Pericardial effusion: Difference between revisions
No edit summary |
No edit summary |
||
| Line 13: | Line 13: | ||
MeshID = D010490 | | MeshID = D010490 | | ||
}} | }} | ||
{{ | {{Pericardial effusion}} | ||
{{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | ||
| Line 19: | Line 19: | ||
==Overview== | ==Overview== | ||
== Differential Diagnosis of {{PAGENAME}}== | == Differential Diagnosis of {{PAGENAME}}== | ||
Revision as of 17:23, 17 July 2011
| Pericardial effusion | |
 | |
|---|---|
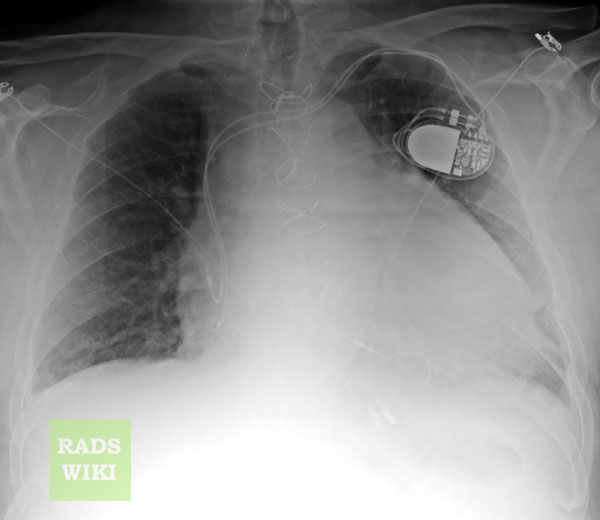
| Pericardial effusion. Image courtesy of RadsWiki | |
| ICD-10 | I30, I31.3 |
| ICD-9 | 420 |
| DiseasesDB | 2128 |
| eMedicine | med/1786 |
| MeSH | D010490 |
|
Pericardial effusion Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pericardial effusion On the Web |
|
American Roentgen Ray Society Images of Pericardial effusion |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
See also: pericarditis, constrictive pericarditis and cardiac tamponade
Overview
Differential Diagnosis of Pericardial effusion
Serous
- Acute pancreatitis
- Chemotherapeutics
- Chronic disease
- Cirrhosis
- Congestive heart failure
- Dressler's syndrome
- Hypoalbuminemia
- Hypothyroidism
- Infection
- Irradiation
- Malnutrition
- Nephrotic Syndrome
Blood
- Acute myocardial infarction
- Anticoagulants
- Aortic rupture
- Cardiac catheterization
- Chemotherapeutics
- Coagulotherapy
- Heart surgery
- Neoplasm
- Perforation
- Trauma
- Uremia
Lymph or chylous
- Benign obstruction of thoracic duct
- Idiopathic
- Neoplasm
Metastatic tumor
Miscellaneous
Infectious
Noninfectious
- Idiopathic
- Uremia: Kidney failure with excessive blood levels of urea nitrogen
- Heart surgery[1]
- Neoplasia that has spread to the pericardium
- Acute myocardial infarction: Post myocardial infarction pericarditis (Dressler's syndrome)
- Postirradiation
- Aortic dissection (with leakage into pericardial sac)
- Trauma
- Sarcoidosis
- Pericarditis
- Rheumatic fever
- Collagen vascular disease
- Drug-induced
- Inflammatory disease, such as lupus
- Pericarditis
Types
Transudative
Exudative
- tuberculosis,
- spread from empyema
Hemorrhagic
Symptoms
Chest pain, pressure symptoms. A small effusion may have no symptoms.
Pericardial effusion is also present after a specific type of heart defect repair. An Atrial Septal Defect Secundum, or ASD, when repaired will most likely produce a pericardial effusion due to one of the methods of repair. One repair method of an ASD is to take a piece of the peridcardial tissue and use it as a patch for the hole in the atrial cavity.
