Pulmonary edema: Difference between revisions
No edit summary |
No edit summary |
||
| Line 21: | Line 21: | ||
==Natural History, Complications and Prognosis== | ==Natural History, Complications and Prognosis== | ||
If left untreated, acute pulmonary edema can lead to [[coma]] and even death, generally due to its main complication of [[Hypoxia (medical)|hypoxia]]. | If left untreated, acute pulmonary edema can lead to [[coma]] and even death, generally due to its main complication of [[Hypoxia (medical)|hypoxia]]. | ||
==Echocardiography== | ==Echocardiography== | ||
Revision as of 02:05, 19 August 2011
| Pulmonary edema | |
 | |
|---|---|
| Chest x-ray showing pulmonary edema | |
| ICD-10 | J81 |
| ICD-9 | 514 |
| DiseasesDB | 11017 |
| MedlinePlus | 000140 |
|
Pulmonary edema Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pulmonary edema On the Web |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Natural History, Complications and Prognosis
If left untreated, acute pulmonary edema can lead to coma and even death, generally due to its main complication of hypoxia.
Echocardiography
Echocardiography is useful in confirming a cardiac or no-cardiac cause of pulmonary edema. Among cardiac causes, echocardiography can identify if systolic or diastolic dysfunction is present. Echocardiography is useful in identify if focal segment wall motion abnormalities are present which would suggest ischemia or myocardial infarction as an underlying cause. If there is a global impairment of left ventricular function, then this suggests a cardiomyopathy may be present. Echocardiography may identify the presence and severity of valvular causes of pulmonary edema including aortic stenosis, aortic insufficiency, mitral stenosis. mitral insufficiency, and hypertrophic cardiomyopathy.
Cardiac Catheterization
Insertion of a pulmonary arterial catheter (a.k.a. a Swan-Ganz catheter) may be required to distinguish between the two main forms of pulmonary edema and to help guide management[1]. In patients with cardiogenic pulmonary edema the pulmonary artery pressure will be elevated. Among patients with non-cardiogenic pulmonary edema the wedge pressure will not be elevated.
Treatment
See also the chapter on congestive heart failure.
Acute Pulmonary Edema
In patients with acute pulmonary edema, the goal is to reduce both preload and afterload and to diurese the patient. Intravenous nitroglycerin can be used to reduce both the preload and afterload. Diuretics such as furosemide or bumetanide can be used to reduce volume overload. The dose that the patient is on chronically should be doubled and administered intravenously in the setting of flash pulmonary edema. Morphine sulfate may be helpful in reducing the drive to breathe, improving patient comfort, and reducing the preload.
Oxygen therapy is required to minimize cyanosis and to maintain adequate oxygenation. High-flow oxygen, noninvasive ventilation (either continuous positive airway pressure (CPAP) or variable positive airway pressure (VPAP) may be effective[2][3]). If the simple measures are not effective then mechanical ventilation may be required.
Treatment should also be directed at managing the underlying cause of an episode of acute pulmonary edema. This would include managing as acute myocardial infarction, mitral regurgitation, aortic regurgitation, or any other condition that causes an increase in left ventricular filling pressures.
Chronic Pulmonary Edema
Reoccurrence of FPE is thought to be associated with hypertension[4] and may signify renal artery stenosis.[5] Prevention of reoccurrence is based on managing hypertension, coronary artery disease, renovascular hypertension, and heart failure.
Pathology and Case Report
Clinical Summary
A 69-year-old male with well-controlled Type I diabetes mellitus (insulin-dependent) presented with upper abdominal and lower chest pain of four hours duration and accompanied by shortness of breath and diaphoresis.
An electrocardiogram revealed multiple premature ventricular contractions (PVCs).
The hospital course was characterized by recurrent pulmonary edema and oliguria.
The terminal event was cardiac arrest.
Autopsy Study
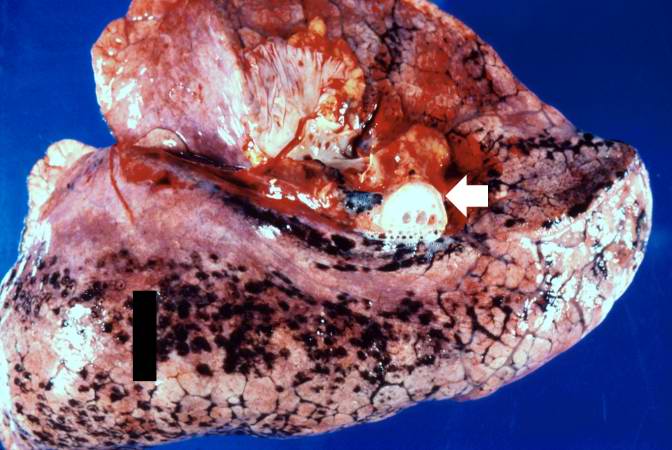
Significant findings at postmortem examination were old and recent myocardial infarctions and evidence of congestive heart failure.
