Rhinitis history and symptoms
|
Rhinitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Rhinitis history and symptoms On the Web |
|
American Roentgen Ray Society Images of Rhinitis history and symptoms |
|
Risk calculators and risk factors for Rhinitis history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Fatimo Biobaku M.B.B.S [2]
Overview
Rhinitis has significant impacts on the quality of life and productivity of the affected individual. Allergic rhinitis, which is the most common type of chronic rhinitis, is frequently underdiagnosed, mistreated, or sometimes ignored.[1] Effective management of rhinitis improves the quality of life, and control of coexisting conditions such as asthma and conjunctivitis.[2][3] Accurately diagnosing rhinitis by taking a careful history and physical examination, is important in order to ensure a timely intervention.[4]
History and Symptoms
History and Symptoms of Allergic Rhinitis[5][3][6][7]
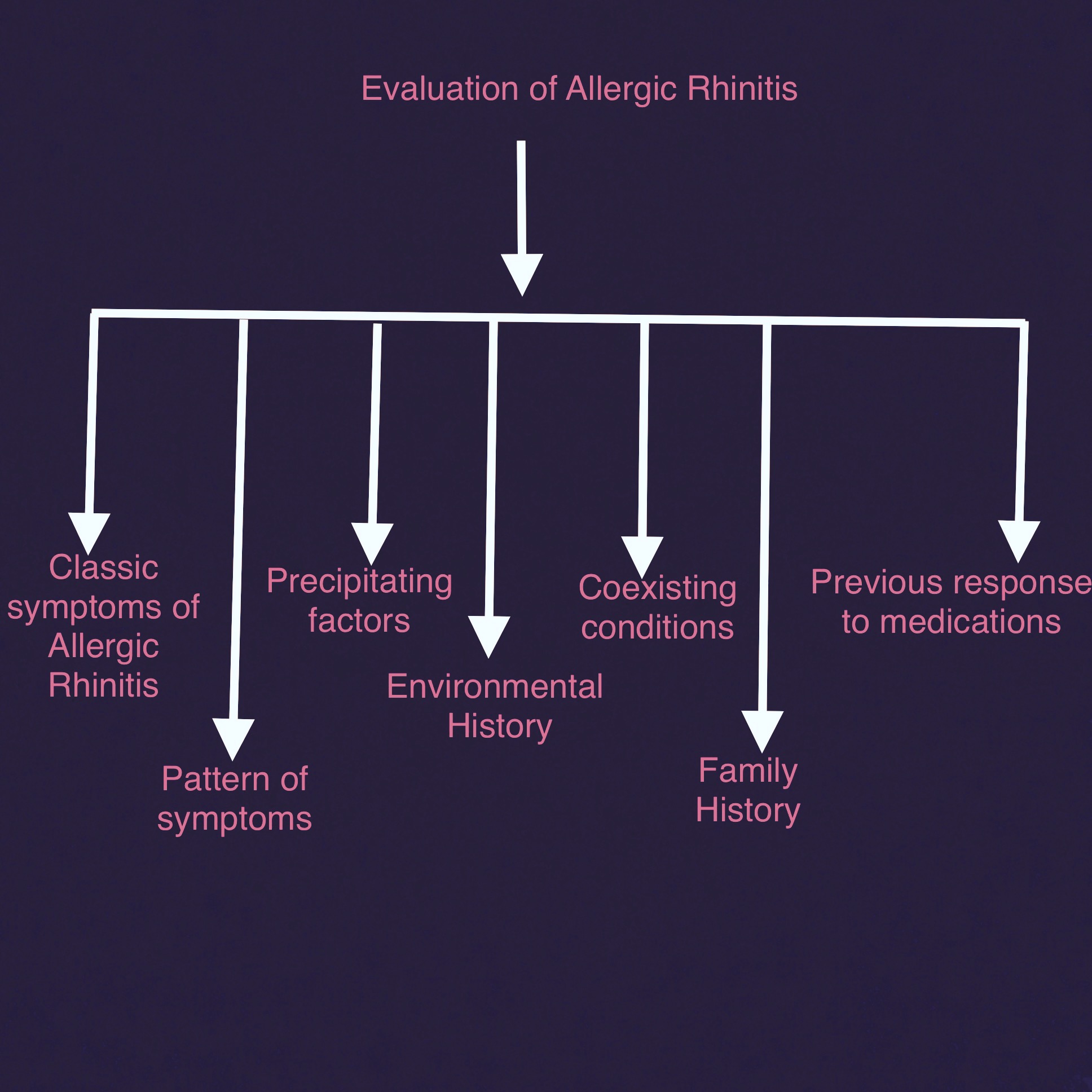
The algorithm below depicts important symptoms and history that should be evaluated when assessing a patient with rhinitis.
