Midostaurin
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sonya Gelfand
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Midostaurin is a kinase inhibitor that is FDA approved for the treatment of newly diagnosed acute myeloid leukemia (AML) that is FLT3 mutation-positive as detected by an FDA-approved test, in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation, aggressive systemic mastocytosis (ASM), systemic mastocytosis with associated hematological neoplasm (SM-AHN), or mast cell leukemia (MCL). Common adverse reactions include (AML) ebrile neutropenia, nausea, mucositis, vomiting, headache, petechiae, musculoskeletal pain, epistaxis, device-related infection, hyperglycemia, and upper respiratory tract infection, or (ASM, SM-AHN, or MCL) nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, constipation, pyrexia, headache, and dyspnea.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Acute Myeloid Leukemia
- Midostaurin is indicated, in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation chemotherapy, for the treatment of adult patients with newly diagnosed acute myeloid leukemia (AML) who are FLT3 mutation-positive, as detected by a FDA approved test.
Limitations of Use
- Midostaurin is not indicated as a single-agent induction therapy for the treatment of patients with AML.
Systemic Mastocytosis
- Midostaurin is indicated for the treatment of adult patients with aggressive systemic mastocytosis (ASM), systemic mastocytosis with associated hematological neoplasm (SM-AHN), or mast cell leukemia (MCL).
Patient Selection
- Select patients for the treatment of AML with midostaurin based on the presence of FLT3 mutation positivity. Information on FDA-approved tests for the detection of FLT3 mutation in AML is available at: http://www.fda.gov/CompanionDiagnostics.
Recommended Dosage in Acute Myeloid Leukemia
- The recommended dose of midostaurin for patients with acute myeloid leukemia is 50 mg orally twice daily with food on Days 8 to 21 of each cycle of induction with cytarabine and daunorubicin and on Days 8 to 21 of each cycle of consolidation with high-dose cytarabine. For a description of the experience with single-agent treatment with midostaurin beyond induction and consolidation.
Recommended Dosage in ASM, SM-AHN, and MCL
- The recommended dose of midostaurin for patients with ASM, SM-AHN, and MCL is 100 mg orally twice daily with food. Continue treatment until disease progression or unacceptable toxicity occurs. Table 1 provides recommendations for dose modifications of midostaurin in patients with ASM, SM-AHN, and MCL. Monitor patients for toxicity at least weekly for the first 4 weeks, every other week for the next 8 weeks, and monthly thereafter while on treatment.

Recommended Administration
- Administer prophylactic anti-emetics before treatment with midostaurin to reduce the risk of nausea and vomiting.
- Administer midostaurin orally with food, twice daily at approximately 12 hour intervals. Do not open or crush midostaurin capsules.
- If a dose of midostaurin is missed or vomited, do not make up the dose; take the next dose at the usual scheduled time.
- Consider interval assessments of QT by EKG if midostaurin is taken concurrently with medications that can prolong the QT interval.
Dosage Forms and Strengths
- 25 mg capsules: pale orange oblong soft capsule with red ink imprint ‘PKC NVR’.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding midostaurin Off-Label NGuideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding midostaurin Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Midostaurin FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding midostaurin Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding midostaurin Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Midostaurin is contraindicated in patients with hypersensitivity to midostaurin or to any of the excipients. Hypersensitivity reactions have included anaphylactic shock, dyspnea, flushing, chest pain, and angioedema (e.g., swelling of the airways or tongue, with or without respiratory impairment).
Warnings
Embryo-Fetal Toxicity
- Based on its mechanism of action and findings from animal reproduction studies, midostaurin may cause fetal harm when administered to pregnant women. In animal studies, midostaurin caused embryo-fetal toxicities, including late embryo-fetal death and reduced fetal birth weight, with delays in fetal growth at doses lower than the recommended human dose. Advise pregnant women of the potential risk to the fetus. Verify the pregnancy status of females of reproductive potential within 7 days prior to initiating midostaurin therapy. Advise females of reproductive potential to use effective contraception during treatment with midostaurin and for at least 4 months after the last dose. Advise males with female partners to use effective contraception during treatment with midostaurin and for 4 months after the last dose.
Pulmonary Toxicity
- Cases of interstitial lung disease and pneumonitis, some fatal, have occurred in patients treated with midostaurin as monotherapy or with chemotherapy. Monitor patients for pulmonary symptoms. Discontinue midostaurin in patients who experience signs or symptoms of interstitial lung disease or pneumonitis without an infectious etiology.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Acute Myeloid Leukemia
- The safety evaluation of midostaurin (50 mg twice daily with food) in patients with newly diagnosed FLT3 mutated AML is based on a randomized, double-blind, trial of midostaurin (n = 345) or placebo (n = 335) with chemotherapy. The overall median duration of exposure was 42 days (range 2 to 576 days) for patients in the midostaurin plus chemotherapy arm versus 34 days (range 1 to 465 days) for patients in the placebo plus chemotherapy arm. On the midostaurin plus chemotherapy arm, 35% of patients completed induction and consolidation therapy, compared to 25% of patients on the placebo plus chemotherapy arm.
