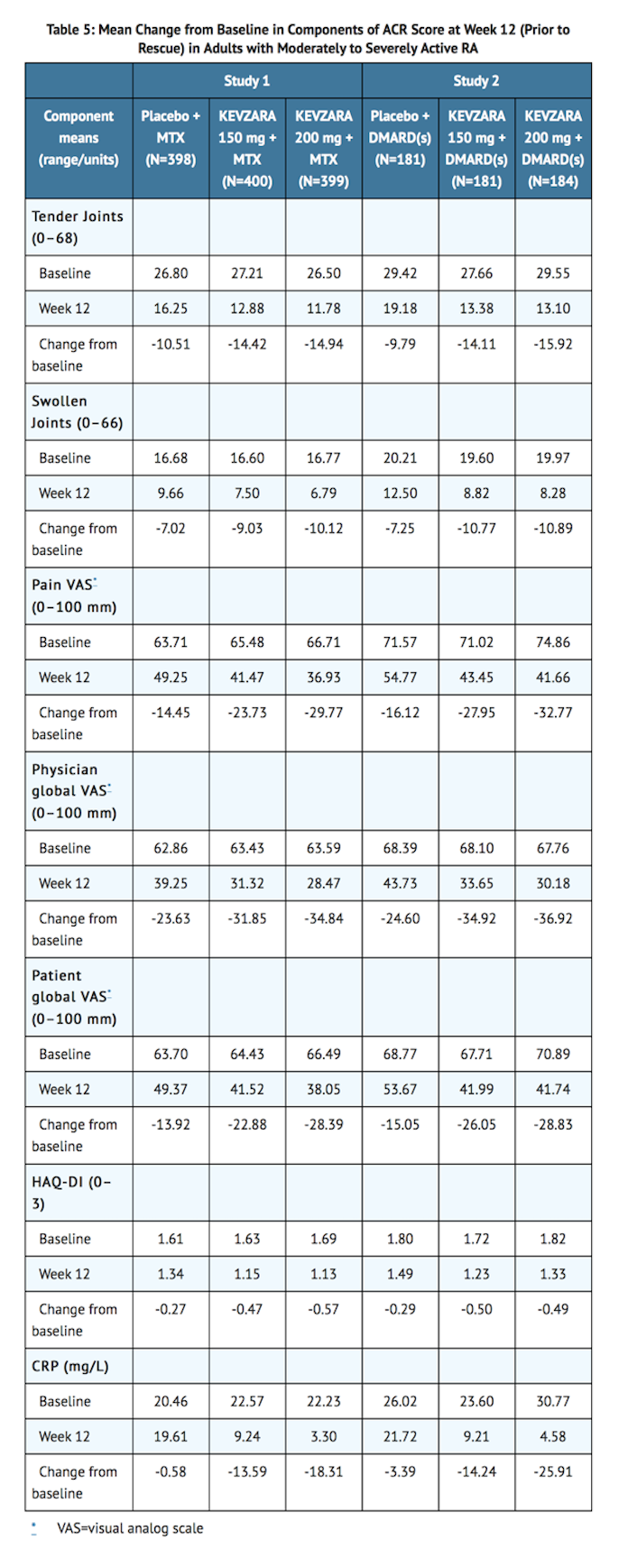
- The results of the components of the ACR response criteria at Week 12 for Studies 1 and 2 are shown in Table 5.
