Sandbox Enoxaparin
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: SPINAL/EPIDURAL HEMATOMA
See full prescribing information for complete Boxed Warning.
Epidural or spinal hematomas may occur in patients who are anticoagulated with low molecular weight heparins (LMWH) or heparinoids and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include:
|
Overview
Sandbox Enoxaparin is {{{aOrAn}}} Low molecular weight heparin that is FDA approved for the {{{indicationType}}} of Treatment of acute deep vein thrombosis,acute ST-segment elevation myocardial infarction and prophylaxis of deep vein thrombosis, ischemic complications of unstable angina and Non-Q-Wave myocardial infarction. There is a Black Box Warning for this drug as shown here. Common adverse reactions include Diarrhea, Nausea,Anemia, Bleeding, Major , Thrombocytopenia,Increased liver function test Fever.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
<h4>Condition 1</h4>
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Sandbox Enoxaparin FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Contraindications
- Active major bleeding
- Thrombocytopenia associated with a positive in vitro test for anti-platelet antibody in the presence of enoxaparin sodium
- Known hypersensitivity to enoxaparin sodium (e.g., pruritus, urticaria, anaphylactic/anaphylactoid reactions) [see Adverse Reactions (6.2)]
- Known hypersensitivity to heparin or pork products
- Known hypersensitivity to benzyl alcohol (which is in only the multi-dose formulation of Lovenox)
Warnings
|
WARNING: SPINAL/EPIDURAL HEMATOMA
See full prescribing information for complete Boxed Warning.
Epidural or spinal hematomas may occur in patients who are anticoagulated with low molecular weight heparins (LMWH) or heparinoids and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include:
|
Cases of epidural or spinal hemorrhage and subsequent hematomas have been reported with the use of Lovenox and epidural or spinal anesthesia/analgesia or spinal puncture procedures, resulting in long-term or permanent paralysis. The risk of these events is higher with the use of post-operative indwelling epidural catheters, with the concomitant use of additional drugs affecting hemostasis such as NSAIDs, with traumatic or repeated epidural or spinal puncture, or in patients with a history of spinal surgery or spinal deformity [see Boxed Warning, Adverse Reactions (6.2) and Drug Interactions (7)].
Adverse Reactions
Clinical Trials Experience
Clinical Trials Experience
The following serious adverse reactions are also discussed in other sections of the labeling:
- *Spinal/epidural hematoma [see Boxed Warning and Warnings and Precautions (5.1)]
- *Increased Risk of Hemorrhage [see Warnings and Precautions (5.1)]
- *Thrombocytopenia [see Warnings and Precautions (5.5)]
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
During clinical development for the approved indications, 15,918 patients were exposed to enoxaparin sodium. These included 1,228 for prophylaxis of deep vein thrombosisfollowing abdominal surgery in patients at risk for thromboembolic complications, 1,368 for prophylaxis of deep vein thrombosisfollowing hip or knee replacement surgery, 711 for prophylaxis of deep vein thrombosisin medical patients with severely restricted mobility during acute illness, 1,578 for prophylaxis of ischemic complications in unstable angina and non-Q-wave myocardial infarction, 10,176 for treatment of acute ST-elevation myocardial infarction, and 857 for treatment of deep vein thrombosiswith or without pulmonary embolism. Enoxaparin sodium doses in the clinical trials for prophylaxis of deep vein thrombosisfollowing abdominal or hip or knee replacement surgery or in medical patients with severely restricted mobility during acute illness ranged from 40 mg SC once daily to 30 mg SC twice daily. In the clinical studies for prophylaxis of ischemic complications of unstable angina and non-Q-wave myocardial infarction doses were 1 mg/kg every 12 hours and in the clinical studies for treatment of acute ST-segment elevation myocardial infarction enoxaparin sodium doses were a 30 mg IV bolus followed by 1 mg/kg every 12 hours SC.