- The most frequent (incidence greater than or equal to 20%) adverse drug reactions (ADRs) in the midostaurin plus chemotherapy arm were febrile neutropenia, nausea, mucositis, vomiting, headache, petechiae, musculoskeletal pain, epistaxis, device-related infection, hyperglycemia, and upper respiratory tract infections. The most frequent Grade 3/4 adverse reactions (incidence greater than or equal to 10%) were febrile neutropenia, device-related infection and mucositis.
- The most frequent serious adverse reaction (≥ 10%) in patients in the midostaurin plus chemotherapy arm was febrile neutropenia (16%), which occurred at a similar rate in the placebo arm (16%).
- Discontinuation due to any adverse reaction occurred in 9% of patients in the midostaurin arm versus 6% in the placebo arm. The most frequent (> 1%) Grade 3/4 adverse reactions leading to discontinuation in the midostaurin arm was renal insufficiency (1%).
- Excluding deaths due to disease progression, no fatal adverse reactions occurred in the study. Overall, the most frequent non-treatment related cause of death in the midostaurin plus chemotherapy arm was sepsis (2%) and occurred at a similar rate in the placebo arm (2%).
- Table 2 presents the frequency category of adverse reactions reported in the randomized trial in patients with newly diagnosed FLT3 mutated AML. Adverse reactions are listed according to body system. Within each body system, the adverse reactions are ranked by frequency, with the most frequent reactions first. Table 3 presents the key laboratory abnormalities from the same randomized trial in patients with newly diagnosed FLT3 mutated AML.

- Other notable adverse reactions occurring in less than 10% of patients treated with midostaurin but at least 2% more frequently than in the placebo group included:
- Infections and infestations: Cellulitisa (7%), fungal infectiona (7%)
- Metabolism and nutrition disorders: Hyperuricemia (8%)
- Nervous system disorders: Tremor (4%)
- Eye disorders: Eyelid edema (3%)
- Cardiac disorders: Hypertensiona (8%), pericardial effusion (4%)
- Respiratory, thoracic and mediastinal disorders: pleural effusion (6%)
- Skin and subcutaneous tissue disorders: Dry skin (7%)
- General disorders and administration site conditions: Thrombosisa (5%)
- Investigations: Weight increased (7%), hypercalcemia (3%)
- abased on grouping of individual PTs:
- Thrombosis: e.g., thrombosis in device, thrombosis
- Cellulitis: e.g., cellulitis, erysipelas
- Fungal infection: e.g., Bronchopulmonary aspergillosis, pneumonia fungal, splenic infection fungal, hepatic candidiasis

- In Study 1, 205 patients (120 in midostaurin arm and 85 in placebo arm) who remained in remission following completion of consolidation continued to receive either single agent midostaurin or placebo for a median of 11 months (range 0.5 to 17 months) with 69 in the midostaurin arm and 51 in the placebo completing 12 treatment cycles. Common adverse reactions (greater than or equal to 5% difference between the midostaurin and placebo arms) reported for these patients included nausea (47% vs. 18%), hyperglycemia (20% vs. 13%) and vomiting (19% vs. 5%).
Systemic Mastocytosis
- Two single-arm, open-label multicenter trials (Study 2 and Study 3) evaluated the safety of midostaurin (100 mg twice daily with food) as a single agent in 142 adult patients total with ASM, SM-AHN, or MCL. The median age was 63 (range: 24 to 82), 63% had an ECOG performance status of 0 or 1, and 75% had no hepatic impairment (bilirubin and AST ≤ ULN) at baseline. The median duration of exposure to midostaurin was 11.4 months (range: 0 to 81 months), with 34% treated for ≥ 24 months.
- The most frequent adverse reactions (≥ 20%), excluding laboratory terms, were nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, constipation, pyrexia, headache, and dyspnea (Table 4). Grade ≥ 3 adverse reactions reported in ≥ 5%, excluding laboratory terms, were fatigue, sepsis, gastrointestinal hemorrhage, pneumonia, diarrhea, febrile neutropenia, edema, dyspnea, nausea, vomiting, abdominal pain, and renal insufficiency (Table 4).
- Adverse reactions led to dose modifications (interruption or reduction) in 56% of patients. Among these, the most frequent adverse reactions (> 5%) were gastrointestinal symptoms, QT prolongation, neutropenia, pyrexia, thrombocytopenia, gastrointestinal hemorrhage, lipase increase, and fatigue. The median time to first dose modification for toxicity was 1.6 months, with 75% of dose modifications first occurring within 5 months of starting treatment.
- Treatment discontinuation due to adverse reactions occurred in 21% of patients. The most frequent adverse reactions causing treatment discontinuation included infection, nausea or vomiting, QT prolongation, and gastrointestinal hemorrhage.