Radiographic Response
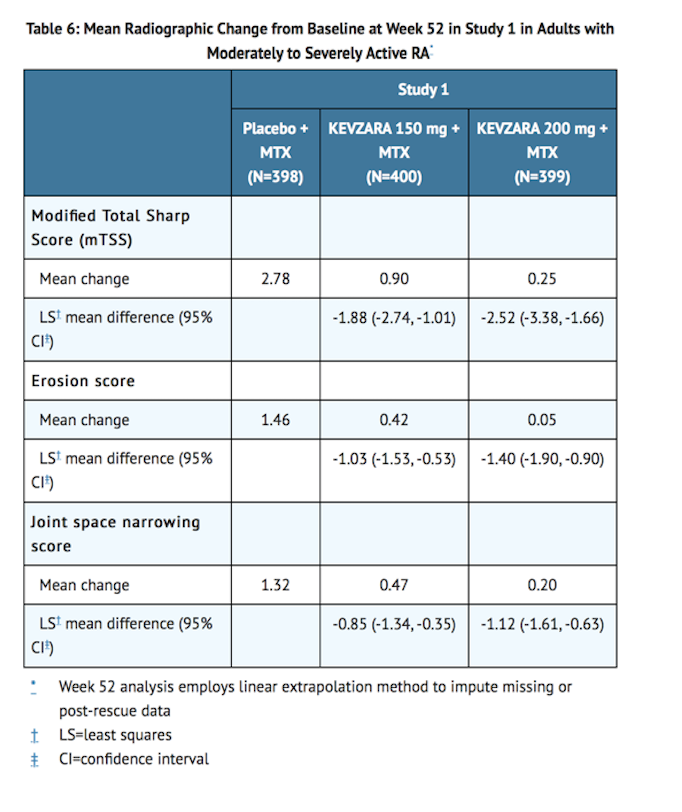
- In Study 1, structural joint damage was assessed radiographically and expressed as the van der Heijde-modified Total Sharp Score (mTSS) and its components, the erosion score and joint space narrowing score. Radiographs of hands and feet were obtained at baseline, 24 weeks, and 52 weeks and scored independently by at least two well-trained readers who were blinded to treatment group and visit number.
- Both doses of KEVZARA + MTX were superior to placebo + MTX in the change from baseline in mTSS over 52 weeks. Less progression of both erosion and joint space narrowing scores over 52 weeks was reported in the KEVZARA + MTX treatment groups compared to the placebo + MTX group.
- Treatment with KEVZARA + MTX was associated with significantly less radiographic progression of structural damage as compared with placebo + MTX. At Week 52, 55.6% of patients receiving KEVZARA 200 mg + MTX and 47.8% of patients receiving KEVZARA 150 mg + MTX had no progression of structural damage (as defined by a change in the Total Sharp Score of zero or less) compared with 38.7% of patients receiving placebo.
Physical Function Response
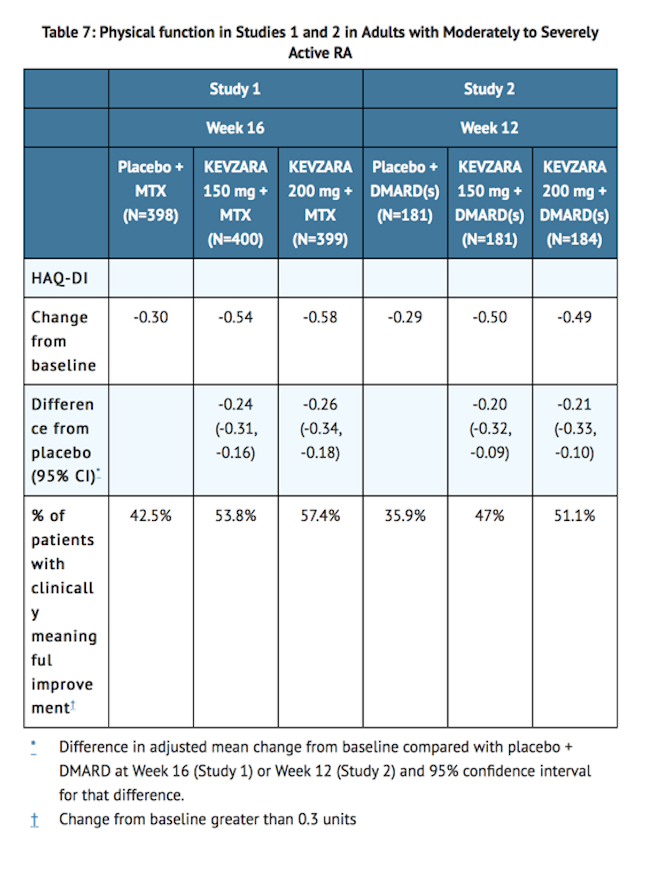
- In Studies 1 and 2, physical function and disability were assessed by the Health Assessment Questionnaire Disability Index (HAQ-DI). Patients receiving KEVZARA 200 mg every two weeks + MTX/DMARD and KEVZARA 150 mg every two weeks + MTX/DMARD demonstrated greater improvement from baseline in physical function compared to placebo + MTX/DMARD at Week 16 and Week 12 in Studies 1 and 2, respectively (Table 7).