Diagnosis
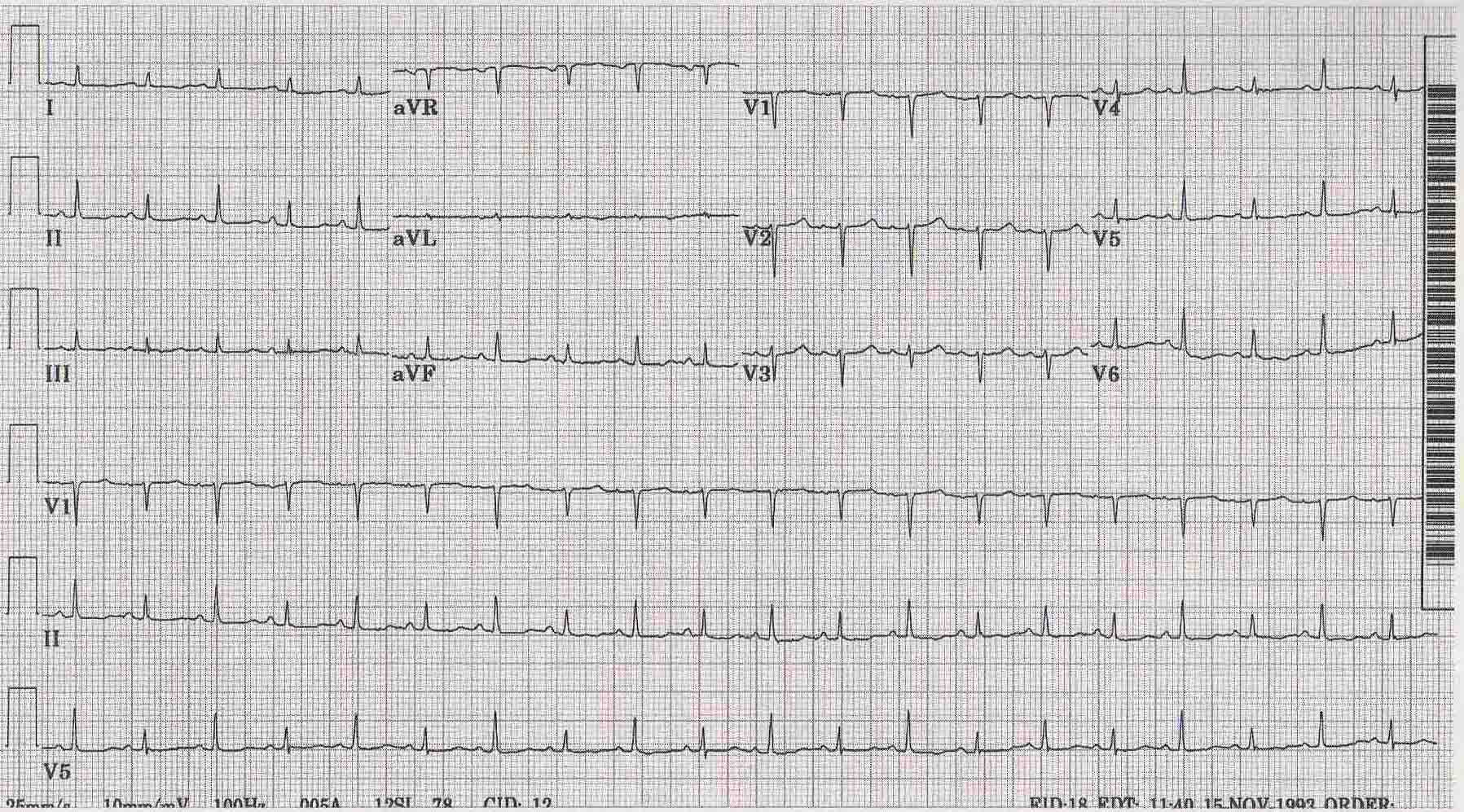
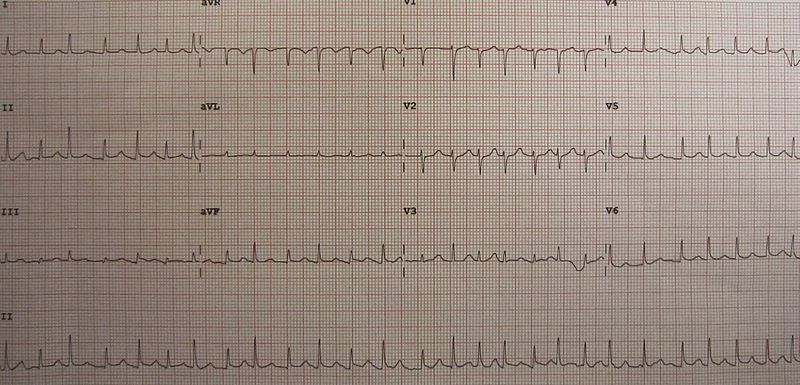
EKG
-
Pericardial Effusion
-
An ECG showing electrical alternans in a person with pericardial effusion.