- Serious adverse reactions were reported in 68% of patients, most commonly (≥ 20%) due to infections and gastrointestinal disorders.
- On-treatment deaths unrelated to the underlying malignancy occurred in 16 patients (11%), most commonly from infection (sepsis or pneumonia), followed by cardiac events. Of the on-treatment deaths from disease progression, 4 were also attributable to infection.
- Table 4 summarizes the adverse reactions reported in ≥ 10% of the patients with advanced SM.

- Gastrointestinal Toxicities Leading to Treatment Modification:
- In patients with advanced SM, the median time to onset of nausea was 9 days, with 75% of cases beginning within the first 3 months. The median time to onset of vomiting was 1 month.
- Other clinically significant adverse reactions occurring in ≤ 10% of patients included:
- Infections and infestations: Sepsis (9%)a, bronchitis (6%), cellulitis or erysipelas (5%)
- Blood and lymphatic system disorders: Febrile neutropenia (8%)
- Cardiac disorders: Cardiac failure (6%), myocardial infarction or ischemia (4%)a
- Immune system disorders: Hypersensitivity (4%)a
- Nervous system disorders: Disturbance in attention (7%), tremor (6%), mental status changes (4%)
- Ear and labyrinth disorders: Vertigo (5%)
- Vascular disorders: Hypotension (9%), hematoma (6%)
- Respiratory, thoracic and mediastinal disorders: Oropharyngeal pain (4%), interstitial lung disease or pneumonitis (2%), pulmonary edema (3%)a
- Gastrointestinal disorders: Dyspepsia (6%), gastritis (3%)a
- General disorders and administration site conditions: Chills (5%)
- Investigations: Weight increased (6%)
- Injury, poisoning and procedural complications: Contusion (6%)
- aGrouped terms
- Sepsis: e.g., sepsis, staphylococcal/Enterobacter/Escherichia sepsis
- Hypersensitivity: includes one report of anaphylactic shock
- Myocardial infarction or ischemia: e.g., myocardial infarction and acute myocardial infarction, angina pectoris
- Gastritis: gastritis, gastritis erosive, gastritis hemorrhagic
- Pulmonary edema: pulmonary edema, pulmonary congestion
- Table 5 summarizes new or worsening laboratory abnormalities. Common (≥ 10%) Grade 3 or higher non-hematologic laboratory abnormalities were hyperglycemia (non-fasting), lipase increase, and hyperuricemia. The most common (≥ 20%) Grade 3 or higher hematologic laboratory abnormalities were lymphopenia, anemia, thrombocytopenia, and neutropenia. Grade 4 hematologic abnormalities occurring in ≥ 5% were thrombocytopenia (13%), neutropenia (8%), anemia (6%), and lymphopenia (6%).

Postmarketing Experience
There is limited information regarding Midostaurin Postmarketing Experience in the drug label.
Drug Interactions
- Effect of Strong Cytochrome P450 (CYP) 3A Inhibitors and Inducers
Effect of Strong Cytochrome P450 (CYP) 3A Inhibitors and Inducers
- Table 6 lists the potential effects of the coadministration of strong CYP3A modulators on midostaurin.

Use in Specific Populations
Pregnancy
Pregnancy Exposure Registry
- There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to midostaurin during pregnancy. Females who may have been exposed to midostaurin during pregnancy directly or through a male partner receiving midostaurin therapy should contact the Novartis Pharmaceuticals Corporation at 1-888-669-6682 and/or at https://psi.novartis.com/.
Risk Summary
- Based on mechanism of action and findings in animal reproduction studies, midostaurin may cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no available data on midostaurin use in pregnant women to inform a drug-associated risk of major birth defects and miscarriage. In animal reproduction studies, oral administration of midostaurin to pregnant rats and rabbits during organogenesis caused embryo-fetal toxicities, including late embryo-fetal death and reduced fetal birth weight, with delays in fetal growth at doses lower than the recommended human dose (see Data). Advise pregnant women of the potential risk to a fetus.
- The background risk of major birth defects and miscarriage for the indicated population are unknown. Adverse outcomes in pregnancy occur regardless of the health of the mother or the use of medications. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data (Animal)
- When midostaurin was administered to female rats prior to mating and through the first week of pregnancy at a dose of 60 mg/kg/day (approximately 0.1 times the human exposure at the recommended dose based on AUC), there were increases in pre- and post-implantation loss, including total litter loss, resulting in a reduction in the number of live embryos.