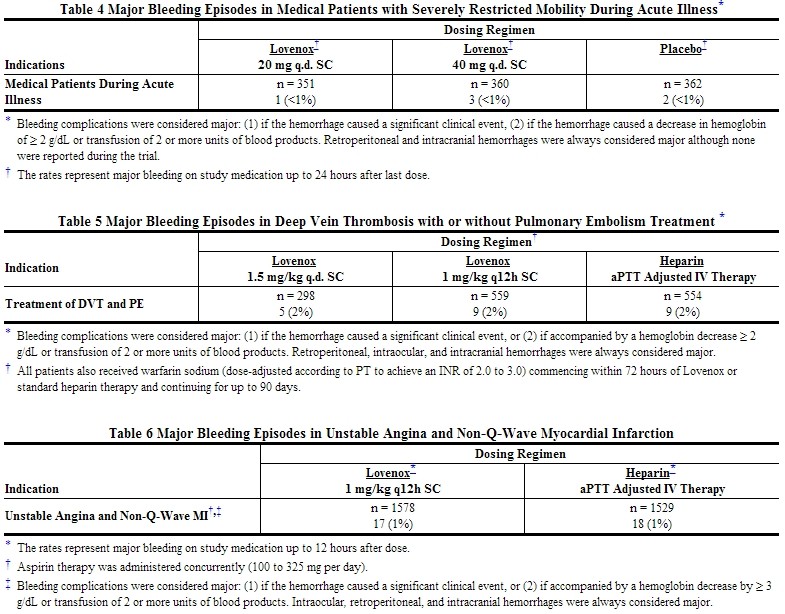
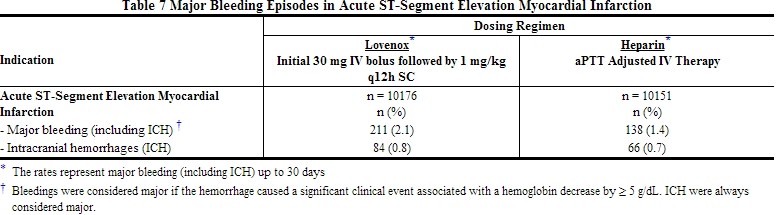
Hemorrhage
The incidence of major hemorrhagic complications during Lovenox treatment has been low.
The following rates of major bleeding events have been reported during clinical trials with Lovenox [see Tables 2 to 7].
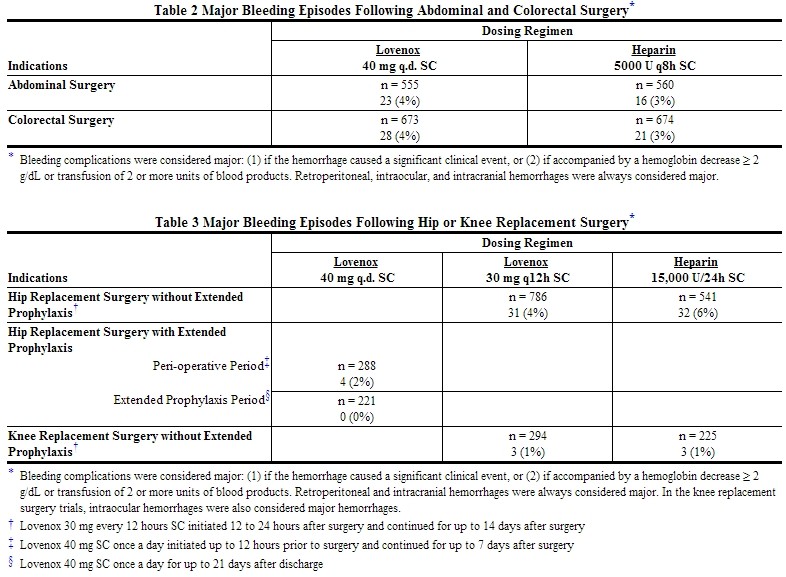
NOTE: At no time point were the 40 mg once a day pre-operative and the 30 mg every 12 hours post-operative hip replacement surgery prophylactic regimens compared in clinical trials.
Injection site hematomas during the extended prophylaxis period after hip replacement surgery occurred in 9% of the Lovenox patients versus 1.8% of the placebo patients.
Elevations of Serum Aminotransferases
Asymptomatic increases in aspartate (AST [SGOT]) and alanine (ALT [SGPT]) aminotransferase levels greater than three times the upper limit of normal of the laboratory reference range have been reported in up to 6.1% and 5.9% of patients, respectively, during treatment with Lovenox. Similar significant increases in aminotransferase levels have also been observed in patients and healthy volunteers treated with heparin and other low molecular weight heparins. Such elevations are fully reversible and are rarely associated with increases in bilirubin.
