Microsporidiosis pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ogheneochuko Ajari, MB.BS, MS [2] Ahmed Younes M.B.B.CH [3]
|
Microsporidiosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Microsporidiosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Microsporidiosis pathophysiology |
|
Risk calculators and risk factors for Microsporidiosis pathophysiology |
Overview
Microsporidia are a group of obligate intracellular protozoa with more than 1,200 species belonging to 143 genera that infect a wide range of vertebrate and invertebrate hosts. They are characterized by the production of resistant spores that vary in size, depending on the species. After ingestion, it infects intestinal epithelial cells and causes chronic diarrhea with the possibility of distant spread. The microorganism can be visualized in stool samples using "Quick-Hot Gram Chromotrope technique".
Pathophysiology
Life Cycle
The infective form of microsporidia is the resistant spore and it can survive for an extended period of time in the environment.[1]
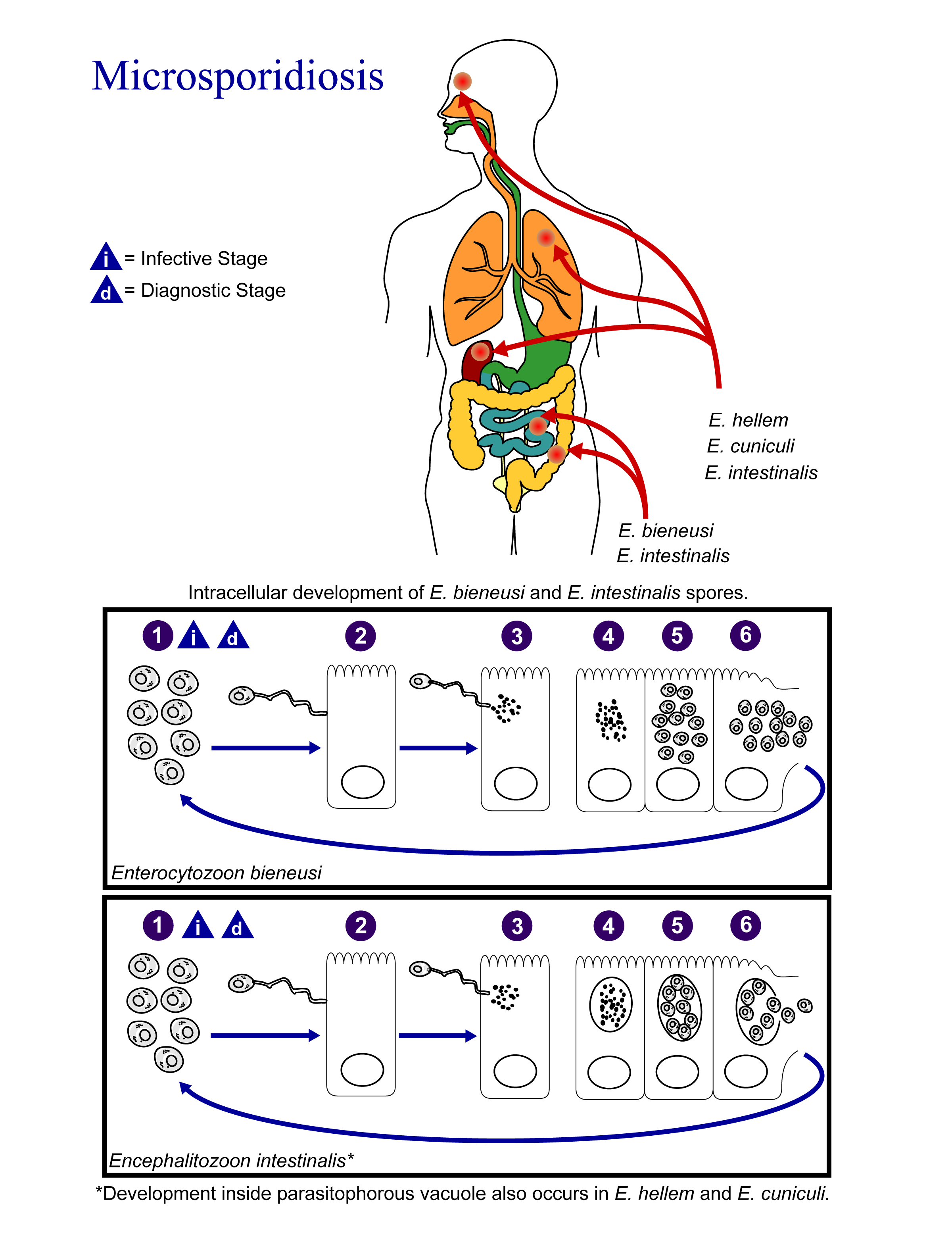 |
- The spores enter the body via ingestion or inhalation.
