Modafinil
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Title
See full prescribing information for complete Boxed Warning.
ConditionName:
|
Overview
Modafinil is a that is FDA approved for the {{{indicationType}}} of . There is a Black Box Warning for this drug as shown here. Common adverse reactions include .
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition1
- Dosing Information
- Dosage
Condition2
- Dosing Information
- Dosage
Condition3
- Dosing Information
- Dosage
Condition4
- Dosing Information
- Dosage
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Modafinil in adult patients.
Non–Guideline-Supported Use
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Modafinil in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding FDA-Labeled Use of Modafinil in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Modafinil in pediatric patients.
Non–Guideline-Supported Use
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Modafinil in pediatric patients.
Contraindications
- Condition1
Warnings
|
Title
See full prescribing information for complete Boxed Warning.
ConditionName:
|
- Description
Precautions
- Description
Adverse Reactions
Clinical Trials Experience
There is limited information regarding Clinical Trial Experience of Modafinil in the drug label.
Body as a Whole
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Modafinil in the drug label.
Body as a Whole
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Drug Interactions
- Drug
- Description
Use in Specific Populations
Pregnancy
- Pregnancy Category
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Modafinil in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Modafinil during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Modafinil with respect to nursing mothers.
Pediatric Use
There is no FDA guidance on the use of Modafinil with respect to pediatric patients.
Geriatic Use
There is no FDA guidance on the use of Modafinil with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Modafinil with respect to specific gender populations.
Race
There is no FDA guidance on the use of Modafinil with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Modafinil in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Modafinil in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Modafinil in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Modafinil in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
- Intravenous
Monitoring
There is limited information regarding Monitoring of Modafinil in the drug label.
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Modafinil in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Description
Management
- Description
Chronic Overdose
There is limited information regarding Chronic Overdose of Modafinil in the drug label.
Pharmacology
There is limited information regarding Modafinil Pharmacology in the drug label.
Mechanism of Action
- The precise mechanism(s) through which modafinil promotes wakefulness is unknown. Modafinil has wake-promoting actions similar to sympathomimetic agents like amphetamine and methylphenidate, although the pharmacologic profile is not identical to that of sympathomimetic amines.
- Modafinil has weak to negligible interactions with receptors for norepinephrine, serotonin, dopamine, GABA, adenosine, histamine-3, melatonin, and benzodiazepines. Modafinil also does not inhibit the activities of MAO-B or phosphodiesterases II-V.
- Modafinil-induced wakefulness can be attenuated by the α1-adrenergic receptor antagonist prazosin; however, modafinil is inactive in other in vitro assay systems known to be responsive to α-adrenergic agonists, such as the rat vas deferens preparation.
- Modafinil is not a direct- or indirect-acting dopamine receptor agonist. However, in vitro, modafinil binds to the dopamine transporter and inhibits dopamine reuptake. This activity has been associated in vivo with increased extracellular dopamine levels in some brain regions of animals. In genetically engineered mice lacking the dopamine transporter (DAT), modafinil lacked wake-promoting activity, suggesting that this activity was DAT-dependent. However, the wake-promoting effects of modafinil, unlike those of amphetamine, were not antagonized by the dopamine receptor antagonist haloperidol in rats. In addition, alpha-methyl-p-tyrosine, a dopamine synthesis inhibitor, blocks the action of amphetamine, but does not block locomotor activity induced by modafinil.
- In the cat, equal wakefulness-promoting doses of methylphenidate and amphetamine increased neuronal activation throughout the brain. Modafinil at an equivalent wakefulness-promoting dose selectively and prominently increased neuronal activation in more discrete regions of the brain. The relationship of this finding in cats to the effects of modafinil in humans is unknown.
- In addition to its wake-promoting effects and ability to increase locomotor activity in animals, modafinil produces psychoactive and euphoric effects, alterations in mood, perception, thinking, and feelings typical of other CNS stimulants in humans. Modafinil has reinforcing properties, as evidenced by its self-administration in monkeys previously trained to self-administer cocaine. Modafinil was also partially discriminated as stimulant-like.
- The optical enantiomers of modafinil have similar pharmacological actions in animals. Two major metabolites of modafinil, modafinil acid and modafinil sulfone, do not appear to contribute to the CNS-activating properties of modafinil.
Structure
- Modafinil is a wakefulness-promoting agent for oral administration. Modafinil is a racemic compound. The chemical name for modafinil is 2-[(diphenylmethyl)sulfinyl]acetamide. The molecular formula is C15H15NO2S and the molecular weight is 273.35.