- During organogenesis, midostaurin administered at oral doses greater than or equal to 3 mg/kg/day (approximately 0.004 times the human exposure at the recommended dose by AUC) to pregnant female rats caused late embryo-fetal death. Dilated lateral brain ventricles were observed in offspring of rats given doses greater than or equal to 3 mg/kg/day. Extra rib and reduced fetal birth weight with effects on fetal growth (severe renal pelvic cavitation and widened anterior fontanelle) were observed in the absence of maternal toxicity at the highest dose of 30 mg/kg/day (approximately 0.05 times the human exposure at the recommended dose by AUC). Midostaurin administered orally to pregnant rabbits during organogenesis led to maternal toxicity with spontaneous abortions and some delay in fetal growth (reduced fetal birth weight) at doses greater than or equal to 10 mg/kg/day (approximately 0.01 times the human exposure at the recommended dose by AUC).
- In an oral pre- and postnatal development study in the rat, adverse effects upon maternal performance included dams with signs of dystocia and a lower live litter size at 30 mg/kg/day (approximately 0.05 times the human exposure at the recommended dose by AUC). For the F1 offspring, lower body weights, accelerated complete eye opening and delayed auricular startle ontogeny were noted at 30 mg/kg/day.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Midostaurin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Midostaurin during labor and delivery.
Nursing Mothers
Risk Summary
- There are no data on the presence of midostaurin or its active metabolites in human milk, the effect on the breastfed infant, or the effect on milk production. Orally administered midostaurin and its active metabolites pass into the milk of lactating rats within 1 hour of a 30 mg/kg/day dose, with approximately 5 times more in the milk of lactating rats compared to plasma. Because of the potential for serious adverse reactions in breastfed infants from midostaurin advise women not to breastfeed during treatment with midostaurin and for at least 4 months after the last dose.
Pediatric Use
- Safety and effectiveness of midostaurin have not been established in pediatric patients.
Geriatic Use
- Of the 142 patients with advanced SM in clinical studies of midostaurin, 64 (45%) were aged 65 and over, and 16 (11%) were aged 75 years and over. No overall differences in safety or response rate were observed between the subjects aged 65 and over compared with younger subjects. Greater sensitivity of older individuals cannot be ruled out.
- Clinical studies in AML with midostaurin did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
- In general, administration for elderly patients should be cautious, based on patient’s eligibility for concomitant chemotherapy and reflecting the greater frequency of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Midostaurin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Midostaurin with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Midostaurin in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Midostaurin in patients with hepatic impairment.
Females of Reproductive Potential and Males
Pregnancy Testing
- Pregnancy testing is recommended for females of reproductive potential within seven days prior to initiating midostaurin.
Contraception
Females
- Midostaurin may cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment with midostaurin and for 4 months after the last dose.
Males
- Males with female sexual partners of reproductive potential should use effective contraception during midostaurin treatment and for at least 4 months after stopping treatment with midostaurin.
Infertility
- Based on findings in animals, midostaurin may impair fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible.
Immunocompromised Patients
There is no FDA guidance one the use of Midostaurin in patients who are immunocompromised.
Administration and Monitoring
Administration
Recommended Administration
- Administer prophylactic anti-emetics before treatment with midostaurin to reduce the risk of nausea and vomiting.
- Administer midostaurin orally with food, twice daily at approximately 12 hour intervals. Do not open or crush midostaurin capsules.
- If a dose of midostaurin is missed or vomited, do not make up the dose; take the next dose at the usual scheduled time.
- Consider interval assessments of QT by EKG if midostaurin is taken concurrently with medications that can prolong the QT interval.
Monitoring
- Disease response or stabilization may indicate efficacy.
- FLT3 mutation: Prior to initiation, with an FDA-approved companion diagnostic test available at http://www.fda/gov/CompanionDiagnostics.
- Pregnancy status (women of reproductive potential): Within 7 days prior to initiation of therapy.
- CBC: At least weekly for the first 4 weeks, every other week for the next 8 weeks, and monthly thereafter during therapy; include a differential.
- Toxicities, including nausea, vomiting, and other non-hematologic toxicities: At least weekly for the first 4 weeks, every other week for the next 8 weeks, and monthly thereafter during therapy.
- Pulmonary symptoms of interstitial lung disease or pneumonitis.
IV Compatibility
There is limited information regarding the compatibility of Midostaurin and IV administrations.
Overdosage
There is limited information regarding Midostaurin overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Mechanism of Action
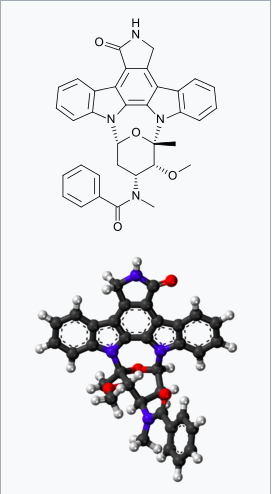
- Midostaurin is a small molecule that inhibits multiple receptor tyrosine kinases. In vitro biochemical or cellular assays have shown that midostaurin or its major human active metabolites CGP62221 and CGP52421 inhibit the activity of wild type FLT3, FLT3 mutant kinases (ITD and TKD), KIT (wild type and D816V mutant), PDGFRα/β, VEGFR2, as well as members of the serine/threonine kinase PKC (protein kinase C) family.
