Pheochromocytoma pathophysiology: Difference between revisions
| Line 19: | Line 19: | ||
==Genetics== | ==Genetics== | ||
Pheochromocytomas can be familial and occur in patients with [[multiple endocrine neoplasia]] (MEN 2 and MEN 3). Patients with Von Hippel Lindau ([[VHL]]) may also develop pheocromocytoma.<ref name="pmid24642075">{{cite journal| author=Shuch B, Ricketts CJ, Metwalli AR, Pacak K, Linehan WM| title=The genetic basis of pheochromocytoma and paraganglioma: implications for management. | journal=Urology | year= 2014 | volume= 83 | issue= 6 | pages= 1225-32 | pmid=24642075 | doi=10.1016/j.urology.2014.01.007 | pmc=4572836 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24642075 }}</ref> It is autosomal dominant inheritance and has two pathways of tumor pathogenesis. Cluster 1 tumorsare noradrenergic. Cluster 2 tumors are adrenergic.<ref name="pmid23933153">{{cite journal| author=King KS, Pacak K| title=Familial pheochromocytomas and paragangliomas. | journal=Mol Cell Endocrinol | year= 2014 | volume= 386 | issue= 1-2 | pages= 92-100 | pmid=23933153 | doi=10.1016/j.mce.2013.07.032 | pmc=3917973 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23933153 }}</ref> | * Pheochromocytomas can be familial and occur in patients with [[multiple endocrine neoplasia]] (MEN 2 and MEN 3). | ||
* Patients with Von Hippel Lindau ([[VHL]]) may also develop pheocromocytoma.<ref name="pmid24642075">{{cite journal| author=Shuch B, Ricketts CJ, Metwalli AR, Pacak K, Linehan WM| title=The genetic basis of pheochromocytoma and paraganglioma: implications for management. | journal=Urology | year= 2014 | volume= 83 | issue= 6 | pages= 1225-32 | pmid=24642075 | doi=10.1016/j.urology.2014.01.007 | pmc=4572836 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24642075 }}</ref> | |||
* It is autosomal dominant inheritance and has two pathways of tumor pathogenesis. Cluster 1 tumorsare noradrenergic. Cluster 2 tumors are adrenergic.<ref name="pmid23933153">{{cite journal| author=King KS, Pacak K| title=Familial pheochromocytomas and paragangliomas. | journal=Mol Cell Endocrinol | year= 2014 | volume= 386 | issue= 1-2 | pages= 92-100 | pmid=23933153 | doi=10.1016/j.mce.2013.07.032 | pmc=3917973 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23933153 }}</ref> | |||
{| class="wikitable" | {| class="wikitable" | ||
!Cluster 1 | !Cluster 1 | ||
| Line 36: | Line 38: | ||
==Associated conditions== | ==Associated conditions== | ||
Pheochromocytoma can be part of other syndromes named Multiple endocrien neoplasia (MEN2) Which are autosomal dominant syndromes controlled by RET gene. Pheochromocytoma occurs in 50% of patients with MEN2 as follows: | * Pheochromocytoma can be part of other syndromes named Multiple endocrien neoplasia (MEN2) Which are autosomal dominant syndromes controlled by RET gene. Pheochromocytoma occurs in 50% of patients with MEN2 as follows: | ||
{| class="wikitable" | {| class="wikitable" | ||
!MEN1 | !MEN1 | ||
Revision as of 19:31, 5 July 2017
|
Pheochromocytoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pheochromocytoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Pheochromocytoma pathophysiology |
|
Risk calculators and risk factors for Pheochromocytoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmad Al Maradni, M.D. [2]
Overview
Pheochromocytoma arise from chromaffin cells of the adrenal medulla.On gross pathology, pheochromocytoma has a multinodular and a multicentric pattern of growth. On microscopic histopathological analysis, nesting (Zellballen) pattern composed of well-defined clusters of tumor cells separated by fibrovascular stroma is a characteristic finding.it may be benign or malignant, familial origin(multiple endocrine neoplasia type 2) or sporadic one. Both of them have genetic origin depends on large number of genes: VHL, SDH, NF1, RET.
Pathophysiology
Pheochromocytoma arise from chromaffin cells of the adrenal medulla and sympathetic ganglia. Traditionally pheochromocytoma known as the "10% tumor":
- Approximately 10% of patients have bilateral disease
- Approximately 10% of tumors are malignant
- Approximately 10% are located in chromaffin tissue outside of the adrenal gland, The most common extradrenal locations are the abdomen and thorax .
- Approximately 10% occur in childhood
- Approximately 10% are familial
- Approximately 10% recur after being resected
- Approximately 10% of patients do not have hypertension
Malignant and benign pheochromocytomas are the same; The only difference is the ability to spread locally and distant. [1]
Genetics
- Pheochromocytomas can be familial and occur in patients with multiple endocrine neoplasia (MEN 2 and MEN 3).