- The chemical structure is:
- Modafinil is a white to off-white, crystalline powder that is practically insoluble in water and cyclohexane. It is sparingly to slightly soluble in methanol and acetone. Modafinil tablets contain 100 mg or 200 mg of modafinil and the following inactive ingredients: Lactose Monohydrate, Corn Starch dried, Crospovidone , Croscarmellose Sodium, Colloidal Silicon Dioxide, Magnesium Stearate, and Talc.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Modafinil in the drug label.
Pharmacokinetics
- Modafinil is a racemic compound, whose enantiomers have different pharmacokinetics (e.g., the half-life of the l-isomer is approximately three times that of the d-isomer in adult humans). The enantiomers do not interconvert. At steady state, total exposure to the l-isomer is approximately three times that for the d-isomer. The trough concentration (Cminss) of circulating modafinil after once daily dosing consists of 90% of the l-isomer and 10% of the d-isomer. The effective elimination half-life of modafinil after multiple doses is about 15 hours. The enantiomers of modafinil exhibit linear kinetics upon multiple dosing of 200 to 600 mg/day once daily in healthy volunteers. Apparent steady states of total modafinil and l-(-)-modafinil are reached after 2-4 days of dosing.
- Absorption
- Absorption of modafinil tablets is rapid, with peak plasma concentrations occurring at 2-4 hours. The bioavailability of modafinil tablets is approximately equal to that of an aqueous suspension. The absolute oral bioavailability was not determined due to the aqueous insolubility (<1 mg/mL) of modafinil, which precluded intravenous administration. Food has no effect on overall modafinil bioavailability; however, its absorption (tmax) may be delayed by approximately one hour if taken with food.
- Distribution
- Modafinil is well distributed in body tissue with an apparent volume of distribution (~0.9 L/kg) larger than the volume of total body water (0.6 L/kg). In human plasma, in vitro, modafinil is moderately bound to plasma protein (~60%, mainly to albumin). At serum concentrations obtained at steady state after doses of 200 mg/day, modafinil exhibits no displacement of protein binding of warfarin, diazepam or propranolol. Even at much larger concentrations (1000 μM; > 25 times the Cmax of 40 μM at steady state at 400 mg/day), modafinil has no effect on warfarin binding. Modafinil acid at concentrations >500 μM decreases the extent of warfarin binding, but these concentrations are >35 times those achieved therapeutically.
- Metabolism and Elimination
- The major route of elimination is metabolism (~90%), primarily by the liver, with subsequent renal elimination of the metabolites. Urine alkalinization has no effect on the elimination of modafinil.
- Metabolism occurs through hydrolytic deamidation, S-oxidation, aromatic ring hydroxylation, and glucuronide conjugation. Less than 10% of an administered dose is excreted as the parent compound. In a clinical study using radiolabeled modafinil, a total of 81% of the administered radioactivity was recovered in 11 days post-dose, predominantly in the urine (80% vs. 1% in the feces). The largest fraction of the drug in urine was modafinil acid, but at least six other metabolites were present in lower concentrations. Only two metabolites reach appreciable concentrations in plasma, i.e., modafinil acid and modafinil sulfone. In preclinical models, modafinil acid, modafinil sulfone, 2-[(diphenylmethyl)sulfonyl]acetic acid and 4-hydroxy modafinil, were inactive or did not appear to mediate the arousal effects of modafinil.
- In adults, decreases in trough levels of modafinil have sometimes been observed after multiple weeks of dosing, suggesting auto-induction, but the magnitude of the decreases and the inconsistency of their occurrence suggest that their clinical significance is minimal. Significant accumulation of modafinil sulfone has been observed after multiple doses due to its long elimination half-life of 40 hours. Induction of metabolizing enzymes, most importantly cytochrome P-450 (CYP) 3A4, has also been observed in vitro after incubation of primary cultures of human hepatocytes with modafinil and in vivo after extended administration of modafinil at 400 mg/day. (For further discussion of the effects of modafinil on CYP enzyme activities, see PRECAUTIONS, Drug Interactions.)
- Drug-Drug Interactions: Based on in vitro data, modafinil is metabolized partially by the 3A isoform subfamily of hepatic cytochrome P450 (CYP3A4). In addition, modafinil has the potential to inhibit CYP2C19, suppress CYP2C9, and induce CYP3A4, CYP2B6, and CYP1A2. Because modafinil and modafinil sulfone are reversible inhibitors of the drug-metabolizing enzyme CYP2C19, coadministration of modafinil with drugs such as diazepam, phenytoin and propranolol, which are largely eliminated via that pathway, may increase the circulating levels of those compounds. In addition, in individuals deficient in the enzyme CYP2D6 (i.e., 7-10% of the Caucasian population; similar or lower in other populations), the levels of CYP2D6 substrates such as tricyclic antidepressants and selective serotonin reuptake inhibitors, which have ancillary routes of elimination through CYP2C19, may be increased by coadministration of modafinil. Dose adjustments may be necessary for patients being treated with these and similar medications (See PRECAUTIONS, Drug Interactions). An in vitro study demonstrated that armodafinil (one of the enantiomers of modafinil) is a substrate of P-glycoprotein.
