Pain diagnosis
|
Pain |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pain diagnosis On the Web |
|
American Roentgen Ray Society Images of Pain diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Diagnosis
There is no way to tell how much pain a person has. No test can measure the intensity of pain, no imaging device can show pain, and no instrument can locate pain precisely. Sometimes, as in the case of headaches, physicians find that the best aid to diagnosis is the patient's own description of the type, duration, and location of pain. Defining pain as sharp or dull, constant or intermittent, burning or aching may give the best clues to the cause of pain. These descriptions are part of what is called the pain history, taken by the physician during the preliminary examination of a patient with pain.
Physicians, however, do have a number of technologies they use to find the cause of pain. Primarily these include:
- Electrodiagnostic procedures include electromyography (EMG), nerve conduction studies, and evoked potential (EP) studies. Information from EMG can help physicians tell precisely which muscles or nerves are affected by weakness or pain. Thin needles are inserted in muscles and a physician can see or listen to electrical signals displayed on an EMG machine. With nerve conduction studies the doctor uses two sets of electrodes (similar to those used during an electrocardiogram) that are placed on the skin over the muscles. The first set gives the patient a mild shock that stimulates the nerve that runs to that muscle. The second set of electrodes is used to make a recording of the nerve's electrical signals, and from this information the doctor can determine if there is nerve damage. EP tests also involve two sets of electrodes-one set for stimulating a nerve (these electrodes are attached to a limb) and another set on the scalp for recording the speed of nerve signal transmission to the brain.
- Imaging, especially magnetic resonance imaging or MRI, provides physicians with pictures of the body's structures and tissues. MRI uses magnetic fields and radio waves to differentiate between healthy and diseased tissue.
- A neurological examination in which the physician tests movement, reflexes, sensation, balance, and coordination.
- X-rays produce pictures of the body's structures, such as bones and joints
To establish an understanding of an individual's pain, health-care practitioners will typically try to establish certain characteristics of the pain: site, onset and offset, character, radiation, associated symptoms, time pattern, exacerbating and ameliorating factors and severity.[1]
By using the gestalt of these characteristics, the source or cause of the pain can often be established. A complete diagnosis of pain will require also to look at the patient's general condition, symptoms, and history of illness or surgery. The physician may order blood tests, X-rays, scans, EMG, etc. Pain clinics may investigate the person's psychosocial history and situation.
Pain assessment also uses the concepts of pain threshold, the least experience of pain which a subject can recognize, and pain tolerance, the greatest level of pain which a subject is prepared to tolerate. Among the most frequent technical terms for referring to abnormal perturbations in pain experience, there are:
- allodynia, pain due to a stimulus which does not normally provoke pain,
- hyperalgesia, an increased response to a stimulus which is normally painful,
- hypoalgesia, diminished pain in response to a normally painful stimulus.[2]
Verbal characterization
A key characteristic of pain is its quality. Typical descriptions of pain quality include sharp, stabbing, tearing, squeezing, cramping, burning, lancinating (electric-shock like), or heaviness. It may be experienced as throbbing, dull, nauseating, shooting or a combination of these. Indeed, individuals who are clearly in extreme distress such as from a myocardial infarction may not describe the sensation as pain, but instead as an extreme heaviness on the chest. Another individual with pain in the same region and with the same intensity may describe the pain as tearing which would lead the practitioner to consider aortic dissection. Inflammatory pain is commonly associated with some degree ofitch sensation, leading to a chronic urge to rub or otherwise stimulate the affected area. The difference between these diagnoses and many others rests on the quality of the pain.
