Norovirus infection epidemiology and demographics
|
Norovirus infection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Norovirus infection epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Norovirus infection epidemiology and demographics |
|
Norovirus infection epidemiology and demographics in the news |
|
Risk calculators and risk factors for Norovirus infection epidemiology and demographics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Anyone can become infected with these viruses. There are many different strains of norovirus, which makes it difficult for a person’s body to develop long-lasting immunity. Therefore, norovirus illness can recur throughout a person’s lifetime. In addition, because of differences in genetic factors, some people are more likely to become infected and develop more severe illness than others.
CDC currently does not conduct active surveillance to monitor outbreaks of gastroenteritis caused by noroviruses. Outbreaks are reported to CDC's Viral Gastroenteritis Section, Respiratory and Gastroenteric Viruses Branch, Division of Viral Diseases, National Center for Immunization and Respiratoiry Diseases (NCIRD) when states send specimens for testing or sequencing, or outbreaks are reported directly by states to the electronic database (eFORS) maintained by the Foodborne Diarrheal Diseases Branch.
Epidemiology and Demographics
Each year, norovirus causes about 21 million cases of acute gastroenteritis (inflammation of the stomach or intestines or both) and contributes to about 70,000 hospitalizations and 800 deaths, mostly among young children and the elderly. You can get norovirus illness at any time during the year. But, it is most common in the winter. Also, there can be 50% more norovirus illness in years when there is a new strain of the virus going around.
Outbreaks
Most outbreaks of norovirus illness happen when infected people spread the virus to others. But, norovirus can also spread by consuming contaminated food or water and touching things that have the virus on them. Healthcare facilities, including nursing homes and hospitals, are the most commonly reported places for norovirus outbreaks in the United States and other industrialized countries. Nearly two-thirds of all norovirus outbreaks reported in the United States occur in long-term care facilities. Outbreaks of norovirus illness have also occurred in restaurants, cruise ships, schools, banquet halls, summer camps, and even at family dinners. These are all places where people often eat food handled or prepared by others. In fact, norovirus is the leading cause of illness from contaminated food in the United States. About 50% of all outbreaks of food-related illness are caused by norovirus. Foods that are commonly involved in outbreaks of norovirus illness are:
- Leafy greens (such as lettuce),
- Fresh fruits, and
- Shellfish (such as oysters).
However, any food that is served raw or handled after being cooked can get contaminated. Norovirus outbreaks have also been caused by contaminated water from sewage in wells and recreational water, such as pools.
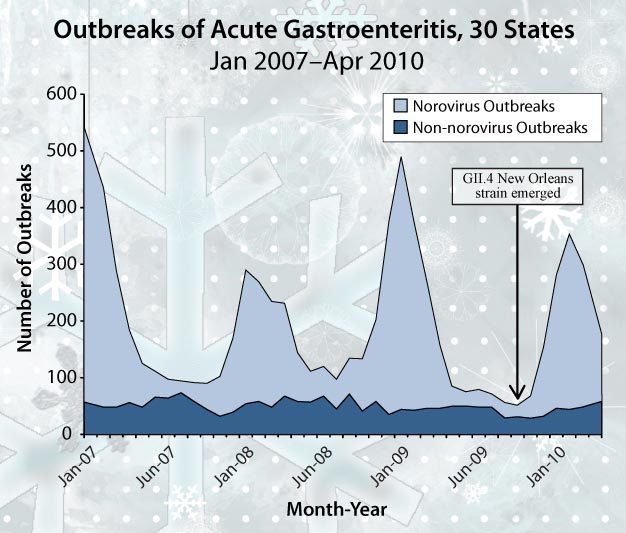
Shown below is a graph that illustrates outbreaks of acute gastroenteritis in 30 states from January 2007 through April 2010. On average, there were nearly 3 times as many norovirus outbreaks (143 per month) as non-norovirus outbreaks (50 per month) and the number of norovirus outbreaks increased dramatically during the winter months. A new virus strain (GII.4 New Orleans) that first appeared in October 2009 did not lead to more outbreaks.
Shown below is a graph that illustrates the setting of 1,518 confirmed norovirus outbreaks in the U.S. from 2010 to 2011: Long-term Care Facility 59% (889 Outbreaks); Restaurants 8% (123 Outbreaks); Party & Event 7% (99 Outbreaks); Hospital 4% (65 Outbreaks); School 4% (64 Outbreaks); Cruise Ship 4% (55 Outbreaks); Other & Unknown 14% (223 Outbreaks).
Epidemiologic criteria
Epidemiologic criteria have been proposed for use in determining whether an outbreak of gastroenteritis is of viral origin. Although quite specific, these criteria are not very sensitive, and therefore the possibility of a viral etiology should not be discarded if the criteria are not met. Kaplan's criteria for this purpose are as follows:
- A mean (or median) illness duration of 12 to 60 hours
- A mean (or median) incubation period of 24 to 48 hours
- More than 50% of people with vomiting
- No bacterial agent previously found