- Midostaurin demonstrated the ability to inhibit FLT3 receptor signaling and cell proliferation, and it induced apoptosis in leukemic cells expressing ITD and TKD mutant FLT3 receptors or overexpressing wild type FLT3 and PDGF receptors. Midostaurin also demonstrated the ability to inhibit KIT signaling, cell proliferation and histamine release and induce apoptosis in mast cells.
Structure

Pharmacodynamics
Cardiac Electrophysiology
- The effect of midostaurin (75 mg twice daily for 3 days) on the QTc interval was evaluated in a randomized, placebo and moxifloxacin controlled, multiple-dose, blinded, parallel study. There was no clinically significant prolongation of QTc interval or relationship between changes in QTc and concentrations for midostaurin and its active metabolites (CGP62221 and CGP52421). The study duration was not long enough to estimate the effects of the metabolite CGP52421 on the QT/QTc interval.
- In pooled clinical studies in patients with advanced SM, 4.7% patients had a post-baseline QTcF > 480 ms, no patients had a QTcF > 500 ms, and 6.3% patients had a QTcF > 60 ms compared to baseline.
- In a randomized placebo-controlled study in patients with AML, the proportion of patients with QTc prolongation was higher in patients randomized to midostaurin as compared to placebo (QTcF > 480 ms: 10.1% vs 5.7%; QTcF > 500 ms: 6.2% vs 2.6%; QTcF > 60 ms: 18.4% vs 10.7%).
Pharmacokinetics
- Midostaurin exhibits time-dependent pharmacokinetics with an initial increase in minimum concentrations (Cmin) that reach the highest Cmin concentrations during the first week followed by a decline to a steady-state after approximately 28 days. The pharmacokinetics of the CGP62221 showed a similar trend. The plasma concentrations of CGP52421 continued to increase after one month of treatment.
- The highest Cmin and steady-state of midostaurin, CGP62221, and CGP52421 were similar when midostaurin was administered with food at a dose of 50 mg twice daily or 100 mg twice daily.
Absorption
- The time to maximal concentrations (Tmax) occurred between 1 to 3 hours post dose in the fasted state.
Effect of Food
- Midostaurin exposure, represented by area under the curve over time to infinity (AUCinf), increased 1.2-fold when midostaurin was coadministered with a standard meal (457 calories, 50 g fat, 21 g proteins, and 18 g carbohydrates) and 1.6-fold when coadministered with a high-fat meal (1007 calories, 66 g fat, 32 g proteins, and 64 g carbohydrates) compared to when midostaurin was administered in a fasted state. Midostaurin maximum concentrations (Cmax) were reduced by 20% with a standard meal and by 27% with a high-fat meal compared to a fasted state. Tmax was delayed when midostaurin was administered with a standard meal or a high-fat meal (median Tmax = 2.5 hrs to 3 hrs).
Distribution
- Midostaurin has an estimated geometric mean volume of distribution (% coefficient of variation) of 95.2 L (31%). Midostaurin and its metabolites are distributed mainly in plasma in vitro. Midostaurin, CGP62221, and CGP52421 are greater than 99.8% bound to plasma protein in vitro. Midostaurin is mainly bound to α1-acid glycoprotein in vitro.
Elimination
- The geometric mean terminal half-life (% coefficient of variation) is 19 hours (39%) for midostaurin, 32 hours (31%) for CGP62221 and 482 hours (25%) for CGP52421.
Metabolism
- Midostaurin is primarily metabolized by CYP3A4. CGP62221 and CGP52421 (mean ± standard deviation) account for 28 ± 2.7% and 38 ± 6.6% respectively of the total circulating radioactivity.
Excretion
- Fecal excretion accounted for 95% of the recovered dose with 91% of the recovered dose excreted as metabolites and 4% of the recovered dose as unchanged midostaurin. Only 5% of the recovered dose was found in urine.
Specific Populations
- Age (20-94 years), sex, race, and mild (total bilirubin greater than 1.0 to 1.5 times the upper limit of normal (ULN) or aspartate aminotransferase (AST) greater than the ULN) or moderate (total bilirubin 1.5 to 3.0 times the ULN and any value for AST) hepatic impairment or renal impairment (creatinine clearance (CLCr) ≥ 30 mL/min) did not have clinically meaningful effects on the pharmacokinetics of midostaurin, CGP62221, or CGP52421. The pharmacokinetics of midostaurin in patients with baseline severe hepatic impairment (total bilirubin greater than 3.0 times the ULN and any value for AST) or severe renal impairment (CLCr 15 to 29 mL/min) is unknown.