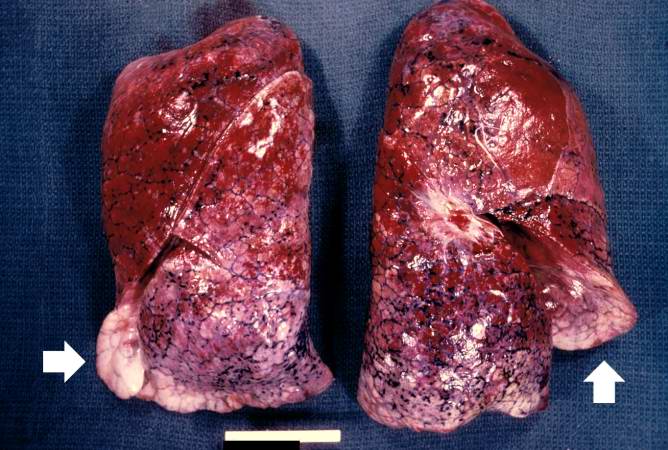
The right and left lungs weighed 950 grams and 750 grams, respectively, and were reddish-brown.
Histopathological Findings
-
This is a gross photograph of lungs that are distended and red. The reddish coloration of the tissue is due to congestion. Some normal pink lung tissue is seen at the edges of the lungs (arrows).
-
This is a gross photograph of lung demonstrating acute pulmonary congestion and edema. A frothy exudate fills the bronchus (arrow).
-
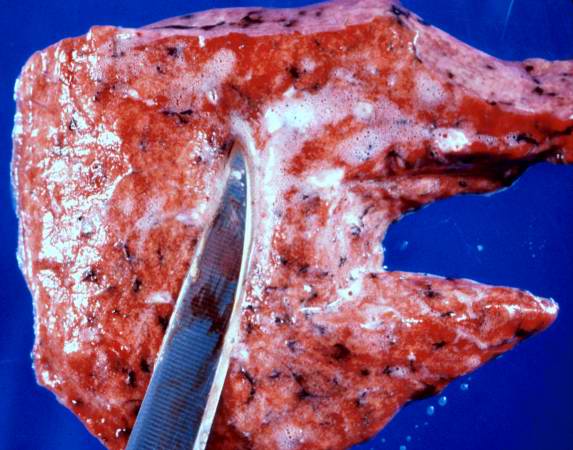
This gross photograph demonstrates the frothy exudate that is being extruded from the lung tissue.
-
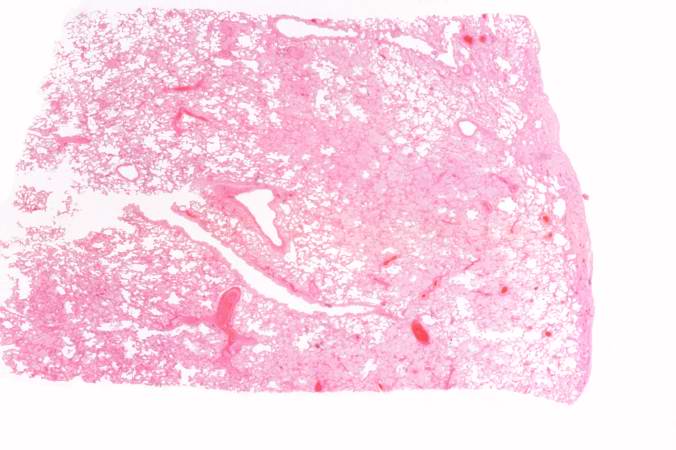
This is a low-power photomicrograph of lung from this case. The lung section has a pale-red color indicating proteinaceous material within the lung.