Since aminotransferase determinations are important in the differential diagnosis of myocardial infarction, liver disease, and pulmonary emboli, elevations that might be caused by drugs like Lovenox should be interpreted with caution.
Local Reactions
Mild local irritation, pain, hematoma, ecchymosis, and erythema may follow SC injection of Lovenox.
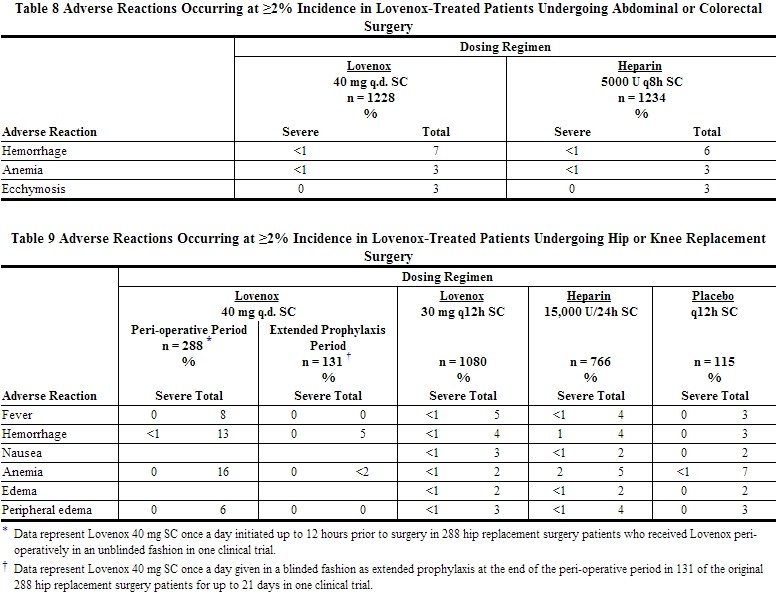
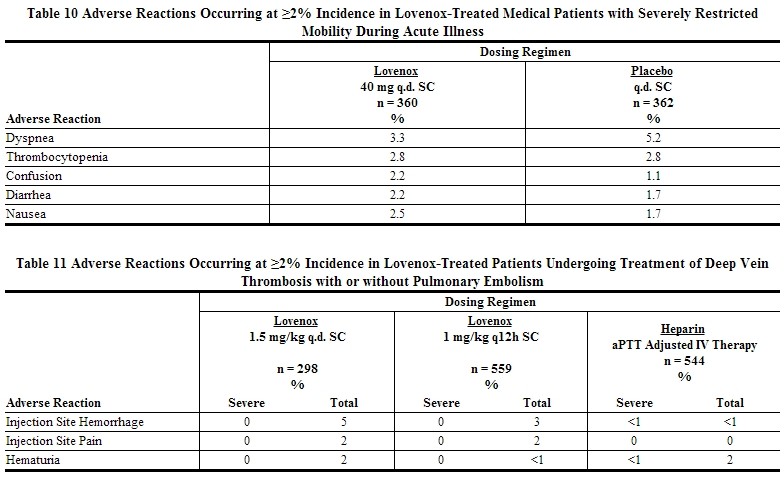
Adverse Reactions in Patients Receiving Lovenox for Prophylaxis or Treatment of DVT, PE
Other adverse reactions that were thought to be possibly or probably related to treatment with Lovenox, heparin, or placebo in clinical trials with patients undergoing hip or knee replacement surgery, abdominal or colorectal surgery, or treatment for DVT and that occurred at a rate of at least 2% in the Lovenox group, are provided below [see Tables 8 to 11].
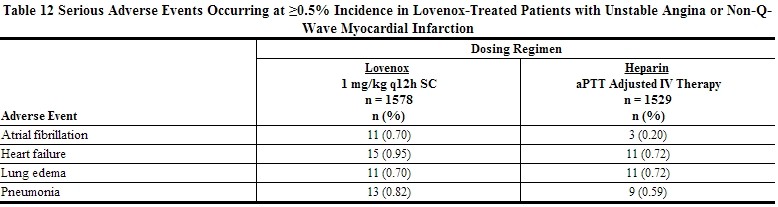
Adverse Events in Lovenox-Treated Patients with unstable angina or Non-Q-Wave myocardial infarction
Non-hemorrhagic clinical events reported to be related to Lovenox therapy occurred at an incidence of ≤1%.