Drug Interaction Studies
Clinical Studies
Effect of Strong CYP3A4 Inhibitors on Midostaurin
- Coadministration of ketoconazole (400 mg daily for 10 days) with a single dose of midostaurin (50 mg) on Day 6 increased AUCinf of midostaurin by 10.4-fold and CGP62221 by 3.5-fold and area under the curve over time to last measurable concentrations (AUC0-t) of CGP52421 by 1.2-fold compared to a single midostaurin dose coadministered with placebo.
- Coadministration of itraconazole (100 mg twice daily on Days 22-28 for 13 doses) with multiple doses of midostaurin (100 mg twice daily on Days 1 to 2 and 50 mg twice daily on Days 3 to 28) increased Day 28 Cmin concentrations of midostaurin by 2.1-fold, CGP62221 by 1.2-fold, and CGP52421 by 1.3-fold compared to the respective Day 21 Cmin concentrations with midostaurin alone.
Effect of Strong CYP3A4 Inducers on Midostaurin
- Coadministration of rifampicin (600 mg daily on Days 1 to 14) with a single dose of midostaurin (50 mg) on Day 9 decreased AUCinf of midostaurin by 96% and CGP62221 by 92% and AUC0-t of CGP52421 by 59%.
Effect of Midostaurin on Sensitive CYP3A substrates
- Midazolam (sensitive CYP3A substrate) AUCinf was not affected following 4 days of midostaurin administration. The clinical relevance of this interaction is unknown as the midostaurin was administered for only 4 days.
In Vitro Studies
Effects of Midostaurin on CYP Enzymes
- Midostaurin inhibits CYP1A2, CYP2C8, CYP2C9, CYP2D6, CYP2E1 and CYP3A; CGP62221 inhibits CYP1A2, CYP2C8, CYP2C9, and CYP3A; and CGP52421 inhibits CYP2D6 and CYP3A in vitro. Midostaurin, CGP52421, and CGP62221 induce CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP3A in vitro.
Effects of Midostaurin on Transporters
- Midostaurin inhibits P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP); CGP52421 and CGP62221 inhibit organic anion transporter polypeptide (OATP) 1B1 in vitro.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies have not been performed with midostaurin.
- Midostaurin was not mutagenic in vitro in the bacterial reverse mutation assay (Ames test) or in Chinese hamster V97 cells. Midostaurin increased the frequency of polyploidy cells in an in vitro chromosomal aberrations assay in Chinese hamster ovary cells, but was not clastogenic in an in vivo rat bone marrow micronucleus assay when tested to the maximum tolerated dose (MTD) of 200 mg/kg (1200 mg/m2). This dose was approximately 20-fold the recommended human dose, based on body surface area.
- Reproductive toxicity was observed in a fertility study, in male and females rats given oral doses of midostaurin at 10, 30 and 60 mg/kg/day (approximately 0.01, 0.05, and 0.1 times, respectively, the AUC at the recommended human dose). In males, testicular degeneration and atrophy was observed at doses greater than or equal to 10 mg/kg/day and reduced sperm count and motility, and a decrease in reproductive organ weights were observed at 60 mg/kg/day. In females, increased resorptions, decreased pregnancy rate, and decreased number of implants and live embryos were observed at 60 mg/kg/day. In a 3-month toxicology study in dogs, there was inhibition of spermatogenesis at doses greater than or equal to 3 mg/kg/day (approximately 0.01 times the exposure at the recommended human dose).
Clinical Studies
Acute Myeloid Leukemia
Study 1
- Midostaurin in combination with chemotherapy was investigated in a randomized, double-blind placebo-controlled trial of 717 patients with newly-diagnosed FLT3-mutated AML. In this study, FLT3 mutation status was determined prospectively with a clinical trial assay and verified retrospectively using the companion diagnostic LeukoStrat® CDx FLT3 Mutation Assay, which is an FDA-approved test for selection of patients with AML for midostaurin treatment. Patients were stratified by FLT3 mutation status: TKD, ITD with allelic ratio less than 0.7, and ITD with allelic ratio greater than or equal to 0.7. Patients with acute promyelocytic leukemia or therapy-related AML were not eligible. Patients were randomized (1:1) to receive midostaurin 50 mg twice daily (n = 360) or placebo (n = 357) with food on Days 8-21 in combination with daunorubicin (60 mg/m2 daily on Days 1 to 3) /cytarabine (200 mg/m2 daily on Days 1 to 7) for up to two cycles of induction and high dose cytarabine (3 g/m2 every 12 hours on Days 1, 3 and 5) for up to four cycles of consolidation, followed by continuous midostaurin or placebo treatment according to initial assignment for up to 12 additional 28-day cycles. There was no re-randomization at the start of post consolidation therapy. Patients who proceeded to hematopoietic stem cell transplantation (SCT) stopped receiving study treatment.