- Patients with Von Hippel Lindau (VHL) may also develop pheocromocytoma.[2]
- It is autosomal dominant inheritance and has two pathways of tumor pathogenesis. Cluster 1 tumorsare noradrenergic. Cluster 2 tumors are adrenergic.[3]
| Cluster 1 | Cluster 2 |
|---|---|
|
|
. Patients with the succinate dehydrogenase B mutations are likely to develop malignant disease.[4]
Associated conditions
- Pheochromocytoma can be part of other syndromes named Multiple endocrien neoplasia (MEN2) Which are autosomal dominant syndromes controlled by RET gene. Pheochromocytoma occurs in 50% of patients with MEN2 as follows:
| MEN1 | MEN2 |
|---|---|
|
|
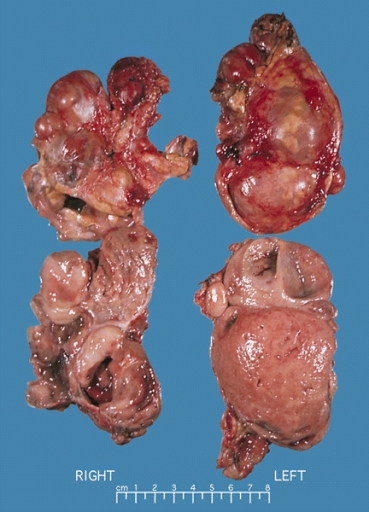
Gross Pathology
On gross pathology, A multinodular and multicentric pattern of growth of pheochromocytoma may be seen.
-
Bilateral pheochromocytoma in MEN2. Gross image.
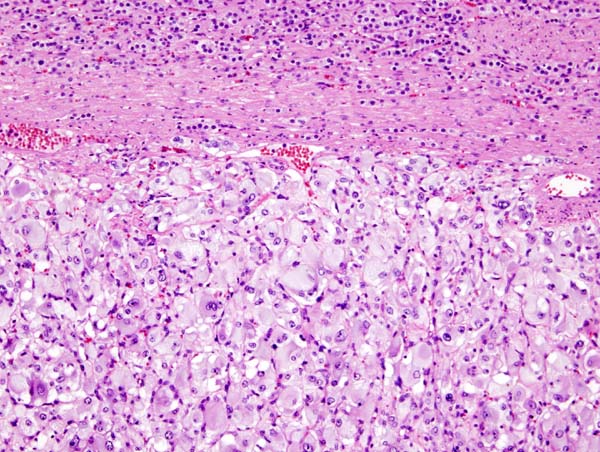
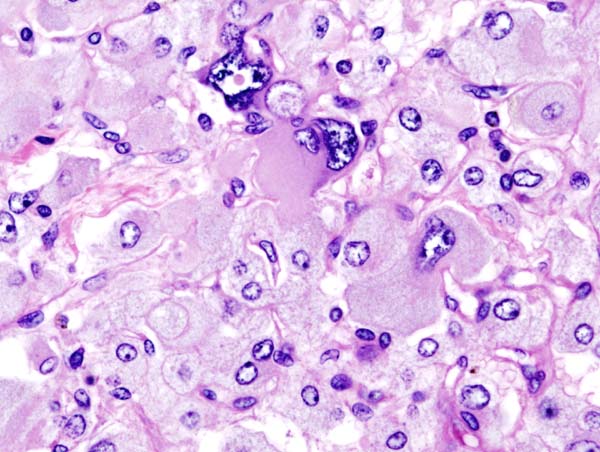
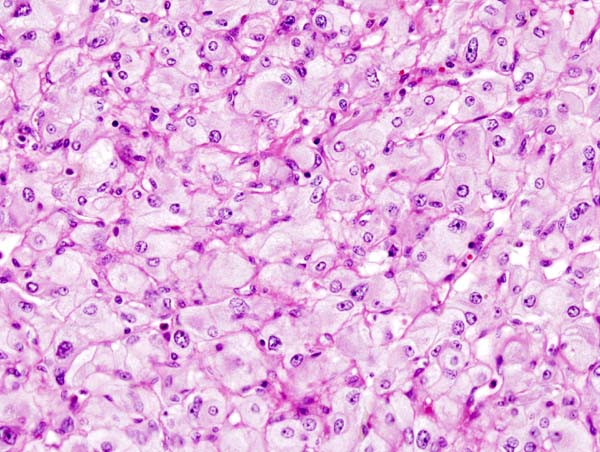
Microscopic Pathology
On microscopic pathology, Pheochromocytoma typically demonstrates a nesting (Zellballen) pattern on microscopy. This pattern is composed of well-defined clusters of tumor cells containing eosinophilic cytoplasm separated by fibrovascular stroma.
-
Micrograph of pheochromocytoma.
-
Histopathology of adrenal pheochromocytoma. Adrenectomy specimen.
-
Micrograph of pheochromocytoma.
-
Micrograph of pheochromocytoma.
Videos
{{#ev:youtube|7yjxG3KmX98}}
References
- ↑ Goldstein RE, O'Neill JA, Holcomb GW, Morgan WM, Neblett WW, Oates JA; et al. (1999). "Clinical experience over 48 years with pheochromocytoma". Ann Surg. 229 (6): 755–64, discussion 764-6. PMC 1420821. PMID 10363888.
- ↑ Shuch B, Ricketts CJ, Metwalli AR, Pacak K, Linehan WM (2014). "The genetic basis of pheochromocytoma and paraganglioma: implications for management". Urology. 83 (6): 1225–32. doi:10.1016/j.urology.2014.01.007. PMC 4572836. PMID 24642075.
- ↑ King KS, Pacak K (2014). "Familial pheochromocytomas and paragangliomas". Mol Cell Endocrinol. 386 (1–2): 92–100. doi:10.1016/j.mce.2013.07.032. PMC 3917973. PMID 23933153.
- ↑ Neumann HP, Pawlu C, Peczkowska M, Bausch B, McWhinney SR, Muresan M; et al. (2004). "Distinct clinical features of paraganglioma syndromes associated with SDHB and SDHD gene mutations". JAMA. 292 (8): 943–51. doi:10.1001/jama.292.8.943. PMID 15328326.