Non-major hemorrhagic events, primarily injection site ecchymoses and hematomas, were more frequently reported in patients treated with SC Lovenox than in patients treated with IV heparin.
Serious adverse events with Lovenox or heparin in a clinical trial in patients with unstable angina or non-Q-wave myocardial infarction that occurred at a rate of at least 0.5% in the Lovenox group are provided below [see Table 12].
Adverse Reactions in Lovenox-Treated Patients with Acute ST-Segment Elevation myocardial infarction
In a clinical trial in patients with acute ST-segment elevation myocardial infarction, the only adverse reaction that occurred at a rate of at least 0.5% in the Lovenox group was thrombocytopenia (1.5%).
Postmarketing Experience
The following adverse reactions have been identified during postapproval use of Lovenox. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
There have been reports of epidural or spinal hematoma formation with concurrent use of Lovenox and spinal/epidural anesthesia or spinal puncture. The majority of patients had a post-operative indwelling epidural catheter placed for analgesia or received additional drugs affecting hemostasis such as NSAIDs. Many of the epidural or spinal hematomas caused neurologic injury, including long-term or permanent paralysis.
Local reactions at the injection site (e.g. nodules, inflammation, oozing), systemic allergic reactions (e.g. pruritus, urticaria, anaphylactic/anaphylactoid reactions including shock), vesiculobullous rash, rare cases of hypersensitivity cutaneous vasculitis, purpura, skin necrosis (occurring at either the injection site or distant from the injection site), thrombocytosis, and thrombocytopenia with thrombosis [see Warnings and Precautions (5.5)] have been reported.
Cases of hyperkalemia have been reported. Most of these reports occurred in patients who also had conditions that tend toward the development of hyperkalemia (e.g., renal dysfunction, concomitant potassium-sparing drugs, administration of potassium, hematoma in body tissues). Very rare cases of hyperlipidemia have also been reported, with one case of hyperlipidemia, with marked hypertriglyceridemia, reported in a diabetic pregnant woman; causality has not been determined.
Cases of headache, hemorrhagic anemia, eosinophilia, alopecia, hepatocellular and cholestatic liver injury have been reported.
Osteoporosis has also been reported following long-term therapy.
Drug Interactions
Whenever possible, agents which may enhance the risk of hemorrhage should be discontinued prior to initiation of Lovenox therapy. These agents include medications such as: anticoagulants, platelet inhibitors including acetylsalicylic acid, salicylates, NSAIDs (including ketorolac tromethamine), dipyridamole, or sulfinpyrazone. If co-administration is essential, conduct close clinical and laboratory monitoring
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
All pregnancies have a background risk of birth defect, loss, or other adverse outcome regardless of drug exposure. The fetal risk summary below describes the potential of Lovenox to increase the risk of developmental abnormalities above the background risk.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Sandbox Enoxaparin in women who are pregnant.
Labor and Delivery
Lovenox does not cross the placenta, and is not expected to result in fetal exposure to the drug. Human data from a retrospective cohort study, which included 693 live births, suggest that Lovenox does not increase the risk of major developmental abnormalities. Based on animal data, enoxaparin is not predicted to increase the risk of major developmental abnormalities
Nursing Mothers
It is not known whether Lovenox is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Lovenox, a decision should be made whether to discontinue nursing or discontinue Lovenox, taking into account the importance of Lovenox to the mother and the known benefits of nursing.
Pediatric Use
Safety and effectiveness of Lovenox in pediatric patients have not been established.