- The randomized patients had a median age of 47 years (range, 18-60 years), 44% were male, and 88% had a performance status of 0-1. AML was de novo onset in 95%. The percentage of patients with FLT3-ITD allelic ratio < 0.7, FLT3-ITD allelic ratio ≥ 0.7, and FLT3-TKD mutations were identical (per randomized FLT3 stratum) on both arms (48%, 30%, and 23%, respectively). Of the 563 patients with NPM1 testing, 58% had an NPM1 mutation. The two treatment groups were generally balanced with respect to the baseline demographics and disease characteristics, except that the placebo arm had a higher percentage of females (59%) than in the midostaurin arm (52%). NPM1 mutations were identified in 55% of patients tested on the midostaurin arm and 60% of patients tested on the placebo arm.
- A second course of induction was administered to 25% of the patients, 62% initiated at least one cycle of consolidation, 29% initiated maintenance, and 17% completed all 12 planned cycles of maintenance; 21% of the patients underwent SCT in first CR. The overall rate of SCT (induction failure, first CR or salvage after relapse) was 59% (214/360) of patients in the midostaurin plus standard chemotherapy arm vs. 55% (197/357) in the placebo plus standard chemotherapy arm. All patients were followed for survival.
- Efficacy was established on the basis of overall survival (OS), measured from the date of randomization until death by any cause. The primary analysis was conducted after a minimum follow-up of approximately 3.5 years after the randomization of the last patient. Midostaurin plus standard chemotherapy was superior to placebo plus standard chemotherapy in OS (HR 0.77; 95% CI 0.63, 0.95; 2 sided p = 0.016) (Figure 1). Because survival curves plateaued before reaching the median, median survival could not be reliably estimated.

- The analysis of event-free survival (EFS), defined as a failure to obtain a complete remission (CR) within 60 days of initiation of protocol therapy, or relapse, or death from any cause, showed a statistically significant improvement with a median of 8.2 months for midostaurin plus standard chemotherapy versus 3.0 months for placebo plus standard chemotherapy with HR 0.78 (95% CI 0.66, 0.93) and 2 sided p = 0.005. In an exploratory analysis of EFS defined as a failure to obtain a CR any time during induction, or relapse, or death from any cause with failures assigned as an event on study day 1, the median EFS was 10.6 months for midostaurin plus standard chemotherapy versus 5.6 months for placebo plus standard chemotherapy with HR 0.72 (95% CI 0.61, 0.86).
Systemic Mastocytosis
Study 2
- A single-arm, open-label, multicenter trial evaluated the efficacy of midostaurin as a single agent in ASM, SM-AHN, and MCL, collectively referred to as advanced SM. The study enrolled 116 adult patients with relapse or progression to 0, 1, or 2 prior regimens for SM. The study excluded patients with serum creatinine > 2.0 mg/dL, hepatic transaminases > 2.5 x upper limit of normal (ULN) or > 5 x ULN if disease-related, total bilirubin > 1.5 x ULN or > 3 x ULN if disease-related, QTc > 450 msec, cardiovascular disease including left-ventricular ejection fraction < 50%, or any pulmonary infiltrates. In addition, the study excluded patients with acute-stage or life-threatening AHN. Patients received midostaurin 100 mg orally twice daily in 28-day cycles until disease progression or intolerable toxicity.
- Of the 116 patients treated, a study steering committee identified 89 patients who had measurable C-findings and were evaluable for response. The median age in this group was 64 years (range: 25 to 82), 64% of patients were male, and nearly all patients (97%) were Caucasian. Among these patients, 36% had prior therapy for SM, and 82% had the KIT D816V mutation detected at baseline. Their median duration of treatment was 11 months (range: < 1 to 68 months), with treatment ongoing in 17%.
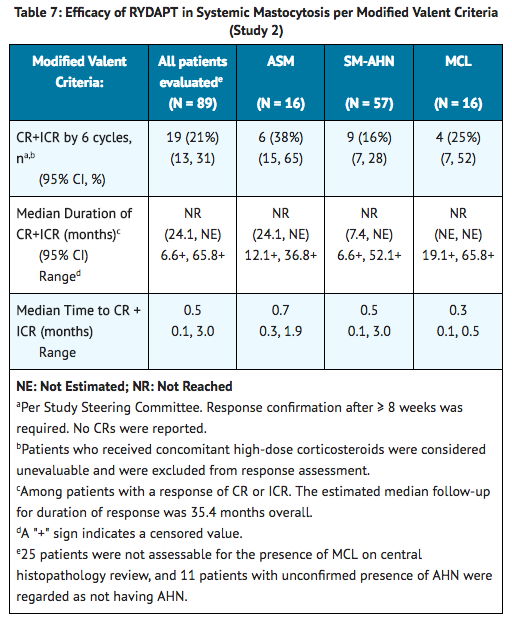
- Efficacy was established on the basis of confirmed complete remission (CR) plus incomplete remission (ICR) by 6 cycles of midostaurin by modified Valent criteria for ASM and SM-AHN (Table 7). Table 7 shows responses to midostaurin according to modified Valent criteria. Confirmed major or partial responses occurred in 46 of 73 patients with a documented KIT D816V mutation, 7 of 16 with wild-type or unknown status with respect to KIT D816V mutation, and 21 of 32 having prior therapy for SM.
