Mitral regurgitation overview: Difference between revisions
m (Robot: Changing Category:Disease state to Category:Disease) |
Varun Kumar (talk | contribs) No edit summary |
||
| Line 6: | Line 6: | ||
After age 55, some degree of mitral regurgitation is found in almost 20% of men and women who have an echocardiogram. | After age 55, some degree of mitral regurgitation is found in almost 20% of men and women who have an echocardiogram. | ||
[[Image:Mitral Regurgitation.png|thumb|left|200px|'''Mitral regurgitation (schematic drawing)'''<br/>During systole, contraction of the left ventricle causes abnormal backflow (arrow) into the left atrium.<br/>1 [[Mitral valve]]<br/>2 [[Left Ventricle]]<br/>3 [[Left Atrium]]<br/>4 [[Aorta]]]] | [[Image:Mitral Regurgitation.png|thumb|left|200px|'''Mitral regurgitation (schematic drawing)'''<br/>During systole, contraction of the left ventricle causes abnormal backflow (arrow) into the left atrium.<br/>1 [[Mitral valve]]<br/>2 [[Left Ventricle]]<br/>3 [[Left Atrium]]<br/>4 [[Aorta]]]] | ||
==Anatomy== | |||
The mitral valve is typically 4–6 cm² in area. It has two cusps, or leaflets (the anteromedial leaflet and the posterolateral leaflet). | |||
==Pathophysiology== | |||
Mitral regurgitation is due to either perforation or prolapse of the leaflets, dilation of the mitral annulus or rupture of the papillary muscles or chordae tendineae. There are several phases of mitral regurgitation (acute, chronic compensated, and chronic decompensated). In the acute phase, the volume and pressure overload in the left atrium is transmitted backward into the pulmonary vasculature to cause an elevation of the [[pulomanry capillary wedge pressure]] which causes [[dyspnea]], [[PND]], [[orthopnea]] and [[rales]]. During the chronic compensated phase of mitral regurgitation, the left ventricle maintains forward [[cardiac output]] by filling with a larger volume of blood than usual to accomodate the fact that a portion of the blood will go backwards into the left atrium. In the decompensated phase, the left ventricle begins to dilate and fail. The markers of decompensation are as follows: | |||
# '''Left ventricular end-diastolic dimension greater than 70 mm''' | |||
# '''Left ventricular end-systolic dimension greater than 45 to 47 mm''' | |||
# '''Left ventricular [[ejection fraction]] (LVEF) less than 50 to 55 percent''' | |||
==References== | ==References== | ||
Revision as of 01:20, 16 April 2012
|
Mitral Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mitral regurgitation overview On the Web |
|
American Roentgen Ray Society Images of Mitral regurgitation overview |
|
Risk calculators and risk factors for Mitral regurgitation overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S; Mohammed A. Sbeih, M.D. [3].
Overview
Mitral regurgitation (MR), mitral insufficiency or mitral incompetence is a disorder of the heart in which the mitral valve does not close properly when the heart pumps out blood. It is the abnormal leaking of blood from the left ventricle, through the mitral valve, and into the left atrium, when the left ventricle contracts, i.e. there is regurgitation of blood back into the left atrium [1]. MR is the most common form of valvular heart disease [2]. Diseases that weaken or damage the valve or the heart tissue around the valve cause mitral regurgitation. After age 55, some degree of mitral regurgitation is found in almost 20% of men and women who have an echocardiogram.
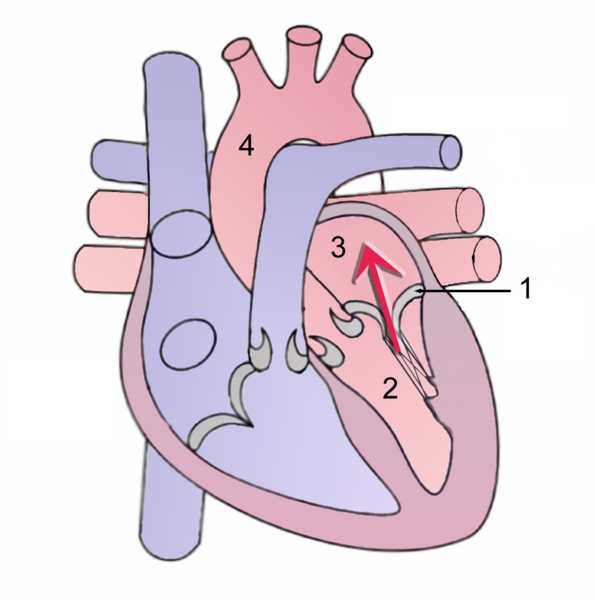
During systole, contraction of the left ventricle causes abnormal backflow (arrow) into the left atrium.
1 Mitral valve
2 Left Ventricle
3 Left Atrium
4 Aorta
Anatomy
The mitral valve is typically 4–6 cm² in area. It has two cusps, or leaflets (the anteromedial leaflet and the posterolateral leaflet).
Pathophysiology
Mitral regurgitation is due to either perforation or prolapse of the leaflets, dilation of the mitral annulus or rupture of the papillary muscles or chordae tendineae. There are several phases of mitral regurgitation (acute, chronic compensated, and chronic decompensated). In the acute phase, the volume and pressure overload in the left atrium is transmitted backward into the pulmonary vasculature to cause an elevation of the pulomanry capillary wedge pressure which causes dyspnea, PND, orthopnea and rales. During the chronic compensated phase of mitral regurgitation, the left ventricle maintains forward cardiac output by filling with a larger volume of blood than usual to accomodate the fact that a portion of the blood will go backwards into the left atrium. In the decompensated phase, the left ventricle begins to dilate and fail. The markers of decompensation are as follows:
- Left ventricular end-diastolic dimension greater than 70 mm
- Left ventricular end-systolic dimension greater than 45 to 47 mm
- Left ventricular ejection fraction (LVEF) less than 50 to 55 percent
References
- ↑ Mitral valve regurgitation at Mount Sinai Hospital
- ↑ Weinrauch, LA (2008-05-12). "Mitral regurgitation - chronic". Medline Plus Encyclopedia. U.S. National Library of Medicine and National Institutes of Health. Retrieved 2009-12-04.