Other Health Related Outcomes
- General health status was assessed by the Short Form health survey (SF-36) in Studies 1 and 2. Patients receiving KEVZARA 200 mg every two weeks + MTX/DMARD demonstrated greater improvement from baseline compared to placebo + MTX/DMARD in the physical component summary (PCS) at Week 24, but there was no evidence of a difference between the treatment groups in the mental component summary (MCS) at Week 24. Patients receiving KEVZARA 200 mg + MTX/DMARD reported greater improvement relative to placebo in the domains of Physical Functioning, Role Physical, Bodily Pain, General Health Perception, Vitality, Social Functioning and Mental Health, but not in the Role Emotional domain.
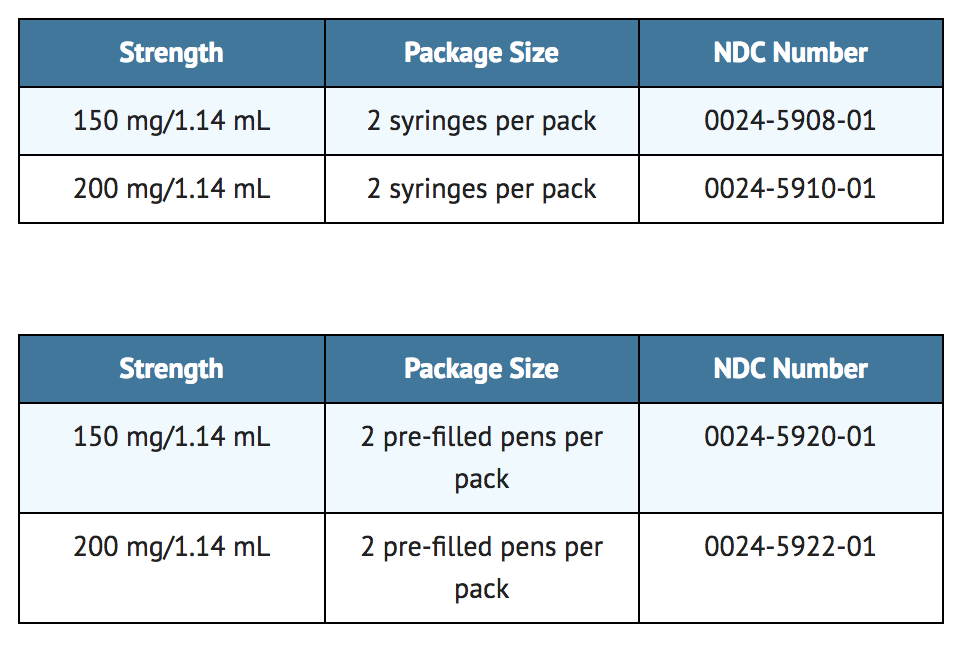
How Supplied
- KEVZARA (sarilumab) injection is supplied as a colorless to pale yellow solution in a single-dose pre-filled syringes and single-dose pre-filled pens.
Storage
- Refrigerate at 36°F to 46°F (2°C to 8°C) in original carton to protect from light. Do not freeze. Do not shake.
- If needed, patients/caregivers may store KEVZARA at room temperature up to 77°F (25°C) up to 14 days in the outer carton. Do not store above 77°F (25°C). After removal from the refrigerator, use KEVZARA within 14 days or discard.