Symptoms of Allergic Rhinitis
- Bilateral, watery rhinorrhea- Consider other diagnosis such as intranasal foreign bodies in children if unilateral, mucopurulent rhinorrhea is seen
- Nasal pruritus- This is usually absent in nonallergic rhinitis
- Nasal congestion which often results in mouth breathing
- Sneezing (usually paroxysmal)
- Sniffing
- Frequent throat clearing
Pattern of symptoms of Allergic Rhinitis- It is important to ascertain the duration of the symptoms, the frequency, and the timing of the symptoms in relation to the allergen exposure, e.g
- Duration of symptoms in allergic rhinitis is usually >1hr on most days
- Intermittent symptoms
- Seasonal symptoms- Pollens are generally associated with seasonal allergic rhinitis (hay fever)
- Perrenial symptoms- There is very little variation between seasons for perrenial allergens like house dust mites, domestic pets, and cockroaches. Pollens in some parts of California and some other regions have also been identified to cause perennial symptoms.
Precipitating factors
- Identification of the allergen
- Identification of the symptoms that are present following exposure to the allergen
Environmental history- This should include a history of possible allergen exposure at places such as:
- The home environment
- The work place
- The school
- Other places
Coexisting conditions- Other conditions frequently coexists with Allergic Rhinitis, and they include:
- Allergic eye disease- Characterized by bilateral eye symptoms such as lacrimation, itching, redness. Allergic eye disease occurs in almost all patients with allergic rhinitis.[2]
- Asthma- Most patients with asthma have allergic rhinitis. Allergic rhinitis is a strong risk factor for the development of asthma, and it is also a major factor in the exacerbation of asthma.
- Oral allergy syndrome- Seen more often in individuals with pollen-induced allergic rhinitis, it occurs as a result of a cross-reaction of pollens with food derived from plants. Oral pruritus and/or local angioedema is seen in response to fruits and vegetables such as apples, hazelnuts, carrots, celery. Oral allergy syndrome has been estimated to affect about 25% of children with seasonal allergic rhinitis.
- Atopic dermatitis
- Adenoidal hypertrophy
References
- ↑ Greiner AN, Hellings PW, Rotiroti G, Scadding GK (2011). "Allergic rhinitis". Lancet. 378 (9809): 2112–22. doi:10.1016/S0140-6736(11)60130-X. PMID 21783242.
- ↑ 2.0 2.1 Shaker M, Salcone E (2016). "An update on ocular allergy". Curr Opin Allergy Clin Immunol. 16 (5): 505–10. doi:10.1097/ACI.0000000000000299. PMID 27490123.
- ↑ 3.0 3.1 Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A; et al. (2008). "Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen)". Allergy. 63 Suppl 86: 8–160. doi:10.1111/j.1398-9995.2007.01620.x. PMID 18331513.
- ↑ Skoner DP (2001). "Allergic rhinitis: definition, epidemiology, pathophysiology, detection, and diagnosis". J Allergy Clin Immunol. 108 (1 Suppl): S2–8. PMID 11449200.
- ↑ Rotiroti, Giuseppina; Scadding, Glenis (July 2016). "Allergic Rhinitis-an overview of a common disease". Paediatrics and Child Health. Volume 26 (Issue 7): 298–303. Retrieved January 20, 2017.
- ↑ Dykewicz MS, Hamilos DL (2010). "Rhinitis and sinusitis". J Allergy Clin Immunol. 125 (2 Suppl 2): S103–15. doi:10.1016/j.jaci.2009.12.989. PMID 20176255.
- ↑ Wallace DV, Dykewicz MS, Bernstein DI, Blessing-Moore J, Cox L, Khan DA; et al. (2008). "The diagnosis and management of rhinitis: an updated practice parameter". J Allergy Clin Immunol. 122 (2 Suppl): S1–84. doi:10.1016/j.jaci.2008.06.003. PMID 18662584.