- Coadministration of modafinil with other CNS active drugs such as methylphenidate and dextroamphetamine did not significantly alter the pharmacokinetics of either drug.
- Chronic administration of modafinil 400 mg was found to decrease the systemic exposure to two CYP3A4 substrates, ethinyl estradiol and triazolam, after oral administration suggesting that CYP3A4 had been induced. Chronic administration of modafinil can increase the elimination of substrates of CYP3A4. Dose adjustments may be necessary for patients being treated with these and similar medications (See PRECAUTIONS, Drug Interactions).
- An apparent concentration-related suppression of CYP2C9 activity was observed in human hepatocytes after exposure to modafinil in vitro suggesting that there is a potential for a metabolic interaction between modafinil and the substrates of this enzyme (e.g., S-warfarin, phenytoin). However, in an interaction study in healthy volunteers, chronic modafinil treatment did not show a significant effect on the pharmacokinetics of warfarin when compared to placebo. (See PRECAUTIONS, Drug Interactions, Other Drugs, Warfarin).
- Special Populations
- Gender Effect: The pharmacokinetics of modafinil are not affected by gender.
- Age Effect: A slight decrease (~20%) in the oral clearance (CL/F) of modafinil was observed in a single dose study at 200 mg in 12 subjects with a mean age of 63 years (range 53 – 72 years), but the change was considered not likely to be clinically significant. In a multiple dose study (300 mg/day) in 12 patients with a mean age of 82 years (range 67 – 87 years), the mean levels of modafinil in plasma were approximately two times those historically obtained in matched younger subjects. Due to potential effects from the multiple concomitant medications with which most of the patients were being treated, the apparent difference in modafinil pharmacokinetics may not be attributable solely to the effects of aging. However, the results suggest that the clearance of modafinil may be reduced in the elderly (See DOSAGE AND ADMINISTRATION).
- Race Effect: The influence of race on the pharmacokinetics of modafinil has not been studied.
- Renal Impairment: In a single dose 200 mg modafinil study, severe chronic renal failure (creatinine clearance ≤ 20 mL/min) did not significantly influence the pharmacokinetics of modafinil, but exposure to modafinil acid (an inactive metabolite) was increased 9-fold (See PRECAUTIONS).
- Hepatic Impairment: Pharmacokinetics and metabolism were examined in patients with cirrhosis of the liver (6 males and 3 females). Three patients had stage B or B+ cirrhosis (per the Child criteria) and 6 patients had stage C or C+ cirrhosis. Clinically 8 of 9 patients were icteric and all had ascites. In these patients, the oral clearance of modafinil was decreased by about 60% and the steady state concentration was doubled compared to normal patients. The dose of modafinil should be reduced in patients with severe hepatic impairment (See PRECAUTION
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Modafinil in the drug label.
Clinical Studies
- The effectiveness of modafinil in reducing excessive sleepiness has been established in the following sleep disorders: narcolepsy, obstructive sleep apnea (OSA), and shift work disorder (SWD).
Narcolepsy
- The effectiveness of modafinil in reducing the excessive sleepiness (ES) associated with narcolepsy was established in two U.S. 9-week, multicenter, placebo-controlled, two-dose (200 mg per day and 400 mg per day) parallel-group, double-blind studies of outpatients who met the ICD-9 and American Sleep Disorders Association criteria for narcolepsy (which are also consistent with the American Psychiatric Association DSM-IV criteria). These criteria include either 1) recurrent daytime naps or lapses into sleep that occur almost daily for at least three months, plus sudden bilateral loss of postural muscle tone in association with intense emotion (cataplexy) or 2) a complaint of excessive sleepiness or sudden muscle weakness with associated features: sleep paralysis, hypnagogic hallucinations, automatic behaviors, disrupted major sleep episode; and polysomnography demonstrating one of the following: sleep latency less than 10 minutes or rapid eye movement (REM) sleep latency less than 20 minutes. In addition, for entry into these studies, all patients were required to have objectively documented excessive daytime sleepiness, a Multiple Sleep Latency Test (MSLT) with two or more sleep onset REM periods, and the absence of any other clinically significant active medical or psychiatric disorder. The MSLT, an objective daytime polysomnographic assessment of the patient's ability to fall asleep in an unstimulating environment, measures latency (in minutes) to sleep onset averaged over 4 test sessions at 2-hour intervals following nocturnal polysomnography. For each test session, the subject was told to lie quietly and attempt to sleep. Each test session was terminated after 20 minutes if no sleep occurred or 15 minutes after sleep onset.