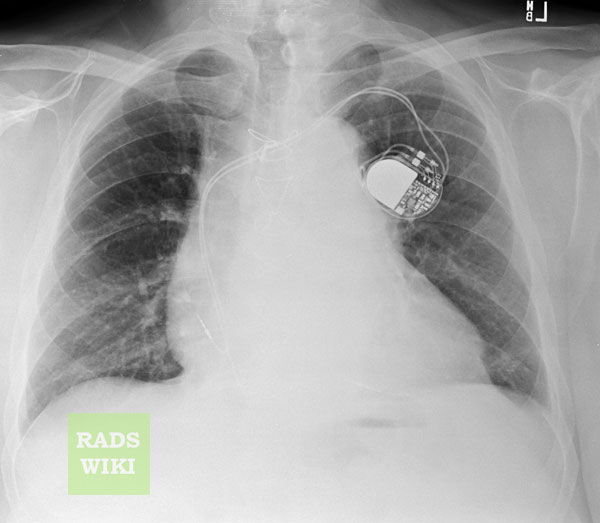
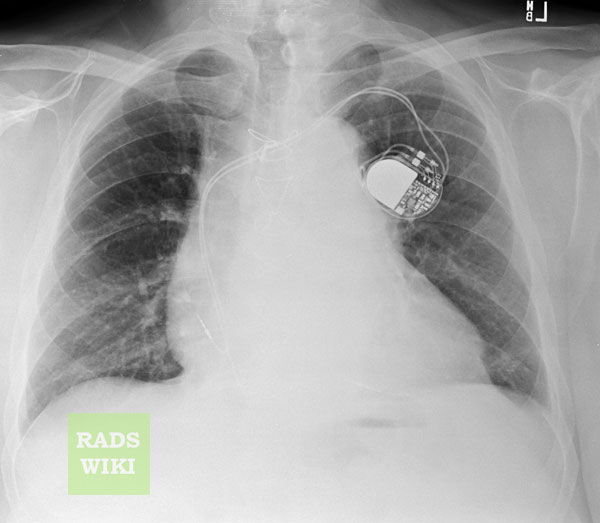
Chest X-Ray


Images shown below are courtesy of RadsWiki
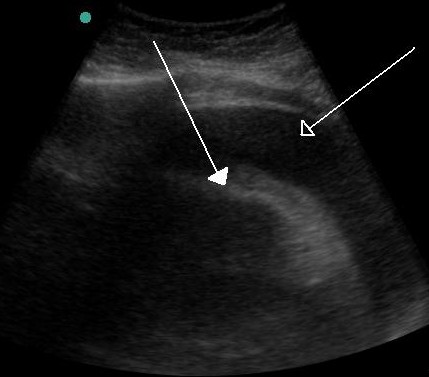
Echocardiography
CT and MRI
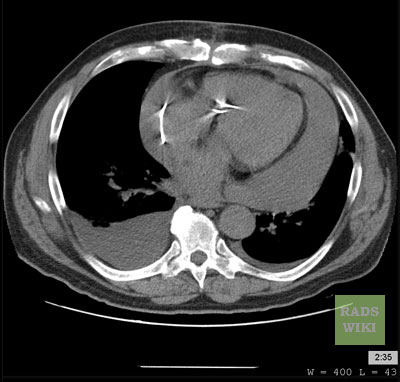
Cross-sectional imaging by CT or MRI is very sensitive in the detection of generalized or loculated pericardial effusions. Some fluid in the pericardial sac contributes to the apparent thickness and should be considered normal. Commonly, free-flowing fluid accumulates first at the posterolateral aspect of the left ventricle, when the patient is imaged in the supine position.
Estimation of the amount of fluid is possible to a limited extent based on the overall thickness of the crescent of fluid. Compared to cardiac ultrasound, CT and MRI may be particularly helpful in detecting loculated effusions, owing to the wide field of view provided by these techniques. Hemorrhagic effusions can be differentiated from a transudate or an exudate based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). Pulsation artefacts may cause local areas of low signal in a hemorrhagic effusion. Effusions are often incidentally noted on CT scans obtained for other indications.
Pericardial thickening (thickness >4 mm) is difficult to differentiate from a small generalized effusion. Both entities will reveal a low signal/density line that is thicker than the normal pericardial thickness. In acute pericarditis, the pericardial lining can show intermediate signal intensity and may enhance after gadolinium administration.
CT
- CT attenuation measurements also enable the initial characterization of pericardial fluid.
- A fluid collection with attenuation close to that of water is likely to be a simple effusion.
- Attenuation greater than that of water suggests malignancy, hemopericardium, purulent exudate, or effusion associated with hypothyroidism.
- Pericardial effusions with low attenuation also have been reported in cases of chylopericardium.
Images shown below are courtesy of RadsWiki

MRI
- The appearance of pericardial fluid is different on SE and GRE cine MR images.
- Nonhemorrhagic fluid has low signal intensity on T1-weighted SE images and high intensity on GRE cine images. Conversely, hemorrhagic effusion is characterized by high signal intensity on T1-weighted SE images and low intensity on GRE cine images.
- When an effusion is secondary to malignancy, an irregularly thickened pericardium or pericardial nodularity may be depicted on MR images.
Cardiac Catheterization
Flouroscopic images show pericardial effusion:
<googlevideo>-7129815717409714366&hl=en</googlevideo>
<googlevideo>7051277599064845698&hl=en</googlevideo>
<googlevideo>1013614061451207857&hl=en</googlevideo>
<googlevideo>3444457597731375301&hl=en</googlevideo>
Treatment
Treatment depends on the underlying cause and the severity of the heart impairment. Pericardial effusion due to a viral infection usually goes away within a few weeks without treatment. Some pericardial effusions remain small and never need treatment. If the pericardial effusion is due to a condition such as lupus, treatment with anti-inflammatory medications may help. If the effusion is compromising heart function and causing cardiac tamponade, it will need to be drained, most commonly by a needle inserted through the chest wall and into the pericardial space. A drainage tube is often left in place for several days. In some cases, surgical drainage may be required by pericardiocentesis, in which a needle, and sometimes a catheter are used to drain excess fluid.
References
- ↑ Pericardial effusion:What are the symptoms?, Dr. Martha Grogan M.D.