Relapsing fever medical therapy: Difference between revisions
No edit summary |
Shanshan Cen (talk | contribs) No edit summary |
||
| Line 19: | Line 19: | ||
</ref> | </ref> | ||
==Treatment== | |||
===Antimicrobial regimen=== | |||
| Line 49: | Line 33: | ||
[[Category:Zoonoses]] | [[Category:Zoonoses]] | ||
[[Category:Infectious diseases]] | [[Category:Infectious diseases]] | ||
[[Category:Infectious Diseases Project]] | |||
Revision as of 15:08, 20 July 2015
|
Relapsing fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Relapsing fever medical therapy On the Web |
|
American Roentgen Ray Society Images of Relapsing fever medical therapy |
|
Risk calculators and risk factors for Relapsing fever medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Medical Therapy
Pharmacotherapy
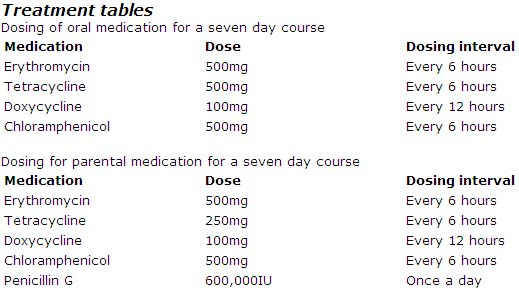
Erythromycin, tetracyclines, chloramphenicol, or penicillins have all been shown to be effective for treating TBRF. Although duration of therapy has not been well studied for TBRF, the current recommendation is seven days of antibiotic therapy. In contrast, LBRF caused by B. recurrentis can be treated with a single dose of antibiotics.
For young children and pregnant women either erythromycin and/or penicillin are recommended for treatment of TBRF.
When initiating antibiotic therapy, a patient should be watched closely for a Jarisch-Herxheimer reaction for the first 4 hours after the antibiotic is given (Negussie, Remick et al. 1992). The reaction may be difficult to distinguish from a febrile crisis, with rigors and decreased blood pressure. Cooling blankets and appropriate use of antipyrectic agents may be indicated. The Jarisch-Herxheimer reaction produces apprehension, diaphoresis, fever, tachycardia, and tachypnea with an initial pressor response followed rapidly by hypotension. Recent studies have shown that tumor necrosis factor-alpha (TNF-alpha) may be partly responsible for the reaction.
Acute Pharmacotherapies
The CDC has not developed specific treatment guidelines for TBRF. Below are the treatment recommendations as outlined in Harrisons Principles of Internal Medicine. 16th edition. 2004. p 994.