Geriatic Use
Prevention of Deep Vein Thrombosis in Hip, Knee and Abdominal Surgery; Treatment of Deep Vein Thrombosis, Prevention of Ischemic Complications of Unstable Angina and Non-Q-wave Myocardial Infarction
Over 2800 patients, 65 years and older, have received Lovenox in pivotal clinical trials. The efficacy of Lovenox in the geriatric (≥65 years) was similar to that seen in younger patients (<65 years). The incidence of bleeding complications was similar between geriatric and younger patients when 30 mg every 12 hours or 40 mg once a day doses of Lovenox were employed. The incidence of bleeding complications was higher in geriatric patients as compared to younger patients when Lovenox was administered at doses of 1.5 mg/kg once a day or 1 mg/kg every 12 hours. The risk of Lovenox-associated bleeding increased with age. Serious adverse events increased with age for patients receiving Lovenox. Other clinical experience (including postmarketing surveillance and literature reports) has not revealed additional differences in the safety of Lovenox between geriatric and younger patients. Careful attention to dosing intervals and concomitant medications (especially antiplatelet medications) is advised. Lovenox should be used with care in geriatric patients who may show delayed elimination of enoxaparin. Monitoring of geriatric patients with low body weight (<45 kg) and those predisposed to decreased renal function should be considered [see Warnings and Precautions (5.9) and Clinical Pharmacology (12.3)].
Treatment of Acute ST-Segment Elevation Myocardial Infarction
In the clinical study for treatment of acute ST-segment elevation myocardial infarction, there was no evidence of difference in efficacy between patients ≥75 years of age (n = 1241) and patients less than 75 years of age (n=9015). Patients ≥75 years of age did not receive a 30 mg IV bolus prior to the normal dosage regimen and had their SC dose adjusted to 0.75 mg/kg every 12 hours [see Dosage and Administration (2.3)]. The incidence of bleeding complications was higher in patients ≥65 years of age as compared to younger patients (<65 years).
Gender
There is no FDA guidance on the use of Sandbox Enoxaparin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Sandbox Enoxaparin with respect to specific racial populations.
Renal Impairment
In patients with renal impairment, there is an increase in exposure of enoxaparin sodium. All such patients should be observed carefully for signs and symptoms of bleeding. Because exposure of enoxaparin sodium is significantly increased in patients with severe renal impairment (creatinine clearance <30 mL/min), a dosage adjustment is recommended for therapeutic and prophylactic dosage ranges. No dosage adjustment is recommended in patients with moderate (creatinine clearance 30–50 mL/min) and mild (creatinine clearance 50–80 mL/min) renal impairment [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)]. In patients with renal failure, treatment with enoxaparin has been associated with the development of hyperkalemia [see Adverse Reactions (6.2)].
Hepatic Impairment
The impact of hepatic impairment on enoxaparin's exposure and antithrombotic effect has not been investigated. Caution should be exercised when administering enoxaparin to patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Sandbox Enoxaparin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Sandbox Enoxaparin in patients who are immunocompromised.
Low-Weight Patients
An increase in exposure of enoxaparin sodium with prophylactic dosages (non-weight adjusted) has been observed in low-weight women (<45 kg) and low-weight men (<57 kg). All such patients should be observed carefully for signs and symptoms of bleeding [see Clinical Pharmacology (12.3)].
Administration and Monitoring
Administration
Lovenox is a clear, colorless to pale yellow sterile solution, and as with other parenteral drug products, should be inspected visually for particulate matter and discoloration prior to administration.
The use of a tuberculin syringe or equivalent is recommended when using Lovenox multiple-dose vials to assure withdrawal of the appropriate volume of drug.
Lovenox must not be administered by intramuscular injection. Lovenox is intended for use under the guidance of a physician.
For subcutaneous administration, patients may self-inject only if their physicians determine that it is appropriate and with medical follow-up, as necessary. Proper training in subcutaneous injection technique (with or without the assistance of an injection device) should be provided.
Subcutaneous Injection Technique: Patients should be lying down and Lovenox administered by deep SC injection. To avoid the loss of drug when using the 30 and 40 mg prefilled syringes, do not expel the air bubble from the syringe before the injection. Administration should be alternated between the left and right anterolateral and left and right posterolateral abdominal wall. The whole length of the needle should be introduced into a skin fold held between the thumb and forefinger; the skin fold should be held throughout the injection. To minimize bruising, do not rub the injection site after completion of the injection.
Lovenox prefilled syringes and graduated prefilled syringes are for single, one-time use only and are available with a system that shields the needle after injection.
Remove the prefilled syringe from the blister packaging by peeling at the arrow as directed on the blister. Do not remove by pulling on the plunger as this may damage the syringe.