-
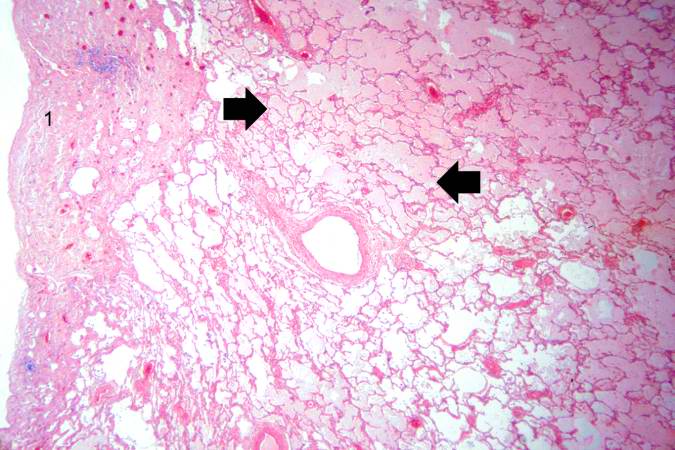
This is a higher-power photomicrograph of lung. The edema fluid within the alveoli is visible at this higher magnification (arrows). The thickened pleura (1) is on the left.
-
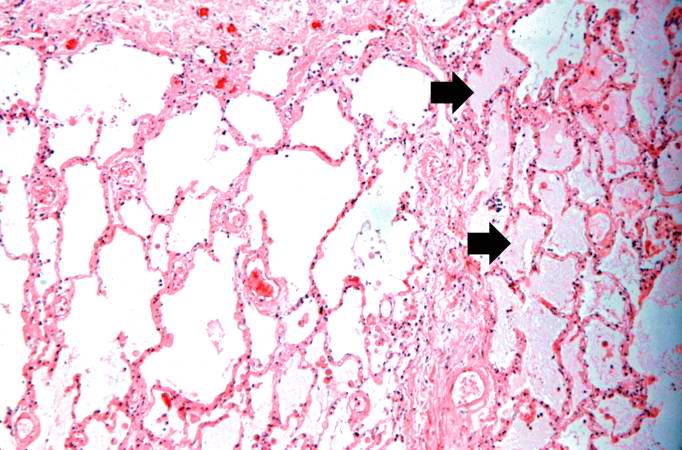
This is a higher-power photomicrograph showing edema-filled alveoli in the right portion of this section (arrows).
-
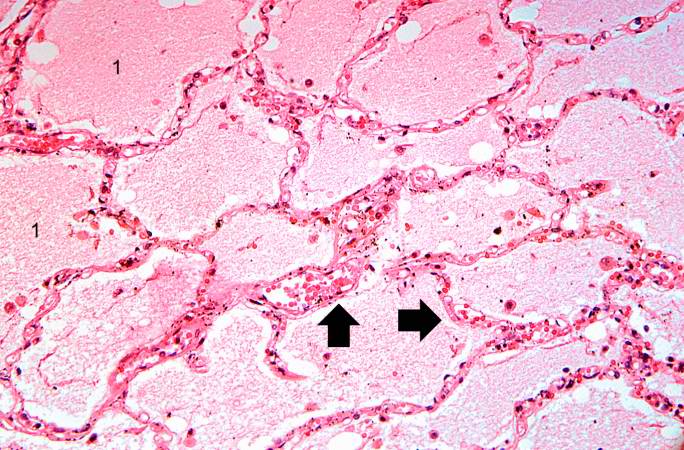
This high-power photomicrograph illustrates the edema fluid within the alveoli (1) and the congestion (RBCs) in the alveolar capillaries (arrows).
References
- ↑
- ↑ Masip J, Roque M, Sanchez B, Fernandez R, Subirana M, Exposito JA. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA 2005;294:3124-30. PMID 16380593.
- ↑ Peter JV, Moran JL, Phillips-Hughes J, Graham P, Bersten AD. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet 2006;367(9517):1155-63. PMID 16616558.
- ↑ Kramer K, Kirkman P, Kitzman D, Little WC. Flash pulmonary edema: association with hypertension and reoccurrence despite coronary revascularization. Am Heart J. 2000 Sep;140(3):451-5. PMID 10966547.
- ↑ Pickering TG, Herman L, Devereux RB, Sotelo JE, James GD, Sos TA, Silane MF, Laragh JH. Recurrent pulmonary oedema in hypertension due to bilateral renal artery stenosis: treatment by angioplasty or surgical revascularisation. Lancet 1988;2(8610):551-2. PMID 2900930.
See also
Template:Respiratory pathology
bs:Akutni edem pluća de:Höhenlungenödem ko:폐부종 it:Edema polmonare acuto he:בצקת ריאות nl:Longoedeem new:पल्मोनरी इडिमा sr:Акутни едем плућа fi:Keuhkoödeema sv:Lungödem