Numeric rating scale
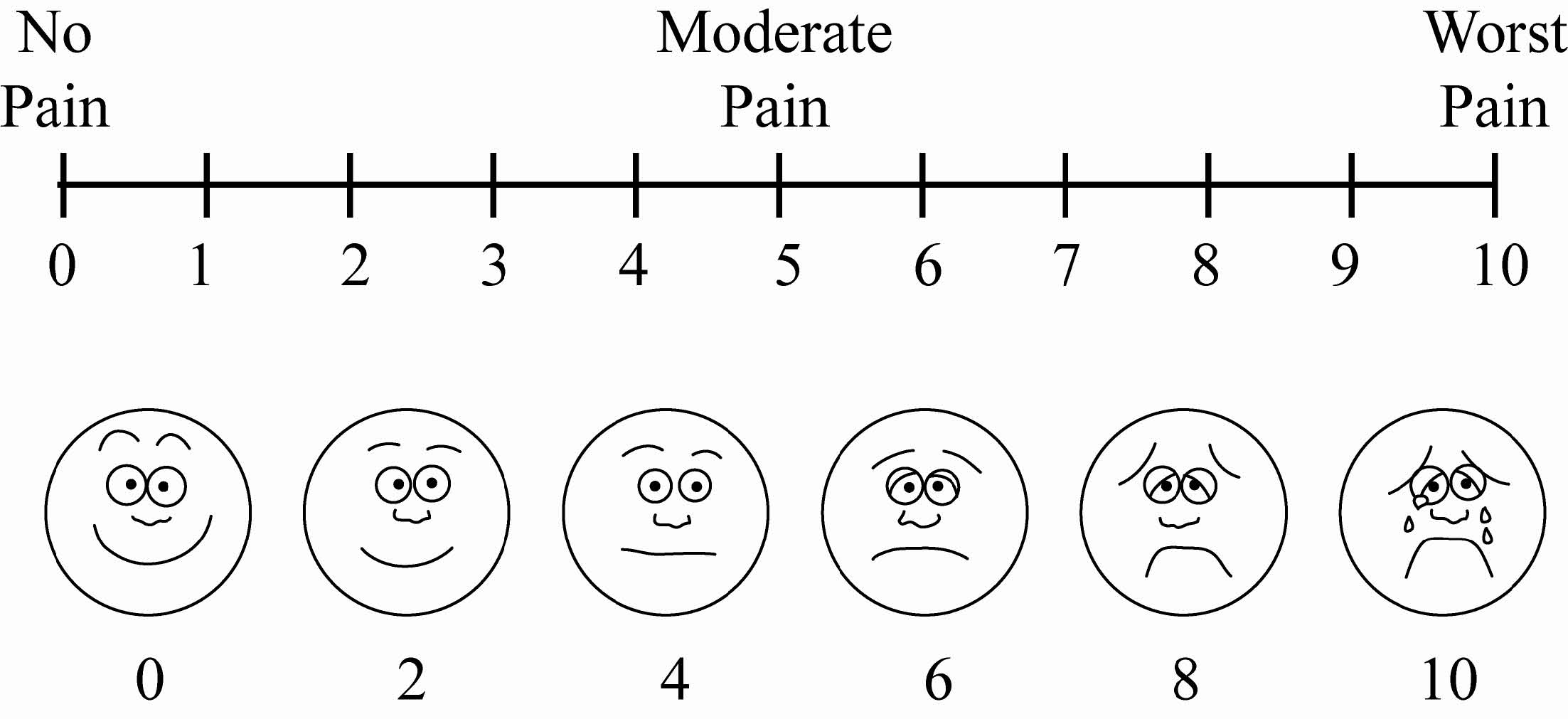
Pain may be quantified on a pain numeric rating scale (NRS) that ranges from 0-10 points (0 means no pain); however, the accuracy of such as scale (using a cut point of 4 or more) for predicting pain that interferes with functioning is:[3]
- sensitivity 64%
- specificity 83%
This score does not correlate with heart rate.[4]
Visual analog scale
Visual analog scales (VAS) have been used to measure pain. An observational study concluded "the minimum clinically significant change in patient pain severity measured with a 100-mm visual analog scale was 13 mm."[5]
The PEG is a 3 item scale that rates pain and its impact on the patient's life.[6]
Other scales
The McGill Pain Questionnaire is available.[7]
Intensity
Pain may range in intensity from slight through severe to agonizing and can appear as constant or intermittent. The threshold of pain varies widely between individuals. Many attempts have been made to create a pain scale that can be used to quantify pain, for instance on a numeric scale that ranges from 0 to 10 points. In this scale, zero would be no pain at all and ten would be the worst pain imaginable. The purpose of these scales is to monitor an individual's pain over time, allowing care-givers to see how a patient responds to therapy for example. Accurate quantification can also allow researchers to compare results between groups of patients.