1.Remove the needle shield by pulling it straight off the syringe (see Figure A). If adjusting the dose is required, the dose adjustment must be done prior to injecting the prescribed dose to the patient.
Figure A
{
Monitoring
- All patients should be evaluated for a bleeding disorder before administration of Enoxaparin Sodium Injection, unless the medication is needed urgently. Since coagulation parameters are unsuitable for monitoring Enoxaparin Sodium Injection activity, routine monitoring of coagulation parameters is not required
- Thrombocytopenia of any degree should be monitored closely. If the platelet count falls below 100,000/mm3, enoxaparin sodium injection should be discontinued. Cases of heparin-induced thrombocytopenia with thrombosis have also been observed in clinical practice. Some of these cases were complicated by organ infarction, limb ischemia, or death
- Women with mechanical prosthetic heart valves may be at higher risk for thromboembolism during pregnancy, and, when pregnant, have a higher rate of fetal loss from stillbirth, spontaneous abortion and premature delivery. Therefore, frequent monitoring of peak and trough anti-Factor Xa levels, and adjusting of dosage may be needed
- Anti-Factor Xa may be used to monitor the anticoagulant effect of enoxaparin sodium injection in patients with significant renal impairment. If during enoxaparin sodium injection therapy abnormal coagulation parameters or bleeding should occur, anti-Factor Xa levels may be used to monitor the anticoagulant effects of enoxaparin sodium injection
- Whenever possible, agents which may enhance the risk of hemorrhage should be discontinued prior to initiation of enoxaparin sodium injection therapy. These agents include medications such as: anticoagulants, platelet inhibitors including acetylsalicylic acid, salicylates, NSAIDs (including ketorolac tromethamine), dipyridamole, or sulfinpyrazone. If co-administration is essential, conduct close clinical and laboratory monitoring
- Monitoring of geriatric patients with low body weight (<45 kg) and those predisposed to decreased renal function should be considered
IV Compatibility
There is limited information regarding the compatibility of Sandbox Enoxaparin and IV administrations.
Overdosage
Accidental overdosage following administration of Lovenox may lead to hemorrhagic complications. Injected Lovenox may be largely neutralized by the slow IV injection of protamine sulfate (1%
solution). The dose of protamine sulfate should be equal to the dose of Lovenox injected: 1 mg protamine sulfate should be administered to neutralize 1 mg Lovenox, if enoxaparin sodium was administered in the previous 8 hours. An infusion of 0.5 mg protamine per 1 mg of enoxaparin sodium may be administered if enoxaparin sodium was administered greater than 8 hours previous to the protamine administration, or if it has been determined that a second dose of protamine is required. The second infusion of 0.5 mg protamine sulfate per 1 mg of Lovenox may be administered if the aPTT measured 2 to 4 hours after the first infusion remains prolonged.
If at least 12 hours have elapsed since the last enoxaparin sodium injection, protamine administration may not be required; however, even with higher doses of protamine, the aPTT may remain more prolonged than following administration of heparin. In all cases, the anti-Factor Xa activity is never completely neutralized (maximum about 60%). Particular care should be taken to avoid overdosage with protamine sulfate. Administration of protamine sulfate can cause severe hypotensive and anaphylactoid reactions. Because fatal reactions, often resembling anaphylaxis, have been reported with protamine sulfate, it should be given only when resuscitation techniques and treatment of anaphylactic shock are readily available. For additional information consult the labeling of protamine sulfate injection products.
Pharmacology
| Template:Px | |
| Template:Px | |
Sandbox Enoxaparin
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | |
| ATC code | B01 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | (C26H40N2O36S5)n |
| Mol. mass | 4500 daltons (average) |
| Pharmacokinetic data | |
| Bioavailability | 92% |
| Protein binding | 80% bound-albumin |
| Metabolism | primarily by kidneys |
| Half life | 4.5 hours |
| Excretion | ? |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. |
B |
| Legal status |
POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | Subcutaneous (SC) Injection and intravenous (IV) per package insert |
Mechanism of Action
There is limited information regarding Sandbox Enoxaparin Mechanism of Action in the drug label.