- In both studies, the primary measures of effectiveness were 1) sleep latency, as assessed by the Maintenance of Wakefulness Test (MWT) and 2) the change in the patient's overall disease status, as measured by the Clinical Global Impression of Change (CGI-C). For a successful trial, both measures had to show significant improvement.
- The MWT measures latency (in minutes) to sleep onset averaged over 4 test sessions at 2 hour intervals following nocturnal polysomnography. For each test session, the subject was asked to attempt to remain awake without using extraordinary measures. Each test session was terminated after 20 minutes if no sleep occurred or 10 minutes after sleep onset. The CGI-C is a 7-point scale, centered at No Change, and ranging from Very Much Worse to Very Much Improved. Patients were rated by evaluators who had no access to any data about the patients other than a measure of their baseline severity. Evaluators were not given any specific guidance about the criteria they were to apply when rating patients.
- Other assessments of effect included the Multiple Sleep Latency Test (MSLT), Epworth Sleepiness Scale (ESS; a series of questions designed to assess the degree of sleepiness in everyday situations), the Steer Clear Performance Test (SCPT; a computer-based evaluation of a patient's ability to avoid hitting obstacles in a simulated driving situation), standard nocturnal polysomnography, and patient's daily sleep log. Patients were also assessed with the Quality of Life in Narcolepsy (QOLIN) scale, which contains the validated SF-36 health questionnaire.
- Both studies demonstrated improvement in objective and subjective measures of excessive daytime sleepiness for both the 200 mg and 400 mg doses compared to placebo. Patients treated with either dose of modafinil showed a statistically significantly enhanced ability to remain awake on the MWT (all p values <0.001) at weeks 3, 6, 9, and final visit compared to placebo and a statistically significantly greater global improvement, as rated on the CGI-C scale (all p values <0.05).
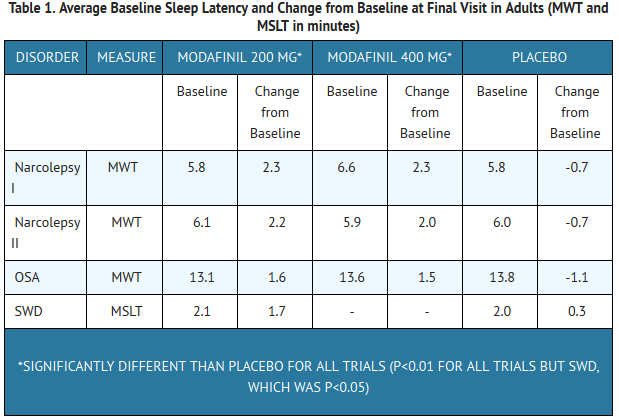
- The average sleep latencies (in minutes) on the MWT at baseline for the 2 controlled trials are shown in Table 1 below, along with the average change from baseline on the MWT at final visit.
- The percentages of patients who showed any degree of improvement on the CGI-C in the two clinical trials are shown in Table 2 below.
- Similar statistically significant treatment-related improvements were seen on other measures of impairment in narcolepsy, including a patient assessed level of daytime sleepiness on the ESS (p<0.001 for each dose in comparison to placebo).
- Nighttime sleep measured with polysomnography was not affected by the use of modafinil.
Obstructive Sleep Apnea (OSA)
- The effectiveness of modafinil in reducing the excessive sleepiness associated with OSA was established in two clinical trials. In both studies, patients were enrolled who met the International Classification of Sleep Disorders (ICSD) criteria for OSA (which are also consistent with the American Psychiatric Association DSM-IV criteria). These criteria include either, 1) excessive sleepiness or insomnia, plus frequent episodes of impaired breathing during sleep, and associated features such as loud snoring, morning headaches and dry mouth upon awakening; or 2) excessive sleepiness or insomnia and polysomnography demonstrating one of the following: more than five obstructive apneas, each greater than 10 seconds in duration, per hour of sleep and one or more of the following: frequent arousals from sleep associated with the apneas, bradytachycardia, and arterial oxygen desaturation in association with the apneas. In addition, for entry into these studies, all patients were required to have excessive sleepiness as demonstrated by a score ≥10 on the Epworth Sleepiness Scale, despite treatment with continuous positive airway pressure (CPAP). Evidence that CPAP was effective in reducing episodes of apnea/hypopnea was required along with documentation of CPAP use.