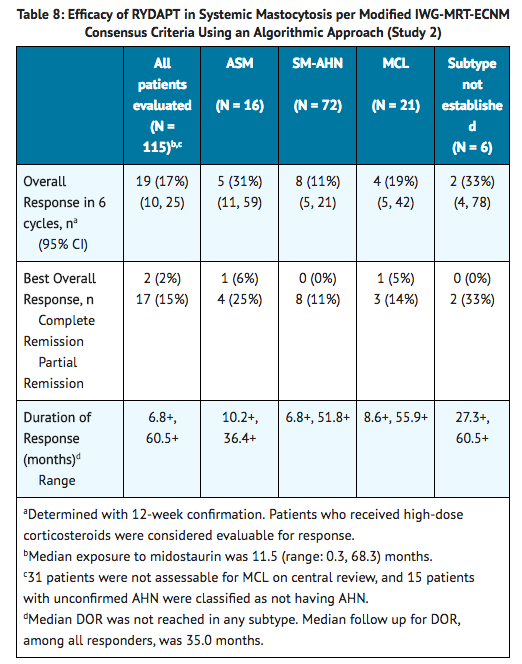
- As a post-hoc exploratory analysis, efficacy was also assessed using modified 2013 International Working Group-Myeloproliferative Neoplasms Research and Treatment-European Competence Network on Mastocytosis (IWG-MRT-ECNM) consensus criteria. Response after 6 cycles of midostaurin was determined using a computational algorithm. The efficacy of midostaurin for MCL was based on the CR results by these criteria. There were 115 patients evaluable for response assessment, of whom 47 (41%) had prior therapy for SM, and 93 (81%) had a documented D816V mutation at baseline. Table 8 provides the results of this analysis. Overall response by modified IWG-MRT-ECNM criteria was reported for 16 (17%) of 93 patients with a documented D816V mutation, and in 8 (17%) of 47 patients having prior therapy for SM.
Study 3
- Study 3 was a single-arm, multicenter, open-label trial of 26 patients with advanced SM. Midostaurin was administered orally at 100 mg twice daily with food. The median age in this group was 64 years, 58% of patients were male and most were Caucasian (81%). Eligibility criteria were similar to Study 2. By Valent criteria per investigator assessment, of 17 patients with SM-AHN, 10 achieved a response (1 partial, 9 major) by 2 cycles that was sustained for at least 8 weeks. Patients who received concomitant corticosteroids were included. Of the 6 patients with MCL, 1 achieved partial response and 1 achieved major response. Median DOR for either group had not been reached, with DOR ranging from 3.4+ to 79.2+ months in patients with SM-AHN and 28.6+ to 32.1+ months in patients with MCL. The subtype of SM in the remaining 3 patients was unconfirmed.
How Supplied
- Midostaurin 25 mg capsules
- Pale orange oblong soft capsule with red ink imprint ‘PKC NVR’; available in:
- 56 soft capsules………………………………………………………………………………………NDC 0078-0698-99
- Contents: Each carton contains two inner packs, each with 28 capsules (7 blister cards with 4 capsules each)
- 112 soft capsules……………………………………………………………………………………..NDC 0078-0698-19
- Contents: Each carton contains four inner packs, each with 28 capsules (7 blister cards with 4 capsules each)
Storage
- Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Store in the original package to protect from moisture.
Images
Drug Images
{{#ask: Page Name::Midostaurin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Midostaurin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling (Patient Information).
- Pulmonary Adverse Reactions: Inform patients to seek medical attention for new cough, chest discomfort, or shortness of breath.
- Gastrointestinal Adverse Reactions: Inform patients that midostaurin can cause nausea, vomiting, and diarrhea. Advise patients to contact their healthcare provider if these symptoms occur or are persisting despite supportive medications.
- Embryo-Fetal Toxicity
- Advise pregnant women and females of reproductive potential of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with midostaurin and for at least 4 months after the last dose. Advise females to inform their healthcare provider of a known or suspected pregnancy.
- Advise male patients with female partners of reproductive potential to use effective contraception during treatment with midostaurin and for 4 months after the last dose.
- Advise females who may have been exposed to midostaurin during pregnancy directly or through male partner receiving midostaurin therapy to contact the Novartis Pharmaceuticals Corporation at 1-888-669-6682 and /or at https://psi.novartis.com/.
- Lactation
- Advise women not to breastfeed during treatment with midostaurin and for at least 4 months after the final dose.
- Infertility
- Advise females and males of reproductive potential that midostaurin may impair fertility.

Precautions with Alcohol
Alcohol-Midostaurin interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Rydapt
Look-Alike Drug Names
There is limited information regarding Midostaurin Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.