Structure
Lovenox is a sterile aqueous solution containing enoxaparin sodium, a low molecular weight heparin. The pH of the injection is 5.5 to 7.5. Enoxaparin sodium is obtained by alkaline depolymerization of heparin benzyl ester derived from porcine intestinal mucosa. Its structure is characterized by a 2-O-sulfo-4-enepyranosuronic acid group at the non-reducing end and a 2-N,6-O-disulfo-D-glucosamine at the reducing end of the chain. About 20% (ranging between 15% and 25%) of the enoxaparin structure contains an 1,6 anhydro derivative on the reducing end of the polysaccharide chain. The drug substance is the sodium salt. The average molecular weight is about 4500 daltons. The molecular weight distribution is:
<2000 daltons ≤20%
2000 to 8000 daltons ≥68%
>8000 daltons ≤18%
STRUCTURAL FORMULA
{
Pharmacodynamics
In humans, enoxaparin given at a dose of 1.5 mg/kg subcutaneously (SC) is characterized by a higher ratio of anti-Factor Xa to anti-Factor IIa activity (mean ± SD, 14.0 ± 3.1) (based on areas under anti-Factor activity versus time curves) compared to the ratios observed for heparin (mean±SD, 1.22 ± 0.13). Increases of up to 1.8 times the control values were seen in the thrombin time (TT) and the activated partial thromboplastin time (aPTT). Enoxaparin at a 1 mg/kg dose (100 mg/mL concentration), administered SC every 12 hours to patients in a large clinical trial resulted in aPTT values of 45 seconds or less in the majority of patients (n = 1607). A 30 mg IV bolus immediately followed by a 1 mg/kg SC administration resulted in aPTT post-injection values of 50 seconds. The average aPTT prolongation value on Day 1 was about 16% higher than on Day 4.
Pharmacokinetics
Absorption: Pharmacokinetic trials were conducted using the 100 mg/mL formulation. Maximum anti-Factor Xa and anti-thrombin (anti-Factor IIa) activities occur 3 to 5 hours after SC injection of enoxaparin. Mean peak anti-Factor Xa activity was 0.16 IU/mL (1.58 mcg/mL) and 0.38 IU/mL (3.83 mcg/mL) after the 20 mg and the 40 mg clinically tested SC doses, respectively. Mean (n = 46) peak anti-Factor Xa activity was 1.1 IU/mL at steady state in patients with unstable angina receiving 1 mg/kg SC every 12 hours for 14 days. Mean absolute bioavailability of enoxaparin, after 1.5 mg/kg given SC, based on anti-Factor Xa activity is approximately 100% in healthy subjects.
A 30 mg IV bolus immediately followed by a 1 mg/kg SC every 12 hours provided initial peak anti-Factor Xa levels of 1.16 IU/mL (n=16) and average exposure corresponding to 84% of steady-state levels. Steady state is achieved on the second day of treatment.
Enoxaparin pharmacokinetics appear to be linear over the recommended dosage ranges [see Dosage and Administration (2)]. After repeated subcutaneous administration of 40 mg once daily and 1.5 mg/kg once-daily regimens in healthy volunteers, the steady state is reached on day 2 with an average exposure ratio about 15% higher than after a single dose. Steady-state enoxaparin activity levels are well predicted by single-dose pharmacokinetics. After repeated subcutaneous administration of the 1 mg/kg twice daily regimen, the steady state is reached from day 4 with mean exposure about 65% higher than after a single dose and mean peak and trough levels of about 1.2 and 0.52 IU/mL, respectively. Based on enoxaparin sodium pharmacokinetics, this difference in steady state is expected and within the therapeutic range.
Although not studied clinically, the 150 mg/mL concentration of enoxaparin sodium is projected to result in anticoagulant activities similar to those of 100 mg/mL and 200 mg/mL concentrations at the same enoxaparin dose. When a daily 1.5 mg/kg SC injection of enoxaparin sodium was given to 25 healthy male and female subjects using a 100 mg/mL or a 200 mg/mL concentration the following pharmacokinetic profiles were obtained [see Table 13].
{
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term studies in animals have been performed to evaluate the carcinogenic potential of enoxaparin. Enoxaparin was not mutagenic in in vitro tests, including the Ames test, mouse lymphoma cell forward mutation test, and human lymphocyte chromosomal aberration test, and the in vivo rat bone marrow chromosomal aberration test. Enoxaparin was found to have no effect on fertility or reproductive performance of male and female rats at SC doses up to 20 mg/kg/day or 141 mg/m2/day. The maximum human dose in clinical trials was 2.0 mg/kg/day or 78 mg/m2/day (for an average body weight of 70 kg, height of 170 cm, and body surface area of 1.8 m2).