- In the first study, a 12-week multicenter placebo-controlled trial, a total of 327 patients were randomized to receive modafinil 200 mg/day, modafinil 400 mg/day, or matching placebo. The majority of patients (80%) were fully compliant with CPAP, defined as CPAP use > 4 hours/night on > 70% nights. The remainder were partially CPAP compliant, defined as CPAP use < 4 hours/night on >30% nights. CPAP use continued throughout the study. The primary measures of effectiveness were 1) sleep latency, as assessed by the Maintenance of Wakefulness Test (MWT) and 2) the change in the patient's overall disease status, as measured by the Clinical Global Impression of Change (CGI-C) at week 12 or the final visit. (See CLINICAL TRIALS, Narcolepsy section above for a description of these tests.)
- Patients treated with modafinil showed a statistically significant improvement in the ability to remain awake compared to placebo-treated patients as measured by the MWT (p<0.001) at endpoint [Table 1]. Modafinil -treated patients also showed a statistically significant improvement in clinical condition as rated by the CGI-C scale (p<0.001) [Table 2]. The two doses of modafinil performed similarly.
- In the second study, a 4-week multicenter placebo-controlled trial, 157 patients were randomized to either modafinil 400 mg/day or placebo. Documentation of regular CPAP use (at least 4 hours/night on 70% of nights) was required for all patients. The primary outcome measure was the change from baseline on the ESS at week 4 or final visit. The baseline ESS scores for the modafinil and placebo groups were 14.2 and 14.4, respectively. At week 4, the ESS was reduced by 4.6 in the modafinil group and by 2.0 in the placebo group, a difference that was statistically significant (p<0.0001).
- Nighttime sleep measured with polysomnography was not affected by the use of modafinil.
Shift Work Disorder (SWD)
- The effectiveness of modafinil for the excessive sleepiness associated with SWD was demonstrated in a 12-week placebo-controlled clinical trial. A total of 209 patients with chronic SWD were randomized to receive modafinil 200 mg/day or placebo. All patients met the International Classification of Sleep Disorders (ICSD-10) criteria for chronic SWD (which are consistent with the American Psychiatric Association DSM-IV criteria for Circadian Rhythm Sleep Disorder: Shift Work Type). These criteria include 1) either: a) a primary complaint of excessive sleepiness or insomnia which is temporally associated with a work period (usually night work) that occurs during the habitual sleep phase, or b) polysomnography and the MSLT demonstrate loss of a normal sleep-wake pattern (i.e., disturbed chronobiological rhythmicity); and 2) no other medical or mental disorder accounts for the symptoms, and 3) the symptoms do not meet criteria for any other sleep disorder producing insomnia or excessive sleepiness (e.g., time zone change [jet lag] syndrome).
- It should be noted that not all patients with a complaint of sleepiness who are also engaged in shift work meet the criteria for the diagnosis of SWD. In the clinical trial, only patients who were symptomatic for at least 3 months were enrolled.
- Enrolled patients were also required to work a minimum of 5 night shifts per month, have excessive sleepiness at the time of their night shifts (MSLT score < 6 minutes), and have daytime insomnia documented by a daytime polysomnogram (PSG).
- The primary measures of effectiveness were 1) sleep latency, as assessed by the Multiple Sleep Latency Test (MSLT) performed during a simulated night shift at week 12 or the final visit and 2) the change in the patient's overall disease status, as measured by the Clinical Global Impression of Change (CGI-C) at week 12 or the final visit. Patients treated with modafinil showed a statistically significant prolongation in the time to sleep onset compared to placebo-treated patients, as measured by the nighttime MSLT [Table 1] (p<0.05). Improvement on the CGI-C was also observed to be statistically significant (p<0.001). (See CLINICAL TRIALS, Narcolepsy section above for a description of these tests.)
- Daytime sleep measured with polysomnography was not affected by the use of modafinil.
T1
T2
How Supplied
Storage
There is limited information regarding Modafinil Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Modafinil |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Modafinil |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Modafinil in the drug label.
Precautions with Alcohol
- Alcohol-Modafinil interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- ®[1]
Look-Alike Drug Names
- A® — B®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Empty citation (help)
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Modafinil |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Modafinil |Label Name=Modafinil11.png
}}
{{#subobject:
|Label Page=Modafinil |Label Name=Modafinil11.png
}}