- Spores penetrate host cell using its polar tubule.
- The spore uses its polar tubule for injecting its sarcoplasm into the infected cell.
- The sarcoplasm multiplies either by binary fission or multiple fission
- The sarcoplasm of microsporidia develops into mature spores either free in the cytoplasm or inside a vacuole.
- The process of development involves acquiring a thick capsule. This capsule provides protection against environmental stressors and is thought to play a role in its infectivity.
- After their number reaches a certain limit, the host cell ruptures releasing the spores to continue the life cycle.
Pathogenesis
- Microsporidia cause distortion of the villi without profound inflammatory findings.[2][3]
- With the progression of the disease, the microsporidia interfere with the intestinal absorption causing various symptoms of malabsorption (weight loss, chronic diarrhea, and vitamin deficiencies).
- Disseminated disease can cause symptoms in the biliary tract, respiratory system, the urinary tract or the eye.
Microscopic pathology
- Intestinal biopsy shows crypt hyperplasia and decreases in the absorptive surface of the intestine.[2]
- Stool examination using “Quick-Hot Gram Chromotrope technique” reveals the spores staining dark violet and containing gram-positive granules.
- Enterocytozoon bieneusi spores measure 0.8 - 1.4 µm while spores of Anncaliia algerae, Encephalitozoon spp., Vittaforma corneae, and Nosema spp measure 1.5 - 4 µm.
-
Sporoblast of the Microsporidium Fibrillanosema crangonycis - By No machine-readable author provided. Javier martin assumed (based on copyright claims). - No machine-readable source provided. Own work assumed (based on copyright claims)., CC BY 2.5, https://commons.wikimedia.org/w/index.php?curid=919796
-
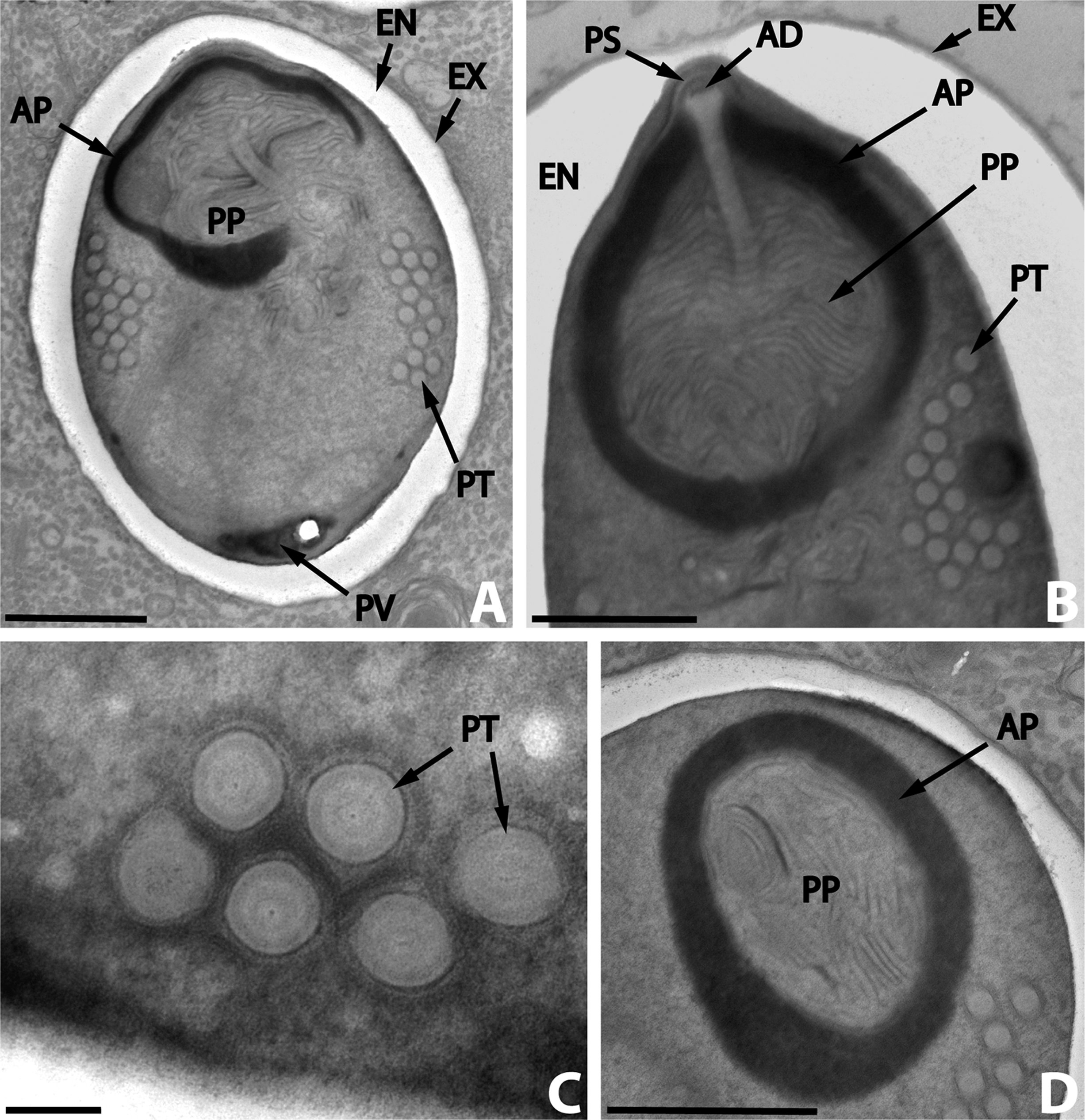
Dictyocoela diporeiae.A, meront and spore; B, spore wall; C, polar filament - By Andrew David Winters & Mohamed Faisal - Winters, A. D., Faisal, M. 2014. Molecular and ultrastructural characterization of Dictyocoela diporeiae n. sp. (Microsporidia), a parasite of Diporeia spp. (Amphipoda, Gammaridea). Parasite, 21, 26 doi:10.1051/parasite/2014028, CC BY 2.0, https://commons.wikimedia.org/w/index.php?curid=33448743