Images
Drug Images
{{#ask: Page Name::Sarilumab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel


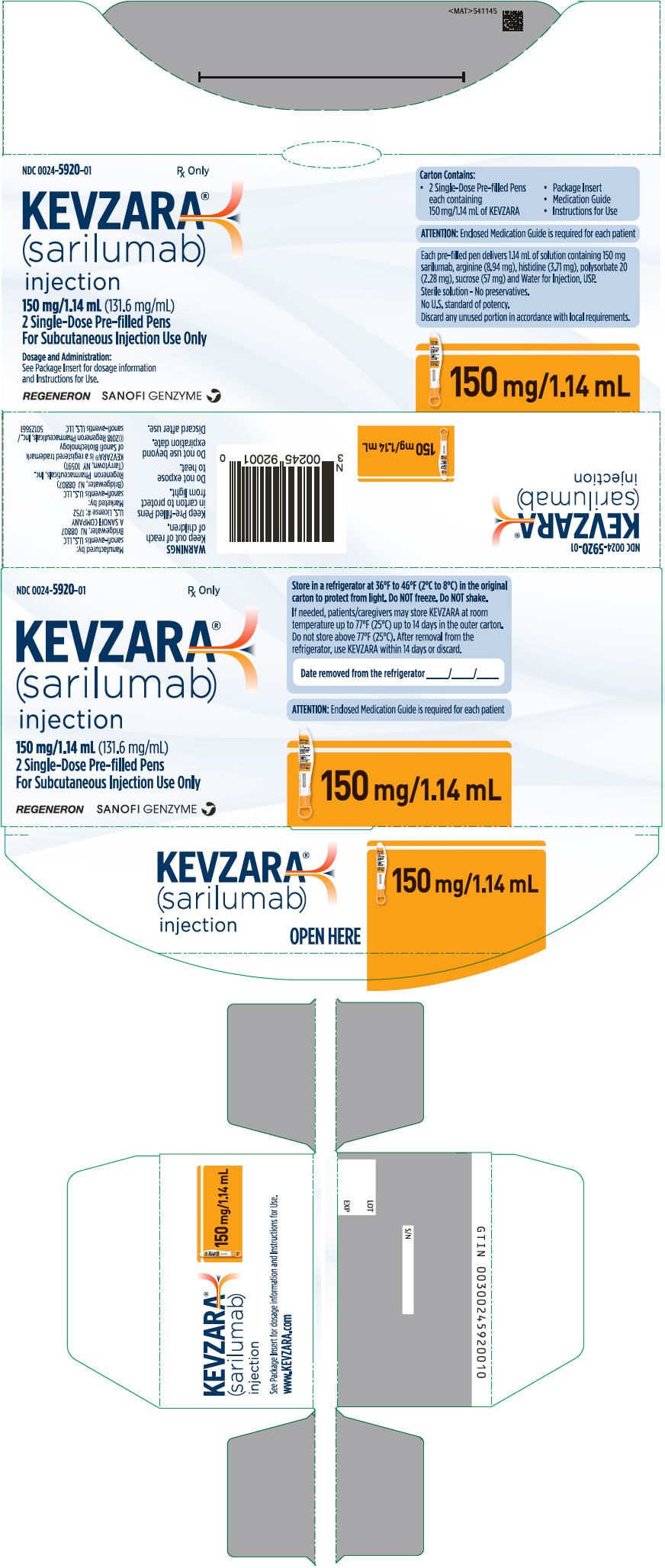
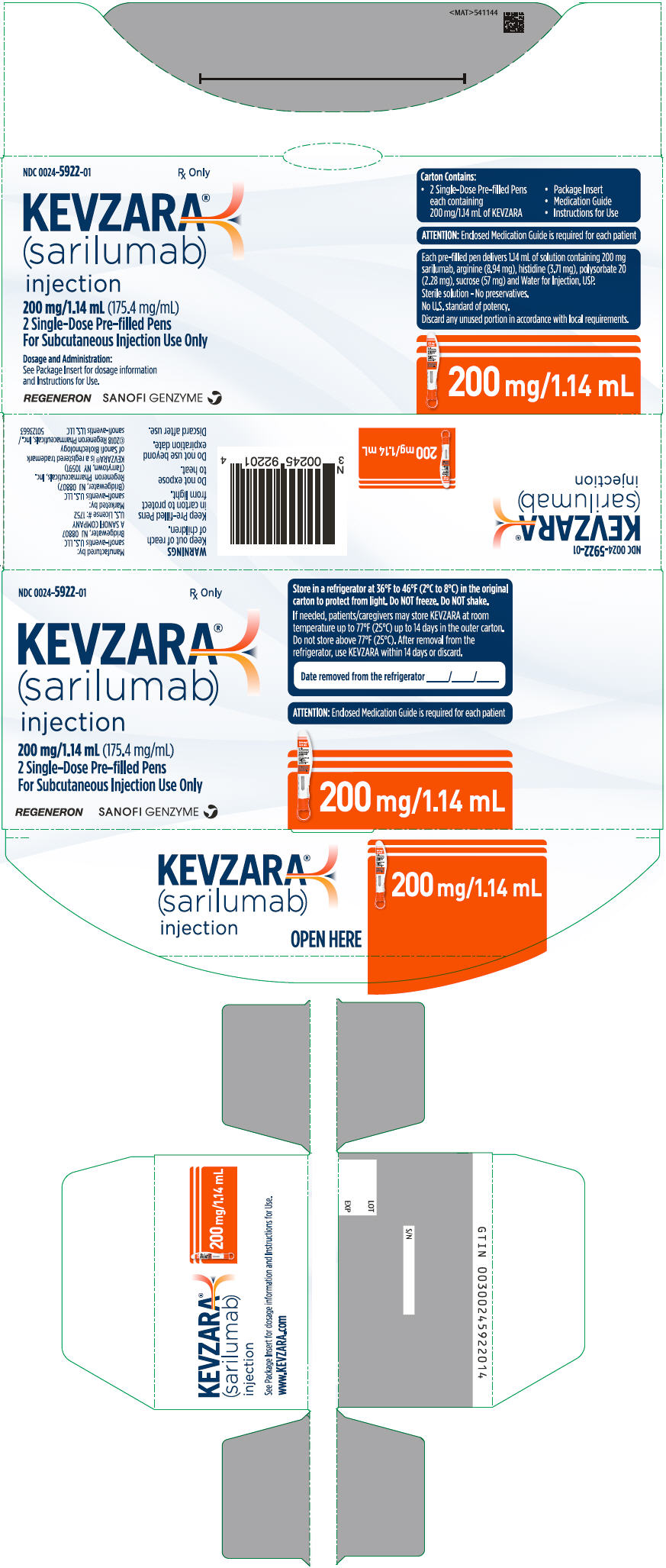
{{#ask: Label Page::Sarilumab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Infections
- Inform patients that KEVZARA may lower their resistance to infections. Instruct patients to contact their physician immediately when symptoms suggesting infection appear, to ensure rapid evaluation and appropriate treatment.
Gastrointestinal Perforation
- Inform patients that some patients, particularly those also taking NSAIDS, and/or steroids, have had tears (perforations) of the stomach or intestines. Inform patients that gastrointestinal perforations have been reported in KEVZARA-treated patients in clinical studies, primarily as a complication of diverticulitis. Instruct patients to contact their physician immediately when symptoms of severe, persistent abdominal pain appear to ensure rapid evaluation and appropriate treatment.
Hypersensitivity and Serious Allergic Reaction
- Assess patient suitability for home use for SC injection. Inform patients that some patients who have been treated with KEVZARA have developed serious allergic reactions. Advise patients to seek immediate medical attention if they experience any symptom of serious allergic reactions.
Pregnancy Registry
- There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to KEVZARA during pregnancy. Encourage participation in the registry.
Instruction on Injection Technique
- Instruct patients and caregivers to read the Instructions for Use before the patient starts using KEVZARA, and each time the patient gets a refill as there may be new information they need to know.
- Provide guidance to patients and caregivers on proper subcutaneous injection technique, including aseptic technique, and how to use the pre-filled syringe or pre-filled pen correctly.
- The pre-filled syringe or pre-filled pen should be left at room temperature for 30 minutes or 60 minutes respectively prior to use. The syringe or pen should be used within 14 days after being taken out of the refrigerator. A puncture-resistant container should be used to dispose the used pre-filled syringes or pre-filled pens and should be kept out of the reach of children. Instruct patients or caregivers in the technique as well as proper pre-filled syringe or pre-filled pen disposal, and caution against reuse of these items.
Precautions with Alcohol
Alcohol-Sarilumab interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Kevzara
Look-Alike Drug Names
There is limited information regarding Sarilumab Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.