Localization
Pains are usually called according to their subjective localization in a specific area or region of the body: headache, toothache, shoulder pain, abdominal pain, back pain, joint pain, myalgia, etc. Localization is not always accurate in defining the problematic area, although it will often help narrow the diagnostic possibilities. Some pain sensations may be diffuse (radiating) or referred. Radiation of painoccurs in neuralgia when stimulus of a nerve at one site is perceived as pain in the sensory distribution of that nerve. Sciatica, for instance, involves pain running down the back of the buttock, leg and bottom of foot that results from compression of a nerve root in the lumbar spine. Referred pain usually happens when sensory fibres from the viscera enter the same segment of the spinal cord as somatic nerves i.e. those from superficial tissues. The sensory nerve from the viscera stimulates the nearby somatic nerve so that the pain localization in the brain is confused. A well-known example is when the pain of a heart attack is felt in the left arm rather than in the chest.[8]
Nurses use the PQRST method to qualify the pain
P = provocation / palliation : what were you doing when the pain started? What caused it? What makes it better? worse? What seems to trigger it? Stress? Position? Certain activities? Arguments? Does it seem to be getting better, or getting worse, or does it remain the same? What relieves it: changing diet? changing position? taking medications? being active? resting? What makes (the problem) worse?
Q = quality / quantity : What does it feel like? Is it sharp? Dull? Stabbing? Burning? Crushing? throbbing? nauseating? shooting? twisting? stretching? Other? (The person who is suffering the pain should describe the pain, rather than saying what they think you would like to hear.) How does it feel, look or sound? How much of it is there?
R = region / radiation : Where is the pain located? Does the pain radiate (i.e. spread to another location, eg. pain source is from thumb but pain spreads to elbow)? Where does it radiate? Is it all in one place? Does it go anywhere else? Did it start elsewhere and now localised to one spot? Does it feel like it travels/moves around?
S = severity scale : How severe is the pain on a scale of 0 - 10, zero being no pain at all and 10 being the worst pain ever? Does it interfere with activities? How bad is it when it's at its worst? Does it force you to sit down, lie down, slow down? How long does an episode last?
T = timing : When did the pain start, at what time? How long did it last? How often does it occur? Is it sudden or gradual? What were you doing when you first experienced or noticed it? How often do you experience it: hourly? daily? weekly? monthly? When do you usually experience it: daytime? night? in the early morning? Are you ever awakened by it? Does it lead to anything else? Is it accompanied by other signs and symptoms? Does it ever occur before, during or after meals? Does it occur seasonally?
Other questions to ask when assessing a person in pain:
- Any medication or allergies?
- Does it hurt on deep inspiration?
- Activity at onset?
- Any history of pain?
- Is it the same?
- Different?
- Any family history of heart disease, lung problems, diabetes, stroke, hypertension?
- Check LOC
- Pupils?
- JVD?
- Midline trachea?
- Any recent trauma?
The purpose for these questions are to be as specific as possible in the description of the pain : when and where, what it feels like... The more specific and detailed information, the better it will be to diagnose the problem/cause and find a way to alleviate it.
References
- ↑ The mnemonic Socrates is used for these "dimensions of a painful complaint".
- ↑ IASP Pain Terminology.
- ↑ Krebs, Carey, and Weinberger, “Accuracy of the Pain Numeric Rating Scale as a Screening Test in Primary Care,” Journal of General Internal Medicine 22, no. 10 (October 21, 2007): 1453-1458, doi:10.1007/s11606-007-0321-2 (accessed September 28, 2007)
- ↑ Lord B, Woollard M (2011). "The reliability of vital signs in estimating pain severity among adult patients treated by paramedics". Emerg Med J. 28 (2): 147–50. doi:10.1136/emj.2009.079384. PMID 20926627.
- ↑ Todd KH, Funk KG, Funk JP, Bonacci R (1996). "Clinical significance of reported changes in pain severity". Ann Emerg Med. 27 (4): 485–9. PMID 8604867. Unknown parameter
|month=ignored (help) - ↑ Krebs EE, Lorenz KA, Bair MJ, Damush TM, Wu J, Sutherland JM; et al. (2009). "Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference". J Gen Intern Med. 24 (6): 733–8. doi:10.1007/s11606-009-0981-1. PMC 2686775. PMID 19418100.
- ↑ Melzack R (2005). "The McGill pain questionnaire: from description to measurement". Anesthesiology. 103 (1): 199–202. PMID 15983473.
- ↑ Other examples include headache while eating ice cream, toothache resulting from a strained upper back, foot soreness caused by a tumor in the uterus, and hip discomfort when the problem is really arthritis in the knee. These examples are taken from Nerves Tangle, and Back Pain Becomes a Toothache, by Kate Murphy, The New York Times, September 16, 2008.http://www.nytimes.com/2008/09/16/health/research/16pain.html?_r=1&pagewanted=print&oref=slogin