Animal Toxicology and/or Pharmacology
A single SC dose of 46.4 mg/kg enoxaparin was lethal to rats. The symptoms of acute toxicity were ataxia, decreased motility, dyspnea, cyanosis, and coma.
Reproductive and Developmental Toxicology
Teratology studies have been conducted in pregnant rats and rabbits at SC doses of enoxaparin up to 30 mg/kg/day corresponding to 211 mg/m2/day and 410 mg/m2/day in rats and rabbits respectively. There was no evidence of teratogenic effects or fetotoxicity due to enoxaparin.
Clinical Studies
Prophylaxis of Deep Vein Thrombosis Following Abdominal Surgery in Patients at Risk for Thromboembolic Complications
Abdominal surgery patients at risk include those who are over 40 years of age, obese, undergoing surgery under general anesthesia lasting longer than 30 minutes or who have additional risk factors such as malignancy or a history of deep vein thrombosis (DVT) or pulmonary embolism (PE).
In a double-blind, parallel group study of patients undergoing elective cancer surgery of the gastrointestinal, urological, or gynecological tract, a total of 1116 patients were enrolled in the study, and 1115 patients were treated. Patients ranged in age from 32 to 97 years (mean age 67 years) with 52.7% men and 47.3% women. Patients were 98% Caucasian, 1.1% Black, 0.4% Asian and 0.4% others. Lovenox 40 mg SC, administered once a day, beginning 2 hours prior to surgery and continuing for a maximum of 12 days after surgery, was comparable to heparin 5000 U every 8 hours SC in reducing the risk of DVT. The efficacy data are provided below [see Table 14]. {
How Supplied
{
Storage
Store at 25°C (77°F); excursions permitted to 15–30°C (59–86°F) [See USP Controlled Room Temperature].
Images
Drug Images
{{#ask: Page Name::Sandbox Enoxaparin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Sandbox Enoxaparin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
If patients have had neuraxial anesthesia or spinal puncture, and particularly, if they are taking concomitant NSAIDs, platelet inhibitors, or other anticoagulants, they should be informed to watch for signs and symptoms of spinal or epidural hematoma, such as tingling, numbness (especially in the lower limbs) and muscular weakness. If any of these symptoms occur the patient should contact his or her physician immediately. Additionally, the use of aspirin and other NSAIDs may enhance the risk of hemorrhage. Their use should be discontinued prior to enoxaparin therapy whenever possible; if co-administration is essential, the patient's clinical and laboratory status should be closely monitored [see Drug Interactions (7)]. Patients should also be informed: of the instructions for injecting Lovenox if their therapy is to continue after discharge from the hospitals. it may take them longer than usual to stop bleeding. they may bruise and/or bleed more easily when they are treated with Lovenox. they should report any unusual bleeding, bruising, or signs of thrombocytopenia (such as a rash of dark red spots under the skin) to their physician [see Warnings and Precautions (5.1, 5.5)]. to tell their physicians and dentists they are taking Lovenox and/or any other product known to affect bleeding before any surgery is scheduled and before any new drug is taken [seeWarnings and Precautions (5.3)]. to tell their physicians and dentists of all medications they are taking, including those obtained without a prescription, such as aspirin or other NSAIDs [see Drug Interactions (7)]. sanofi-aventis U.S. LLC Bridgewater, NJ 08807 A SANOFI COMPANY
Precautions with Alcohol
Alcohol-Sandbox Enoxaparin interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Sandbox Enoxaparin Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Sandbox Enoxaparin Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 01.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 02.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 03.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 04.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 05.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 06.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 07.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 08.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 09.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 10.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 11.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 12.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 13.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 14.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 15.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin label 16.jpg
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin panel 01.png
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin panel 02.png
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin panel 03.png
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin panel 04.png
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin panel 05.png
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin panel 06.png
}}
{{#subobject:
|Label Page=Sandbox Enoxaparin |Label Name=Enoxaparin panel 07.png
}}