-
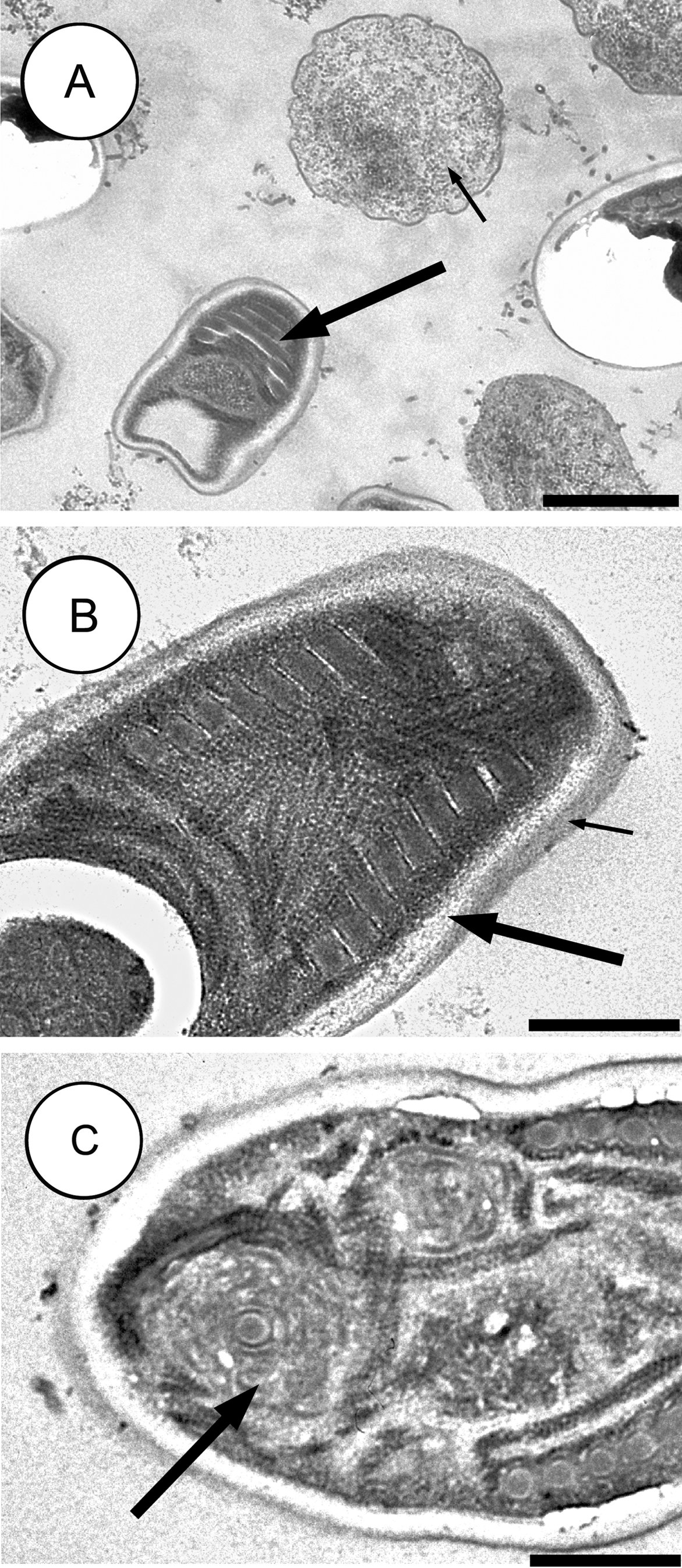
A hyperparasitic microsporidian, Nosema podocotyloidis - By Bhen Sikina Toguebaye, Yann Quilichini, Papa Mbagnick Diagne and Bernard Marchand - Toguebaye, B. S., Quilichini, Y., Diagne, P. M. & Marchand, B. 2014: Ultrastructure and development of Nosema podocotyloidis n. sp. (Microsporidia), a hyperparasite of Podocotyloides magnatestis (Trematoda), a parasite of Parapristipoma octolineatum (Teleostei). Parasite, 21, 44. doi:10.1051/parasite/2014044, CC BY 2.0, https://commons.wikimedia.org/w/index.php?curid=35088476
References
- ↑ "CDC - DPDx - Microsporidiosis".
- ↑ 2.0 2.1 Franzen C, Müller A (2001). "Microsporidiosis: human diseases and diagnosis". Microbes Infect. 3 (5): 389–400. PMID 11369276.
- ↑ Weber R, Bryan RT, Schwartz DA, Owen RL (1994). "Human microsporidial infections". Clin. Microbiol. Rev. 7 (4): 426–61. PMC 358336. PMID 7834600.